Risk factors for death among children with severe malaria, Namutumba District, Eastern Uganda, September 2021 – February 2022
Authors: Marie Gorreti Zalwango1*, Brenda Simbwa1, Zainah Kabami1, Peter Chris Kawungezi1, Mercy Wanyana1, Rebecca Akunzirwe1, Jane Frances Zalwango1, Saudah Namubiru Kizito1, Oonyu Lawrence1, Hellen Nelly Naiga1, Mackline Ninsiima1, Brian Agaba1, Robert Zavuga1, Patrick King1, Thomas Kiggundu1, James Kiirya2, Jeremiah Gambaniro2, Richard Migisha1, Daniel Kadobera1, Benon Kwesiga1, Lilian Bulaga1, Alex Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Namutumba District Local Government, Namutumba, Uganda *Correspondence: Email: mzalwango@musph.ac.ug, Tel: +256752610802
Summary Background: On February 17, 2022, a “strange disease', which was later confirmed as malaria, was reported to the Ministry of Health from Namutumba District, mainly affecting children and reportedly causing large numbers of child deaths since late 2021. We investigated to determine the scope of severe malaria deaths, identify factors associated, and recommend evidence-based control measures to inform proper programming for the prevention of malaria-associated deaths among children in Namutumba District. Methods: We conducted an unmatched case-control study in March 2022 in Ivukula Subcounty. This subcounty had the highest attack rate per 1,000 population in the district. We defined a case as death with a history of fever AND any of the following: convulsions, difficulty in breathing, yellowing of eye or palms, tea-colored urine, anemia, loss of consciousness, or reduced urine output in a child ≤12 years from September 2021 to February 2022 in Ivukula Subcounty, Namutumba District. A control was defined as a severe malaria survivor. We actively searched for cases and controls with the help of VHTs in a ratio of 1:2 controls. A semi-structured interviewer-administered questionnaire was used to obtain demographic data and assess clinical, health-seeking, and health system risk factors. Drugs and bloodstock status information was obtained from health workers using semi-structured interviews. We identified risk factors for death using multivariate logistic regression and thematic analysis for qualitative data. Results: We identified 46 cases and 77 controls. Among the 46 cases, 63% were <5 years, with 1:1 ratio for males and females. Death among children with severe malaria was significantly associated with treatment non-completion (aOR=9.7, 95%CI:1.8 – 52.9) and failure to receive blood transfusion for anemic patients (aOR=7.1, (95%CI: 1.4 – 36.2). Other findings that hindered access to effective care and treatment included failure to reach intended referral sites due to transport cost challenges, stockouts of antimalarials and blood products, and absence of integrated community case management of childhood illnesses (iCCM). Conclusion: Failure to complete antimalarial treatment, not receiving blood transfusion for anemic patients, stockouts of malaria drugs, and failure to reach referral sites were major contributors to malaria mortality among children ≤12 years in Ivukula Subcounty, Namutumba District. We recommend a more accurate quantification of antimalarials for health facilities, offering transport support to severe patients referred to higher-level facilitiesincreasing access to blood products and activation of iCCM to avert numerous deaths among children in this area.
Introduction
Globally, the scale-up of malaria prevention and control measures has made a significant contribution to the fight against malaria, with notable gains between 2000 and 2020 resulting in a 36% reduction in mortality[1].
Despite this decrease, the number of malaria-related deaths remains high, reaching 627,000 in 2020 as a result of the 241 million cases reported that year, with the World Health Organization (WHO) African Region bearing the highest burden[2].
In Uganda, malaria is still highly endemic in 95% of the country, with the remaining 5% prone to epidemics. The disease is one of the leading causes of morbidity and mortality in the country, responsible for 30-50% of outpatient visits and 15-20% of hospital admissions[3].
With such a heavy burden, the risk of death is high if not managed promptly and effectively. True to this, Uganda, which ranked third with a 5% contribution of all global malaria cases in 2020, accounted for 3.5% of all reported deaths in the same year, ranking fifth in this regard[2].
We would expect Uganda’s contribution to global deaths to be minimal with the current implementation of prompt and effective diagnosis and treatment of cases combined with other malaria control interventions such as the nationwide distribution of long-lasting insecticide-treated bed nets (LLINs) and indoor residual spraying (IRS). On the contrary, Uganda still registers approximately 20-30 deaths per week due to severe malaria according to the National Health Information System[4].
According to the Uganda National Malaria Control Program (NMCP), severe malaria is defined as malaria complicated by serious organ failures or abnormalities in the patient’s blood or metabolism.
The manifestations of severe malaria may include cerebral malaria (impairment of consciousness), severe anaemia, hemoglobinuria, acute respiratory distress syndrome, abnormalities in blood coagulation, low blood pressure caused by cardiovascular collapse, acute kidney injury, hyper-parasitemia, and metabolic acidosis.
Severe malaria is a medical emergency and should be treated urgently and aggressively using 3 doses of intravenous artesunate in 24 hours followed by a complete dose of artemether and lumefantrine (AL) for 3 days[5].
On February 17, 2022, a Member of Parliament in Busiki County, Namutumba District reported to the Uganda Ministry of Health (UMoH) about a ‘strange disease’, mainly affecting children. The condition was reportedly presenting as fever, anemia, urinating and coughing blood, and death, mostly among children 12 years of age and below and on investigation the disease was identified to be severe malaria. We investigated to determine the scope of severe malaria deaths, identify factors associated, and recommend evidence-based control measures.
Methods
Outbreak area
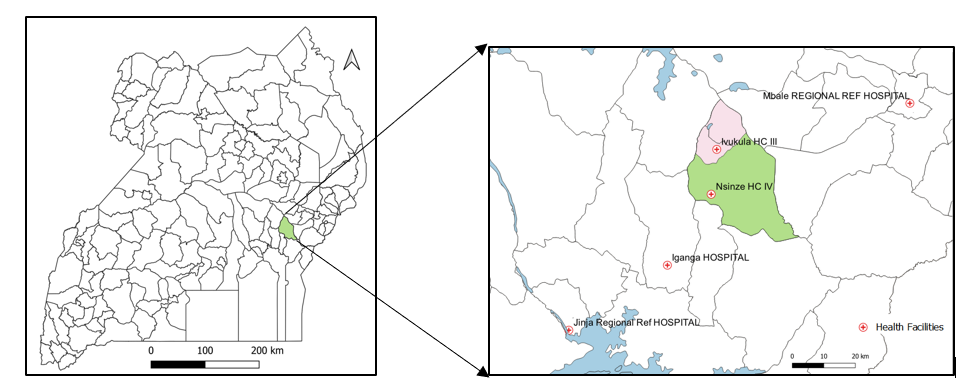
Namutumba District is located in the eastern part of Uganda, a region highly burdened with malaria. The district is made up of 2 constituencies and 20 sub-counties with a total population of approximately 320,000 people[6]. The population is served by 2 private hospitals, 1 Health center (H/C) IV, 7 H/C IIIs, and 25 H/C IIs.
Only H/C IIIs are mandated to manage severe malaria while blood transfusion services are offered at the HC IV in the district; these products are received from Jinja Regional Referral Hospital on request and supply is not guaranteed.
For further management beyond Nsinze H/C IV, referrals are made to Iganga Hospital, Jinja Regional Referral Hospital or Mbale Reginal Referral Hospital which are 31Km, 71Km and 79Km respectively away from Nsinze H/C IV.
Case definition and finding
We defined a case as fatal fever and any of the following: convulsions, difficulty in breathing, yellowing of eye or palms, tea-colored urine, anemia (subjective or clinically-identified), loss of consciousness, or reduced urine output child ≤12 years from September 2021 to February 2022 in Ivukula Sub-county.
We chose to use clinical definitions and relied on the caretakers’ memory to remember the child’s presentation. For case-patients, majority of the caregivers had discarded the records immediately after the loss of their child or were not provided with the records at facilities
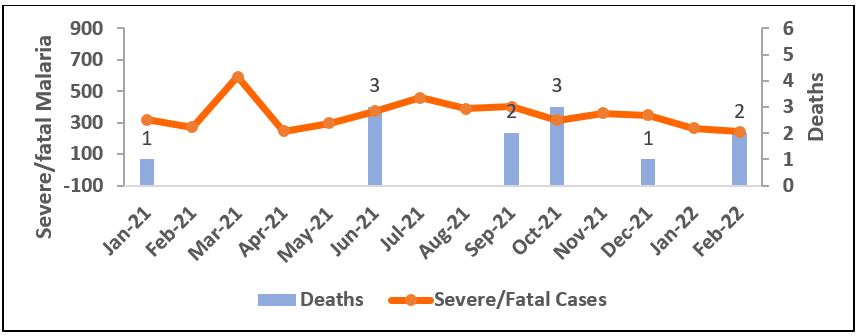
To find and ascertain the scope of severe malaria deaths in the district, we reviewed data on severe malaria and fatal malaria cases in the district health information system (DHIS2). This was followed by review of records from inpatient registers from all public and private health facilities in Namutumba District. Unfortunately, these data sources could not support the alleged increase in deaths among children (Figure 2).
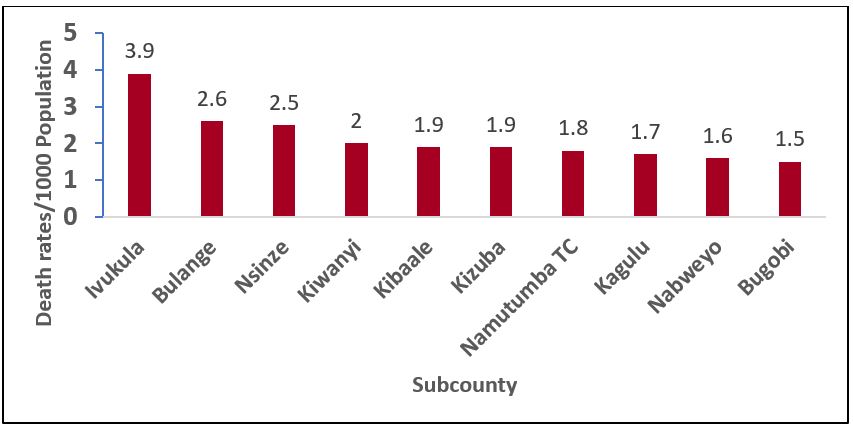
We then hypothesized that the deaths could be happening in the community. We conducted semi-structured interviews with all Village Health Teams (VHTs) to ascertain the presence of community deaths. All VHTs from 640 villages of Namutumba District were contacted through phone call interviews to obtain the number of all deaths among children ≤12 years that occurred in the communities from September 2021 to February 2022, regardless of the cause. We calculated subcounty death rates among children ≤12 years using total population as a denominator, due to lack of age-specific population data (Figure 3).
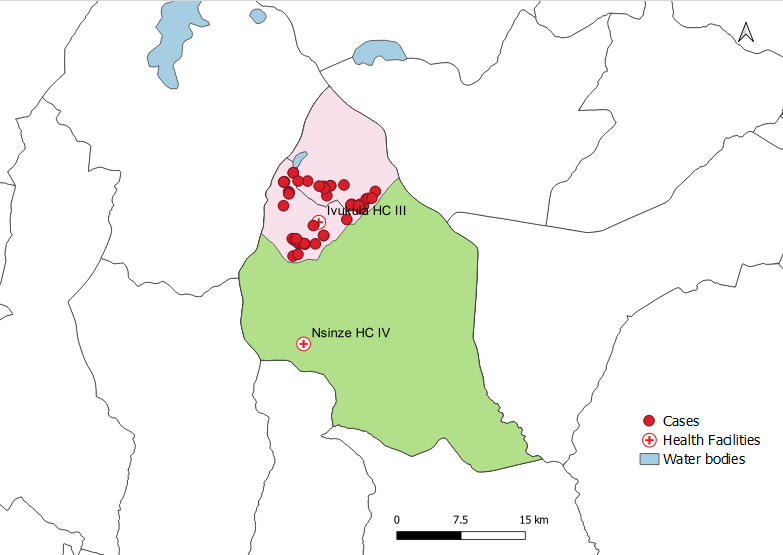
We then focused our case finding based on the case definition to Ivukula Subcounty since it had the highest attack rates. We conducted active case search in the villages of Ivukula Subcounty and line listed the cases.
Descriptive epidemiology
We calculated the median age, sex ratio, and made a geographical presentation of cases based on their homestead location. For the time factor, we constricted an epi curve to determine the period when the deaths increased.
Hypothesis generation
On addition to the descriptive epidemiology from the line lists, we conducted key Informant interviews with the VHTs, health facility in charges, and health facility staff to identify factors that might be associated with malaria deaths to support hypothesis generation. 10 KII were conducted (2 health facility in charges, 4 health facility staff, and 4 VHTs. We also assessed stock details for facilities (2 H/C IIs and 1 H/C III) in Ivukula Subcounty from September 2021 to February 2022 to identify any antimalaria stock challenges if any.
Case control study
We conducted an unmatched case-control study in Ivukula Subcounty, the most affected subcounty in the district to identify risk factors for deaths among children with severe malaria. Exposures assessed included child and caregiver demographic factors, child clinical factors, care-seeking practices, delays to care, care provided at facilities, adherence to care, and history of severe malaria.
A control was non-fatal fever AND any of the following: convulsions, difficulty in breathing, yellowing of the eyes and palms, tea-colored urine, anaemia, loss of consciousness or reduced urine output in a child <12 years from September 2021 to February 2022 in Ivukula Sub-county.
Controls were selected from the same parish as the cases in a ratio of 2:1. All children suffering from severe malaria at the time of the investigation were excluded since they still had the possibility of turning into cases. Furthermore, for homesteads with more than one case or control, only one case was considered to avoid collinearity.
A semi-structured questionnaire was constructed in Epi-info 7 and administered using electronic forms or, when not available, paper-based forms which were entered into the database manually each evening. Data were cleaned and analyzed using Epi-info version 7.2.5.0 software. Univariant analysis and multivariant analysis using logistic regression was done to determine levels of association.
First, crude odds ratios, 95% confidence interval (CI) and their respective p-values were obtained. All variables with p-values <0.05 were considered for multivariable analysis except for variables that were collinear. Multivariable logistic regression was conducted to obtain adjusted odds ratios with their respective 95% confidence interval (CI) and p-values. Variables with p-values <0.05 at multivariable analysis were considered to be significant and associated with the outcome.
Ethical considerations
This investigation was in response to a public health emergency and was therefore determined to be non-research. The MoH gave the directive to investigate this outbreak.
The Office of the Associate Director for Science, CDC/Uganda, also determined that this activity was not human subject research, and its primary intent was public health practice or a disease control activity (specifically, epidemic or endemic disease control activity).
Written informed consent in English and the local language was sought from respondents or care-takers of diseased children. They were informed that their participation was voluntary and their refusal would not result in any negative consequences. To protect the confidentiality of the respondents, each was assigned a unique identifier which was used instead of their names.
Results
Descriptive epidemiology
We identified 61 deaths among children ≤12years of which 51 were due to severe malaria while 10 were from other causes (neonatal deaths (5), unknown cause (2), anaemia without fever (1), convulsions without fever (1) and severe pneumonia (1).
Among the cases with severe malaria (51), 63% were below 5 years while 37% were older than 5 years. The median age was 4years, IQR (2-6) while 51% were male. Distribution of parishes with the highest number of deaths were: Nabitula (15; 29%), Kirongo (14; 27%), Kisewozi (9;18%), Budomero (7;14%), Kimenyulo (3;6%), Namukode (2; 4%) and Ivukula (1; 2%).
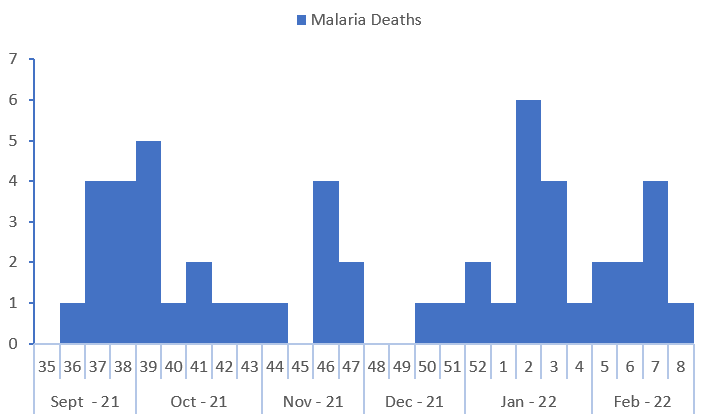
The highest number of child deaths in Ivukula Subcounty was recorded in September 2021 and January 2022 (Figure 4).
Hypothesis generation findings
From the caregiver interviews and KII from the health workers and VHTs, frequent drug stockouts were the most commonly-reported severe malaria deaths associated concern.
All health facilities assessed for stock status reported having received stock twice in the assessed 6 months (Table 1). The HCIII had received 200 doses of artesunate which was completely used up in 14 days. During periods of reduced stock of artesunate, patients are given the starter dose and advised to buy the rest. However, community members and healthcare workers noted that this often does not happen.
“During periods of reduced stock of artesunate, patients are given only the start dose and are advised to buy the rest but this does not happen to finance challenges….” A narration from one of the health workers at a HC III.
Table 1: Antimalaria quantities delivered and their consumption period for facilities in Ivukula Subcounty, Namutumba District
| Facility | Artemether-lumefantrine packs received per cycle (30 doses/pack) | AL stock duration (days) | Artesunate doses received | Artesunate stock duration (days) |
| Lwatama H/C II | 34 | 21 | — | — |
| Namasita H/C II | 10 | 45 | — | — |
| Ivukula H/C III | 60 | 21 | 200 | 14 |
Other related factors included failure to receive blood products in severely anemic patients, failure to reach the high-level health facilities when referred due to economic constraints. One VHT revealed that; “caretakers often go home with very sick children and wait until transport money is acquired, hence children die from home or during transportation to the health facilities….”
Regarding blood products stock, the HC IV in-charge reported challenges in transport to pick blood products from Jinja regional referral hospital and on some occasions when transport is available, the stock at the regional referral is not available.
We hypothesized that either age and sex of the child, care giver status and education level, the duration to seek care, the health facility visited, availability of drugs and blood products and completeness of referral were contributing to the death of children below 12 years in Ivukula Subcounty, Namutumba District.
Case control study findings
A total of 46 cases and 77 controls were used for the case control study, 5 of the 51 cases were excluded from the case control study since they were from the same homestead as the other cases for collinearity concerns. Cases were not different from controls in age, 63% cases and 52% controls were below 5 years (p= 0.23). Similar proportions of cases (50%) and controls (53%) were females (p=0.73). Caregivers were older for cases than controls (median age 42 vs 35 years, p=0.01) and generally had lower levels of education (54% vs 35% with none or lower primary education, p=0.1) (Table 2).
Anemia was more common among cases than controls (85% vs 44%, p=0.002), as was jaundice (80% vs 58%, p=0.01), while convulsions were more common among controls than cases (53% vs 35%, p=0.06). Experiencing tea-colored urine was more common among cases than controls (61% vs 43%, p=0.05). Cases were more likely to need blood transfusion 58% compared to 32% among controls (p=<0.001) and were less likely to receive blood transfusion, cases 41% compared to 82% among controls (p=<0.001). Together, these suggest that cases might have been sicker than controls. (Table 2).
|
Characteristic |
Cases (N=46)
n (%) |
Controls (N=77)
n (%) |
COR (95% CI) |
AOR (95% CI) |
| Child characteristics | ||||
| Age in years
<5 ≥5 Median age (years) |
29 (63) 17 (37) 3.5 |
40 (52) 37 (48) 4.5 |
Ref 0.6 (0.3 – 1.4) NA |
Ref 0.5 (0.1 -2.8) |
| Sex
Female Male |
23 (50) 23 (50) |
41 (53) 36 (47) |
Ref 1.1 (0.5-2.3) |
Ref 0.8 (0.2 – 3.9) |
| Clinical Characteristics | ||||
| Anaemia (pale palms and eyes)
No Yes |
7 (15) 39 (85) |
43 (56) 34 (44) |
Ref 4.5 (1.8 – 11.3) *** |
– |
| Convulsions
No Yes |
30 (65) 16 (35) |
36 (47) 41 (53) |
Ref 0.5 (0.22 – 1.0) |
–
|
| Difficulty in breathing
No Yes |
22 (48) 24 (52) |
29 (38) 48 (62) |
Ref 0.6 (0.3 – 1.4) |
– |
| Jaundice
No Yes |
9 (20) 37 (80) |
32 (42) 45 (58) |
Ref 2.9 (1.2 – 6.9) * |
– |
| Loss of consciousness
No Yes |
33 (72) 13 (28) |
64 (83) 13 (17) |
Ref 1.9 (0.8 – 4.6) |
– |
| Tea colored Urine
No Yes |
18 (39) 28 (61) |
44 (57) 33 (43) |
Ref 2.1 (0.99 – 4.4) |
|
| Needed blood transfusion
No Yes |
16 (42) 22 (58) |
47 (68) 22 (32) |
Ref 2.9 (1.3 – 6.7) *** |
– |
| Received blood transfusion
Yes |
9 (41) 13 (59) |
18 (82) 4 (18) |
Ref 6.5 (1.6 – 25.8) ** |
Ref 7.1 (1.4 – 36.2) ** |
Table 2: Demographic characteristics for cases and controls during a study to assess for risk factors for death, Ivukula subcounty, Namutumba District,
September 2021 – February 2022
Note: COR= Crude Odds Ratio, AOR= Adjusted Odds Ratio, * p<0.05, ** p<0.01, *** p<0.001
Factors associated with deaths among children with severe malaria, Ivukula Subcounty, Namutumba District, September 2021 – February 2022
Community VHT consultations in Ivukula Subcounty were infrequent; neither cases (6%) nor controls (13%) had sought care from a VHT. We also noted that more cases (52%) than controls (35%) sought care in the first 24 hours.
The highest proportion of cases and controls attended a HCIII first, cases 43% and controls 49% (Table 2). While severe malaria is considered an emergency condition requiring urgent attention in clinical settings of level III and above, in Ivukula Subcounty 39% of the cases and 24% of the controls accessed their first level of care from small private clinics. Notably, completion of treatment given at the first facility was much lower among cases than controls (22% vs 61%, p=<0.001) (Table 3). The main reasons noted were death, drug and blood stockouts, referrals, inability to feed and lack of funds to purchase drugs.
Among those who went to a second facility following referral, the most common facility visited was a HCII (38% of cases and 43% of controls). This is in contrast to 11% of cases and 18% of controls who visited a HCII as their first facility an indication that clients did not go to the health facilities referred to since H/C II is not mandated to manage severe malaria cases. Among those given treatment, completion was again more frequent among controls than cases (89% vs 11%, p=<0.001) (Table 3).
Among the 123 cases and controls, 117 said they visited a second health facility without being referred. The most common reasons for visiting additional facilities without referral included: need for higher level of care (75% of cases and 84% of controls), need for blood products (16% cases and 3% controls), and drug stock outs at the first facility (9% cases and 13% controls). Important to note, still the most commonly visited facility was HC II which is not equipped to manage severe malaria cases (78% cases and 74% controls) (Table 3).
There was no difference among cases and controls regarding receipt of indoor residual spraying (IRS) during the last round of IRS in the district, 98% of cases and 96% of controls said their household had been sprayed.
Table 3: Factors associated with death among cases and controls with severe malaria in Ivukula subcounty, Namutumba District, September 2021 – February 2022
| Characteristic
|
Cases (N=46)
n (%) |
Controls (N=77)
n (%) |
COR (95% CI)
|
AOR (95% CI)
|
| Caregiver characteristics | ||||
| Age in years
18-24 25-44 ≥45 Median age |
4 (9) 20 (43) 22 (48) 42 |
7 (9) 52 (68) 18 (23) 35 |
Ref 0.67 (0.17 – 2.6) 2.14 (0.54 – 8.5) NA |
–
|
| Type of caregiver
Father Mother Grandparent |
12 (26) 21 (46) 13 (28) |
17 (22) 52 (68) 8 (10) |
Ref 0.57 (1.23 – 1.4) 2.3 (0.73 – 2.3) |
– |
| Level of education
Secondary Upper Primary None-Lower Primary |
8 (17) 13 (28) 25 (54) |
17 (22) 33 (43) 27 (35) |
Ref 0.8 (0.3 – 2.4) 1.9 (0.7 – 5.4) |
–
|
| Health facility attended first for patients with severe malaria | ||||
| Health facility type
Health center II Health center III Health center IV Hospital Private clinic Drug shop |
5 (11) 20(43) 1 (2) 2 (4) 18 (39) 0 (0) |
13 (18) 35 (49) 3 (4) 0 (0) 17(24) 3 (4) |
– |
– |
| Given antimalarial drugs at first facility
Yes No |
32 (69) 14 (31) |
50(70) 21 (30) |
Ref 0.95 (0.4 – 2.2) |
– |
| Completed treatment given at first facility
Yes No |
10 (22) 36 (78) |
47(61) 30 (39) |
Ref 5.6 (2.4 – 13.0) *** |
Ref 9.7 (1.8 – 52.9) ** |
| Reasons for not completing treatment (among those that could not)
Death Failure to feed Drug stock outs Blood products stock out Referred Failure to pay |
10 (28) 1 (3) 17 (47) 6 (17) 0 (0) 2 (6) |
0 (0) 0 (0) 22 (76) 2(7) 1 (3) 4 (14) |
– |
– |
| Time between illness onset to visiting first facility
≤1 day >1 day |
24 (52) 22 (48) |
25(35) 46 (65) |
Ref 0.5 (0.2 – 1.0) |
Ref 0.8 (0.2 –3.7) |
| Facilities visited after first HF (only for referred patients) | ||||
| Health facility type
Health center II Health center III Health center IV Hospital Private clinic |
11 (38) 3 (10) 9 (31) 5 (17) 1 (3) |
16 (43) 4 (11) 11 (30) 4 (11) 2(5) |
– |
|
| Given treatment at second facility
Yes No |
9 (31) 20 (69) |
18 (48) 19 (51) |
Ref 0.5 (0.2 – 1.3) |
– |
| Completed treatment given at second facility
Yes No |
1 (11) 8 (89) |
16 (89) 2 (11) |
Ref 42.5 (4.1 – 434.9) *** |
– |
Note: COR= Crude Odds Ratio, AOR= Adjusted Odds Ratio, * p<0.05, ** p<0.01, *** p<0.001
In the bivariate analysis, five variables were found to be significantly associated with death among children with severe malaria (Table 2 & 3), only 2 were considered for multivariate analysis, need for blood transfusion, jaundice and having anaemia were excluded from the final model for collinearity with receiving blood transfusion.
From the multivariate analysis, following adjustment for child age, child sex and duration to seek care, two variables were found to be significantly associated with death among children with severe malaria.
The odds of death among the children that did not completed their first treatment were 9.7 times higher than the odds among those who completed treatment (aOR=9.7, 95%CI:1.8 – 52.9), Additionally, the odds of deaths among anemic children who did not receive blood transfusion were 7.1 times higher than those who received blood transfusion (aOR=7.1, 95%CI:1.4 – 36.2) (Table 3).
Discussion
We assessed factors associated with death due to severe malaria among children ≤12 years following an alert of multiple deaths in the community. The analytic findings revealed that failing to complete antimalaria treatment and failure to receive blood transfusion among anemic patients requiring blood all increased risk of death.
We also identified stockouts as a major challenge for health facilities and persons seeking care; care-seeking appeared to be less common during stockouts and low stock levels of antimalarials led to failure to disburse full courses of treatment. Inability to pay for the remaining course of treatment led to incomplete treatments, which were associated with death.
We found a strong association between failing to complete antimalarial treatment and deaths among children. According to WHO, poorly treated severe malaria can lead to high death rates, while effective treatment and supportive care reduces mortality to 10-20%.
It is essential that full doses of parenteral antimalarial medication be given promptly in the initial treatment of severe malaria with a complete dose of intravenous or intramuscular artesunate for at least 24 hours and a continuation of artemisinin-based combination therapy (ACT) for 3 days[7].
However, in Ivukula Subcounty, parents reported that treatment completion was frequently challenged by drug stockouts or low stocks. We confirmed this finding by visiting facilities, where we found reports of antimalarials stockouts as a challenge.
Antimalarial drugs intended for 2 months were lasting a month or less, and artesunate, the required drug for treating severe malaria, lasted only two weeks at the facilities we visited. Additional reports from healthcare workers at facilities that they often gave only one dose to make the drugs last longer, forcing parents to purchase medication for their children sheds some light onto the reasons for non-completion.
When parents are unable to purchase such medications, the child cannot complete treatment. Reassessment of the appropriate quantities of drugs to provide to health centers in the district, especially during upsurges, and emphasizing the importance of treatment completion is needed to ensure that this problem is addressed.
Beyond this, we found that referrals to higher-level facilities that could manage severe malaria were frequently not completed. Caretakers could only manage accessing lower-level facilities near them, yet these facilities are not equipped to manage severe malaria cases.
This likely accounts for the high proportion of patients who accessed H/C IIs as their second level of health-seeking. Addressing this issue requires provision of transport support to enable all referred patients reach the intended referral hospitals, alternatively, upgrading some of the H/C II facilities to levels that can manage severe malaria could improve service access.
The need for blood transfusion and failure to receive it was a risk factor for deaths among children with severe malaria in our study. This is not surprising and likely reflects more severe illness among cases, which was also suggested in our comparison of cases and controls.
Anaemia is one of the major complications of malaria infection, contributing directly or indirectly to hospitalization and deaths in young children. While malaria is responsible for anaemia due to hemolysis, anaemia in turn lowers the body’s immunity leading to increased exposure to malaria infections and hence the repeated cycle[8]. Blood transfusions can be life-saving interventions for children with severe anaemia[9].
However, we found that blood transfusions were more often needed by cases, and less often received, compared to controls. Unfortunately, Ivukula Subcounty has no health facility equipped to provide blood transfusion services. Addressing this issue requires improving blood transfusion services closer to the communities by equipping HC IIIs with blood storage equipments and availing sufficient quantities of blood products.
In contrast to prior studies of severe malaria conducted elsewhere in sub-Saharan Africa[10-12], we did not find an association between age and mortality, perhaps explained by the overall low median age of our study population (< 5 years) relative to previously studied populations. Similar findings are seen in a study conducted in Zambia where age was not significant due to low median age of both cases and controls (<2yrs)[13].
Study limitations
A limitation to this study was the absence of medical records for review. Because of this, we chose to use clinical definitions and relied on the caretakers’ memory to remember the child’s presentation. For case-patients, majority of the caregivers had discarded the records immediately after the loss of their child or were not provided with the records at facilities.
Conclusion
The major contributors to malaria mortality among children ≤12 years in Ivukula Subcounty, Namutumba District were: not completing treatment for malaria, failure to receive blood transfusion among anemic patients that needed blood, stockouts of malaria drugs and blood products and failure to reach referral sites. These issues indicate both health system and individual challenges that need to be addressed. We therefore recommend, increasing access to blood products, accurate quantification of antimalarials for health facilities in upsurge districts, offering transport support to patients referred to higher-level facilities and activation of iCCM in the communities of Namutumba. Upgrade of the H/C IV to hospital status to enable proper management of cases in this area highly prevalent with malaria. Furthermore, an upgrade of health facilities for the district to have a general hospital and more H/C IIIs per subcounty to improved management of severe malaria with limited referrals. All this is hoped to avert numerous deaths among children in this area.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgments
We appreciate Namutumba District Local Government and the Village Health Teams for the guidance in the community during data collection.
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
-
Organisation, W.H. World Malaria Report. 2021.
-
WHO, World Malaria Report2021.
-
Malaria, T. Uganda Malaria Facts, Target Malaria. Severe Malaria Observatory. 2022.
-
Uganda, M.o.H., District health Information system. Division of Health Information. 2022.
-
National Malaria Control Program, M.o.H.U., Uganda National Malaria Control Policy. . 2011. p. Pg 8.
-
District, N. Namutumba District Local Government. 2022; Available from: https://namutumba.go.ug/lg/district-location-and-its-neighbors.
-
WHO, WHO Guidelines for malaria. 2022, Global Malaria Programme: Geneva.
-
Health, C.G. Division of Parasitic Diseases and Malaria 2022.
-
Mutombo, A.M., et al., Severe malaria and death risk factors among children under 5 years at Jason Sendwe Hospital in Democratic Republic of Congo. Pan African Medical Journal, 2018. 29(1): p. 1-8.
-
Carneiro, I., et al., Age-patterns of malaria vary with severity, transmission intensity and seasonality in sub-Saharan Africa: a systematic review and pooled analysis. PloS one, 2010. 5(2): p. e8988.
-
Kamau, A., et al., Malaria infection, disease and mortality among children and adults on the coast of Kenya. Malaria journal, 2020. 19(1): p. 1-12.
-
Kapesa, A., et al., The current malaria morbidity and mortality in different transmission settings in Western Kenya. PloS one, 2018. 13(8): p. e0202031.
-
Ippolito, M.M., et al., Risk factors for mortality in children hospitalized with severe malaria in northern Zambia: a retrospective case-control study. The American Journal of Tropical Medicine and Hygiene, 2018. 98(6): p. 1699.


Comments are closed.