
Dear Reader,
We take great pleasure in welcoming you to Issue 2, Volume 5 of the Uganda National Institute of Public Health (UNIPH) Quarterly Epidemiological Bulletin. This bulletin aims to inform the district, national, and global stake- holders on disease outbreak investigations, public health surveil- lance, and interventions undertaken in detecting, preventing, and responding to public health events in the country. In this issue, we present a variety of COVID-19 related articles including; highlights of Uganda’s COVID-19 outbreak, the role of the PHFP fellows in the COVID-19 response, capacity building in the context of COVID-19, risk mapping and population movements, rapid assessment of compliance to prevention measures, and institutional quarantine in Masindi. We also share an article on sustained vigilance for other public health emergencies amidst COVID -19, rubella outbreak in Nakaseke, and a policy brief 0n using malaria channels based on percentiles to detect malaria epidemics in Uganda
For further information on anything in this bulletin please contact us on: andyabakira@musph.ac.ug, bomoda@musph.ac.ug, ekatana@musph.ac.ug, OR lbulage@musph.ac.ug
We hope this will be a worthwhile and informative read and we shall appreciate all the feedback from you.
Thank You
EDITORIAL TEAM
Dr. Patrick K. Tusiime |
Commissioner, National Disease Control and
Prevention, MoH
Dr. Alex Riolexus Ario |
Director, Uganda National Institute of Public Health, MoH
Dr. Felix Ocom |
Deputy Director, Public Health Emergency Operations Centre, MoH
Lilian Bulage |
Scientific Writer, Uganda Public Health Fellowship Program, MoH
Dr. Benon Kwesiga
Field Supervisor, Uganda Public Health Fellowship Program, MoH
Daniel Kadobera
Field Supervisor, Uganda Public Health Fellowship Program, MoH
Dr. Alex Ndyabakira |
PHFP Fellow, Kampala Capital City Authority Bob
Omoda Amodan |
PHFP Fellow, Uganda National Expanded Program on Immunisation, MoH
Elizabeth Katana |
PHFP Fellow, Kampala Capital City Authority
Inside this Issue;
- Highlights of the COVID-19 outbreak in Uganda, March to June 2020
- Capacity Building in the Context of COVID-19 Outbreak in Uganda
-
The role of PHFP Field Epidemiology Fellows in the response to the COVID-19 pandemic in Uganda, 2020
-
Covid-19 risk mapping and population movement studies along Uganda-Rwanda borders in Ntungamo District, Uganda-Tanzania borders in Isingiro District, and Masaka District, Uganda, May 2020
-
Compliance to COVID-19 prevention measures during early phase of easing the lockdown restrictions in the Kampala metropolitan area
-
Quarantine management during the COVID-19 Outbreak: A Case of Masindi District
-
Sustained Vigilance, Preparedness, and Response to All Public Health Emergencies amidst COVID-19 Pandemic
-
Rubella Outbreak among Vaccinated Children Propagated by Attending School X, Nakaseke District, Uganda, January 2020
- Policy brief: Using malaria channels based on percentiles to detect malaria epidemics in Uganda
Highlights of the COVID-19 outbreak in Uganda, March to June 2020
Authors: Maureen Nabatanzi1, Daniel Eurien1, Godfrey Nsereko1, Benon Kwesiga1, Daniel Kadobera, Bernard Lubwama2, Alex Riolexus Ario1, Julie Harris3
Affiliations;
1Uganda Public Health Fellowship Program, Kampala, Uganda
2Integrated Epidemiology, Surveillance and Public Health Emergencies Department, Ministry of Health, Uganda
3US Centers for Disease Control and Prevention, Kampala, Uganda
Summary
On 21 March 2020, Uganda’s Ministry of Health (MoH) confirmed the country’s first case of COVID-19. The initial response included: institutional quarantine of suspected cases, contact tracing and follow up, and stepping up efforts in alert verification and testing. To strengthen social distancing recommendations and reduce movement of people, public transportation was banned and use of private cars limited to a maximum carriage of three persons. Despite these interventions, Uganda registered 696 confirmed cases, including 20 health workers by 13 June, and 165 local infections by 5 June 2020. The local infections were in 30 districts. We recommend strengthening of COVID-19 surveillance in all districts of Uganda.
Highlights of the COVID-19 outbreak in Uganda
On 21 March 2020, Uganda’s Ministry of Health (MoH) confirmed the country’s first case of COVID-19. The index case-patient had returned from a high-risk country and was identified through routine screening at Entebbe International Airport. Subsequently, most of the initial cases were among travelers from high risk countries and truck drivers. However, there was a shift in the confirmed cases to trans-border truck drivers and their contacts in and around the country’s points of entry (PoEs).
As of 12 June 2020, 696 confirmed cases had been reported (Figure 1). There was a surge in cases in May. Between 30 May and 5 June, 264 new COVID-19 cases were registered compared to the 156 from 23rd to 29th May. At 69%, this was the highest weekly increase in cases the country had had since the outbreak begun. Of the 264 cases confirmed between 30 May and 5 June week, 120 (45%) were trans-border truck drivers.
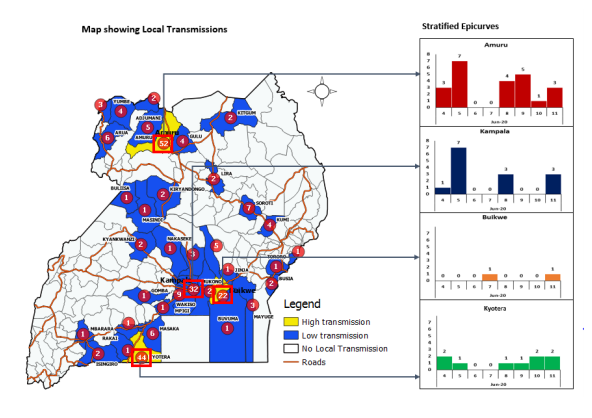
As of 5 June, a total of 20 health care workers tested positive for COVID-19, 16 of them were identified from health facilities and four were among the response teams. There is evidence of increasing local infections. By 5 June, Uganda had 165 known local infections in 30 districts. The most affected districts were: Amuru (36, 22%), Kampala (21, 13%) and Kyotera (20, 12%).
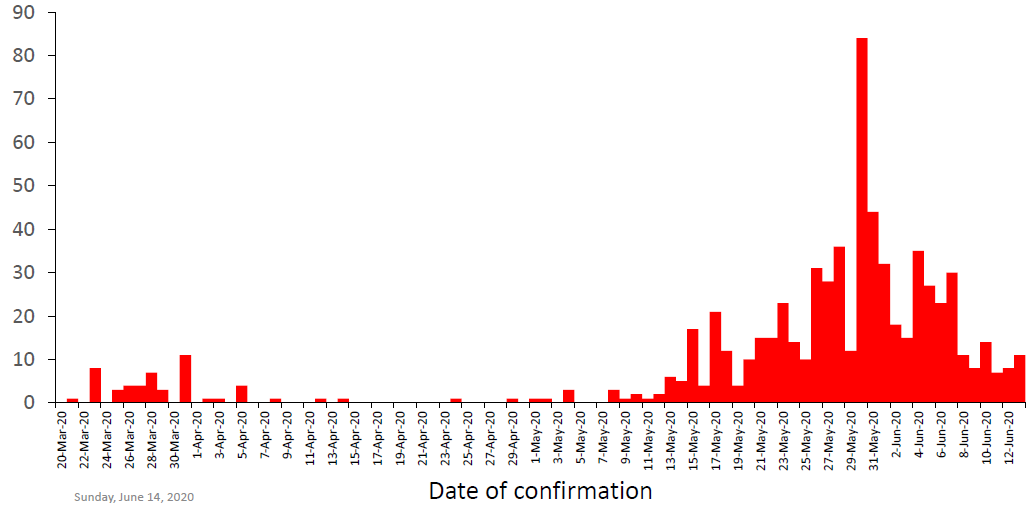
Figure 1: Curve of COVID-19 cases by date of confirmation, Uganda, 20 March-13 June 2020
Public health interventions
The initial response to the outbreak included: institutional quarantine of suspected cases, contact tracing and follow up, and stepping up efforts in alert verification and testing. To strengthen social distancing recommendations and reduce movement of people, public transportation was banned and use of private cars limited to a maximum carriage of three persons. Private transport for non-essential workers was suspended and passengers coming into Uganda by air, land or water were stopped. Pedestrians from neighbouring countries were also prohibited from entry into the country. In addition, public gatherings in bars, churches, theatres were banned and schools and universities were closed (Figure 2).
Response activities
The Ministry of Health strengthened screening and laboratory sample testing for COVID-19. Mandatory testing included: all persons crossing into Uganda at various PoEs, contacts and suspected cases. As of 5 June, a total of 131,714 samples had been collected and tested for COVID-19. Tracing and follow up of contacts of confirmed cases enabled the prompt identification, isolation and testing of exposed persons. As of 5 June, the cumulative number of contacts listed were 6,493, a total of 5,376 (75%) of the listed contacts had completed the 14 days of follow-up while 1,117 (25%) contacts were still under follow up. Institutional quarantine was used to prevent further transmission of COVID-19 from exposed persons to unexposed community members. Between 20 March and 5 June, 4,119 persons were quarantined at 68 quarantine centres for 14 days. Of these 4,119, 125 (3%) tested positive for COVID-19. Confirmed case-patients were managed at Uganda’s 16 regional referral hospitals and Mulago national referral hospital. As of 13 June, Uganda had registered 240 recoveries out of the 696 confirmed cases (34%) and no deaths.
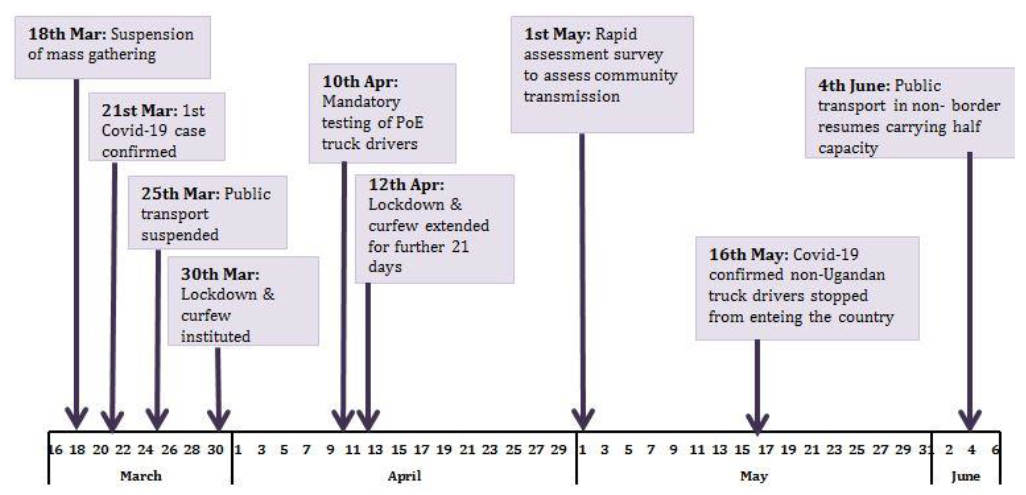
Figure 2: Chronology of COVID-19 public health interventions in Uganda, March-June 2020
Conclusion and recommendations
The COVID-19 outbreak in Uganda is shifting from predominantly imported to more local infections. There is need for case investigations to enable immediate identification and categorization of hot spots for effective response. The increase in detected local infections also implies that all districts must heighten COVID-19 surveillance. Districts with high risk of local transmission should be supported in strengthening surveillance.
References
- Uganda COVID-19 Analytical Report Week 30th May to 5th June 2020
- Uganda COVID-19 Surveillance Update, 14th June 2020
Uganda COVID-19 Situation Report 116, 12th June 2020
Capacity Building in the Context of COVID-19 Outbreak in Uganda
By Irene B. Kyamwine, PHFP Fellow
On 21 March, 2020 Uganda, registered the first case of the novel corona virus (SARS-COV 2), virus causing the Corona Virus disease (COVID-19) in a Ugandan returning from Dubai. The new disease (COVID-19) first detected in Wuhan city in December 2019, was declared a pandemic by the World Health Organization on 11 March 2020. Since its discovery, the knowledge on COVID-19 outbreak has been evolving rapidly. The WHO guidance was mainly implementation of infection prevention and control (IPC) measures and surveillance in order to control the pandemic. Therefore, strict adherence to IPC measures including PPE, social distancing, early detection, isolation and management of patients, among others were the measures that would prevent the rapid spread. However, health workers had limited knowledge on management and prevention of this new disease which made them increasingly fearful of contracting it and leading some to abandon suspected cases and flee health facilities. In view of this, Ministry of Health in partnership with various organizations organized trainings for national and regional level trainers of trainees (ToT). These trainers then conducted a series of orientations for District health teams and the district Task Forces and four-day trainings targeting health workers, managers, and other stakeholders in both public and private organizations. The district COVID 19 orientation was carried out in 133 districts across the country. The trainings were in two forms; classroom and online. Classroom sessions were conducted where space allowed for appropriate social distancing. Online sessions were conducted following the lockdown in the country and in areas where space was not sufficient. The training involved both power point presentations and practical sessions including: donning and doffing of PPE, hand washing, and sample collection. Key areas covered during the training included; Epidemiology, case management, surveillance, contact tracing, specimen collection and testing, infection prevention and control, and psychosocial sessions. The trainings were officiated by, the commissioner for Clinical Services at Ministry of Health Uganda. Following these trainings districts developed district response plans for COVID-19, District task forces were activated and trainings were scaled down to lower health facilities. Reporting on COVID-19 activities also, drastically improved from below 7% before the trainings to 71% by 28 April, 2020 the month when the trainings were conducted.

Upcoming Events and updates
1. World Hepatitis Day, 28th July 2020
According to WHO, viral hepatitis B and C affect over 300 million people worldwide causing about 1.4 million deaths a year. Hepatitis is considered the second major killer infectious disease after Tuberculosis, and 9 more people are now infected with hepatitis than HIV. In commemoration of the World Hepatitis day, the public is urged to know, test, and treat hepatitis while the policy makers are encouraged to invest in eliminating hepatitis.
2. World Suicide Prevention Day; 10 September 2020
World Suicide Prevention Day is organized by the International Association for Suicide Prevention (IASP). The World Health Organization is a co-sponsor of the day. The purpose of this day is to raise awareness around the globe that suicide can be prevented. Suicide is among the top 20 leading causes of death globally for people of all ages, and responsible for over 800,000 deaths, which equates to one suicide every 40 seconds.
3. World Patient Safety Day; 17 September 2020
No one should be harmed in healthcare and yet, about 134 million adverse events continue to occur each year due to unsafe care in hospitals in low- and middle-income countries, contributing to 2.6 million deaths annually. The World Health Organization held the first-ever annual World Patient Safety day on 17 September 2019, and also launched a global campaign to create awareness of patient safety and urge people to show their commitment to making healthcare safer.
4. MASS CAMPAIGN FOR DISTRIBUTION OF 27 MIL- LION MOSQUITO NETS LAUNCHED; 17 June 2020
This campaign will take place in a wave-based manner starting with the districts with the highest prevalence of Malaria and those that have been affected by floods. Twenty-five districts will be covered under wave 1 and these include; Alebtong, Amolatar, Budaka, Bududa, Bugiri, Bukwo, Bulambuli, Butaleja, Butebo, Dokolo, Kaberamaido, Kalaki, Kapchorwa, Kibuku, Kween, Lira, Mbale, Namisindwa, Namutumba, Otuke, Paliisa, Serere, Sironko, Soroti and Tororo.
The campaign will be conducted in observance of the COVID-19 preventive measures. Village Health Teams and the rest of the net distribution team will spend very few hours in the homes and there will be no community mass gatherings as it has been in the previous campaigns. The teams will be fully donned in Personal Protective Equipment while registering households and distributing the mosquito nets.
The role of PHFP Field Epidemiology Fellows in the response to the COVID-19 pandemic in Uganda, 2020
Authors: Elizabeth Katana1, Alex Ndyabakira1, Steven N. Kabwana1, Lilian Bulage1, Alex R. Ario1, Julie Harris2
Affiliations;
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda
2US Centers for Disease Control and Prevention, Kampala, Uganda
Correspondence: ekatana@musph.ac.ug
The Uganda Public Health Fellowship Program (UPHFP), established in 2014 by the Ministry of Health (MoH) in partnership with Makerere University School of Public Health and the U.S. Centers for Disease Control and Prevention (CDC), aims to develop a competent public health workforce to manage epidemics and improve disease surveillance in Uganda. Fellows in this program, all of whom must enter with a Master’s Degree, typically spend 85% of their two years in MoH placements, providing service delivery directly relevant to MoH needs, gaining competencies in major public health domains as well as conducting outbreak investigations countrywide whenever the need arises. Since 2015, PHFP has graduated 40 fellows, and has 25 currently in training; 13 in their first year (cohort 2020), and 12 in their second year (cohort 2019).
Historically, PHFP has played a critical role in supporting the MoH in a wide range of activities. By 2018, fellows had investigated more than 91 outbreaks country wide. Some notable outbreak investigations included typhoid in 2015, yellow fever and meningitis in 2016, and multiple nationwide outbreaks of cholera, malaria, measles, and others (1). PHFP fellows today are valued members of the National Rapid Response Team of the National Task Force (NTF) for Public Health Emergencies.
In March 2020, the World Health Organization declared the novel coronavirus (COVID-19 disease, caused by the SARS-CoV-2 virus) a pandemic. By June 14, 2020, over 7 million people were reported to have been infected with COVID-19 across 213 countries globally, including 696 confirmed cases in Uganda. Since February 2020, all fellows, staff, and several alumni of UPHFP have been actively involved in the countrywide preparedness and response efforts for the COVID-19 pandemic in Uganda, working closely with the COVID-19 National Task Force. The COVID-19 National Task force is charged with establishment of a strong response system to be able to prevent, detect and respond to suspected cases of COVID-19 in collaboration with other relevant ministries, agencies and departments of Government and was formed in mid-January by the Ministry of Health at Public Health Emergencies Operations Center (PHEOC).
Before cases were recognized in Uganda, the MoH set up active surveillance and risk communications activities at the Entebbe International Airport, as this was the likeliest mechanism of COVID-19 introduction into Uganda. During January-March 2020, all twelve Cohort 2019 fellows conducted risk communication and assessment, screening, and active surveillance activities at the Entebbe International airport, ultimately enabling the detection of the first case in Uganda on March 21, 2020. These Fellows also closely monitored several high-risk travelers in areas of Entebbe and Kampala who were quarantining at their homes to ensure rapid identification and evacuation of any symptomatic COVID-19 suspects.
Many of the PHFP alumni drafted Standard Operating Procedures (SOPs) for contact tracing, which are still being used today. Contact tracing, which involves identifying contacts of cases and quarantining them, effectively breaks the chains of transmission of infectious diseases. Contact tracing is a key strategy for preventing further spread of an infectious disease during an outbreak.
Starting in March 2020, following the confirmation of the first COVID-19 case in Uganda, several alumni and fellows were officially deployed by the Public Health Emergency Operations Center (PHEOC) to be part of the COVID-19 National Task Force, activating district task forces, managing the COVID-19 national case database, overseeing proper data collection and entry, and harmonizing data from different sources such as laboratories, hospitals, and points of entry, among others.
With the increasing number of cases, the needs soon exceeded the capacity of the team, and it became necessary to train others in public health intervention activities, including contact tracing and surveillance. All twelve Cohort 2019 fellows were part of a team that drafted training materials and SOPs for enhanced surveillance and conducted Trainers of Trainers (TOTs) for enhanced surveillance for surveillance teams in all regions countrywide.
In mid-March, three PHFP Cohort 2020 fellows, Richard Migisha, Patricia Thiwe and Aggrey Byaruhanga, conducted Training of Trainers (TOTs) sessions for contact tracing and surveillance teams at the Emergency Operations Center. These TOTs enabled the team to multiply knowledge about contact tracing and surveillance, effectively increasing the capacity for response to COVID-19 many folds.
Beginning in March 2020, referral hospitals around the country began serving as isolation centers, caring for persons who tested positive and whose cases required investigation. Case investigation is an important component of public health efforts, enabling efficient management and support for patients during an epidemic response, and also supports the identification of exposed contacts, to stop the transmission chains. Two fellows (Richard Migisha and Ignatius Wadunde) and alumni Bernadette Mirembe Basuta have been part of the case investigation teams at isolation units of referral hospitals countrywide, conducting in-depth interviews with confirmed cases. Ultimately, these case investigations yielded high-quality information about relevant exposures for the cases, as well as providing information about the clinical picture of COVID-19 disease in Uganda. The findings and reports from these investigations have been used by MoH and stake holders to subsequently guide the response.

On May 1, 2020 Masindi District reported a confirmed case of COVID-19 in a police officer who was identified through a rapid and widespread community testing initiative. The police officer had interacted with more than 800 persons while he was ill. A team of four Cohort 2020 fellows (Josephine Namayanja, Immaculate Akusekera, Bob Omoda Amudan and Geoffrey Amanya) was dispatched to investigate and support Masindi district in the efforts to respond to the outbreak. These fellows established, functionalized, and supervised four institutional quarantine facilities in the district. Organized institutional quarantine is an important public health practice and a valuable way to control geographical spread of infectious disease outbreaks including COVID-19.
Another team of three Cohort 2020 fellows (Peter Oumo, Job Morukileng, and Daniel Emong) was tasked with similar activities in mid May 2020, in Kyotera District following an upsurge in confirmed cases of COVID-19 among truck drivers crossing at border points in Kyotera. This ensured that fellows were able to identify practical solutions that would fit the communities at hand while conducting field activities and also strengthen their skills in community engagement activities.

In mid-May 2020, with closure of the airport, the COVID-19 epidemic had shifted from imported cases in high risk travelers accessing the country by air to cases among persons crossing at land border points including truck drivers and their contacts as well as unauthorized travelers using porous borders. Human movements have been known to significantly contribute to the spread of infectious diseases outbreaks over the years. As a result, it was important to understand population movements at some of the Points of Entry, to gain a better understanding of where the highest risk might be. Four Cohort 2020 fellows (Alex Ndyabakira, Job Morukileng, Geoffrey Amanya, and Bob Omoda Amudan) were tasked with risk mapping and monitoring population movements of truck drivers and high-risk travelers at major Points of Entry of Ntungamo, Mirama Hills, and Tanzania, including several porous borders such as Kikagati and Buganga. These fellows also followed, documented, and mapped these transient populations in major town centers of Masaka District. Risk mapping and monitoring population movements enables understanding of the risks or threats that may arise from these key population movements that could impact negatively on the efforts to control an epidemic in public health responses.
Several alumni and fellows were deployed by Ministry of Health to serve as COVID-19 Epidemiologists at district levels. These have activated district response task forces, established active community surveillance and trained district contact tracing teams country wide. This has enabled capacity building and improved workforce in the country’s response to the COVID-19 epidemic. Fellows have also made presentations to the National Taskforce which has informed the implementation of non-pharmaceutical interventions to contain the pandemic in Uganda.
The participation of PHFP Fellows in various activities of the COVID-19 response has filled critical human resource gaps at the Ministry of Health and enabled the fellows to obtain competencies in applied epidemiology, public health leadership, communication as well as conducting surveillance. The fellows will continue to support the COVID-19 response in the coming months, as well as many other public health issues and outbreaks.
In summary PHFP fellows and graduates have contributed substantially in all core components of Uganda’s COVID-19 response and preparedness. Their contribution, training and service during COVID-19 will serve as a pillar for development of a workforce competent in real-time disease surveillance and response to Public Health Emergencies.
References
- Ario AR, Bulage L, Kadobera D, Kwesiga B, Kabwama SN, Tusiime P, et al. Uganda public health fellowship program’s contribution to building a resilient and sustainable public health system in Uganda. Glob Health Action. 2019 Dec 13;12(1):1609825.
Covid-19 risk mapping and population movement studies along Uganda-Rwanda borders in Ntungamo District, Uganda-Tanzania borders in Isingiro District, and Masaka District, Uganda, May 2020
Authors: Job Morukileng1, Geoffrey Amanya1, Alex Ndyabakira1, Bob Omoda Amodan1, Lilian Bulage1
Institutions
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda
Corresponding Author: Job Morukileng, Email, jmorukileng@musph.ac.ug Mobile: +256782611585
Summary
Population mobility and connectivity facilitates movement and introduction of pathogens through infected travelers. Therefore, understanding population movement and connectivity patterns and how this relates to COVID-19 transmission is vital for planning and designing control strategies. In this study, we adopted the Centre for Disease Control and Prevention (CDC) Population Connectivity Across Borders (PopCAB) toolkit to assess and characterize population movement and connectivity patterns along the border districts of Ntungamo, Isingiro and Masaka/Kyotera. We identified seven landing sites, 15 trading centers, two streets in Masaka Town, 8 health facilities, 20 POE (5 official and 15 illegal) and one refugee settlement as areas of interest for mobile populations and the local communities. Our results further demonstrate that, transporters (truck drivers and boda bodas), sex workers (in Nyendo and Rubaare); traders/vendors on highways and trading centers, restaurant attendant’s, health workers (mainly in Masaka RRH), car mechanics (in Nyendo) and refugees, are high-risk groups. We recommended targeting priority areas and populations with interventions such as mass screening for COVID-19, strengthened community-based surveillance systems, risk communication, reinforced security at points of entry, provision of essential supplies, delayed opening of concentrated places such as schools, markets, places of worship and public transport.
Background
Human movement is associated with infectious diseases transmissions. As transport networks continue to expand in reach and speed of travel, pathogens and their vectors can now move further and faster than ever before. [1]. The current example is the significant contribution of human mobility to the spread of COVID-19 from Wuhan, Hubei province in China where it was first reported to the entire world[2]. As of 29 May, nearly four in five confirmed cases in Uganda were imported from the neighboring countries[3]. However, much of the Ugandan border remains porous, posing a risk of entry of unauthorized persons. As with the original SARS-CoV epidemic of 2002/2003, predictive risk mapping using population travel data, and tracing and mapping super-spreader trajectories are proving vital for timely and effective epidemic monitoring and response[2]. However, in Uganda, population movement and connectivity are not well understood, yet the government was in the process of lifting travel restrictions. We conducted COVID 19 risk mapping and population movement and connectivity patterns along border districts of Ntungamo and Isingiro in the southwest and Masaka District in Central Uganda to inform control and prevention measures
Methods
We assessed Corona Virus Disease (COVID-19) risk and population movement patterns using the Population Connectivity Across Borders (PopCAB) toolkit, a CDC innovation, in Uganda’s southwestern border districts of Ntungamo and Isingiro, and Masaka District in central Uganda. We conducted Key Informant Interviews (KIIs) with the district leadership involved in the COVID 19 task force, and district security and intelligence, including, the Resident District Commissioners (RDC), District Internal Security Officers (DISOs), District Surveillance Focal Person, and District Police Commanders (DPCs). These were purposively selected based on their role in national security and COVID-19 pandemic response. The KIs guided the identification of priority areas and participants for focused group discussions (FGD) at community level. We identified the long-distance truck drivers, motorcycle riders, local leaders, business people, sex workers, and farmers in priority locations to participate in the FGDs. Through a participatory approach, all important places and routes of interest before and after COVID-19 cross border movement restrictions and lock down, were plotted on the local district maps. After FGDs, we took GPS coordinates for important places of interest identified during the discussion. We further took guided walks at the Point of Entry (POE) and identified priority areas in order to observe the on-going activities.
Results
In Isingiro district, we identified the following areas of interest: Nakivale refugee settlement (hosting Congolese, Rwandese, Burundians and other nationals who move in and out of the
country through porous borders); Kamwema POE, Endiizi Trading Centre (close to the border and hosts illegal entrants), and Bugango and Kikagate POE. The populations identified to be at risk included Refugees, business people/venders in the POE and along the routes from POE to Isingiro Town, health care workers (in Nakivale health center III, Rwambaga health center III and Kikagate health center III), and Truck drivers.
In Ntungamo District, Mirama hills POE, Sofia Town (border town with several illegal entry points), Kizinga POE, Ngoma Trading Centre( close to the border with large farms that employ illegal entrants from Rwanda), and Rubaare Town Council (known for sex workers and the main stopping point for truck drivers) were identified as areas of interest for the populations. The Truck drivers; sex workers (in Rubaare town); illegal immigrants from Rwanda (youth); the matooke farmers and business people/venders in the POEs and along the roads were identified as the most at-risk groups.
The areas of interest identified in Masaka District included Nyendo Town Council (known for sex workers, vehicle garages, washing bays, and bars and lodges), Hobat and Budu streets (main destination for produce and general merchandise trucks from Tanzania, Rwanda, Kenya and within Uganda), the Masaka Regional Referral Hospital (the main treatment center for COVID-19 cases and other diseases), landing sites in Bukakata and Marembo, and Kalisizo Trading Centre a long Mutukula POE-Masaka road. We identified the following categories of people as the most at risk in Masaka District, drivers for fish and other cargo trucks; sex workers (mostly in Nyendo); health workers; wholesalers in Budu and Hobat streets (Masaka town); mechanics mostly in Nyendo, restaurant and bar attendants and passion fruit, tomatoes and pineapple farmers in the growing villages of Marembo and Bukakata.
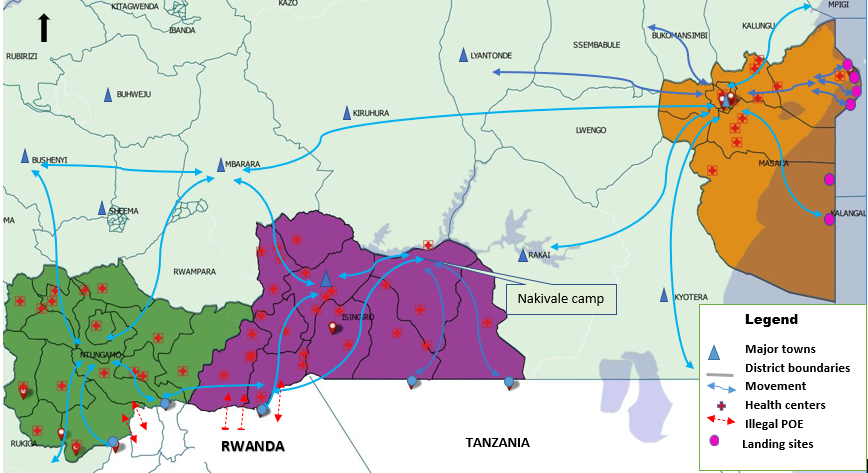
Figure 1: Map showing population movements in Isingiro, Ntungamo, and Masaka Districts, May 2020
Discussion
Although the lock down and the closure of border crossings significantly minimized movements in the Uganda and through the legal Points of Entry, the people in Southwestern border districts of Ntugamo and Isingiro continue interacting with Rwandese, Burundians and Tanzanians through the porous borders. Persons from neighboring Tanzania who enter through illegal routes, mainly access nearby villages to visit relatives and to buy and sell goods. The Rwandese similarly cross to nearby villages to visit relatives but also look for work in farms. Some proceed to the refugee settlement at Nakivale in Isingiro District.
Although Masaka District is not directly bordering any country, Tanzanians can access Masaka District directly through Lake Victoria. Masaka is also a converging point for the main routes originating from the Southwestern border district and is the exit point towards the capital Kampala. Masaka is a large town with major schools, hotels, garages, large wholesale shops, restaurants, and health care facilities, making it a main destination for the travelers and the population from neighboring districts. Being a converging and stopping point means that Masaka District continues to receive a significant amount of traffic even during lock down which puts the district at a heightened risk for transmission of COVID-19 virus.
The study results show that the populations remain mobile and interconnected at district and regional scale even in amidst of lockdown. By mapping these population movements and connectivity, especially for the border districts, a valuable evidence base to guide disease surveillance as well as control and elimination planning can be improved. In this study, we identified seven landing sites, 15 trading centers, two streets in Masaka Town, 8 health facilities, 5 official points of entry, and 15 illegal POEs, and one refugee settlement as areas of interest for mobile populations and the local communities. Interactions in the priority/areas of interest increases risk of infection among the transporters (truck drivers and boda bodas), sex workers, traders/vendors on highways and trading centers, restaurant attendant’s, health care workers, security officials; famers (for tomatoes, matoke, passion fruits and pineapples), car mechanics and refugees.
Conclusion
Although the lockdown has minimized population movement and connectivity in the districts under study, cross border interactions continue through the porous borders and legal POE. This interaction translates into increased risk of COVID-19 importation and transmission in the identified areas and populations.
Recommendations
We recommend that the MoH and health implementing partners target the priority areas and categories of people with tailored COVID-19 interventions such as; COVID-19 mass testing, risk communication; improved community based surveillance; providing supplies to priority locations; Delaying opening areas of concentration such as markets, schools, public transport, and places of worship in the hot sports and increasing deployment of security in illegal POE to minimize unauthorized cross border movements.
References
- Tatem, A.J., D.J. Rogers, and S.I. Hay, Global transport networks and infectious disease spread. Advances in parasitology, 2006. 62: p. 293-343.
- Boulos, M.N.K. and E.M. Geraghty, Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. 2020, BioMed Central.
- Uganda, M.o.H., COVID-19 Situation Report#103, 29/05/2020 update, accessed on 2020/05/29. available at https://veoci.com/veoci/p/w/f/abgy41atnue1t6r4/Ug_COVID-19_Sitrep%23103_+29May2020.pdf
![]()
![]()
. 2020.
Compliance to COVID-19 prevention measures during early phase of easing the lockdown restrictions in the Kampala metropolitan area
Authors: Alex Ndyabakira1, 2, Elizabeth Katana1, 2, Daniel A. Okello2, Aggrey Byaruhanga1, Geoffrey Amanya1, Richard Migisha1, Daniel Kadobera1, Julie Harris3, Alex A. Ario1
Affiliations; 1Uganda Public Health Fellowship program, Kampala, Uganda
2Directorate of Public Health and Environment, Kampala Capital City Authority, Kampala, Uganda
3Division of Global Health Protection, Center for Global Health, Centers for Disease control and prevention, Kampala, Uganda
Summary
On March 25, 2020, the government of Uganda instituted a total lock down and curfew in addition to other public health response measures in response to the COVID-19 pandemic. Six weeks later with little community transmission, the president gradually relaxed some of the COVID-19 lockdown restrictions. In light of an expected additional lifting of the lockdown measures we estimated the level of compliance to COVID-19 preventive measures to inform phased lifting of the lockdown. We conducted an online survey using a structured questionnaire designed using Google Docs and administered online to the general public from 8th to 15th May, 2020. We also purposively selected six sites in Kampala Metropolitan and observed practices of the general public on COVID-19 preventive measures from 10th to 13th May, 2020.
Out of the 965 respondents, only 23% were compliant with all the three key preventive measures (use of face mask in public, practicing social distance, and proper hand washing). Despite the 652 (68%) of the respondents having access to a face mask, only 293 (30%) regularly used it in public. Among the 965 respondents, 736 (83%) always practiced regular hand hygiene. However, only 496 (56%) always practiced social distancing outside of the home.
Compliance to the key COVID-19 preventive measures was low. Social distancing and consistent use of face masks in public were the least adhered to while hand washing was higly complied to. We recommend more enforcement and leveraging public access to face masks if compliance to COVID-19 preventive measures in public places is to be achieved.
Background
On March 18, 2020, the government of Uganda instituted several strategies such as halting mass gatherings, closure of learning institutions, and churches to reduce the risk of importation and spread of COVID-19 in the country. However, on March 21, 2020, Uganda detected the first case of COVD-19, a traveler who had returned from Middle East through mandatory screening of all travelers. Following this, the government instituted a number of control and prevention measures including total lock down and curfew on March 25, 2020.
Six weeks later (May 6, 2020), only 91 cases had been detected in the country, with little community transmission detected (8%). As a result, the President gradually relaxed some of the earlier restrictions. These included opening of large scale or whole sale trade, ware houses, garages, hard wares, and workshops in an attempt to spur economic growth. At the time, the Ministry was waiting for the results of the rapid assessment survey expected to establish the extent of community spread of the COVID-19 before the final position on easing the lock down could be reached. In light of an expected additional lifting of lockdown measures, it was important to understand the extent of adherence to the current recommended preventive measures. Information on adherence to the control and prevention measures was likely going to become increasingly important as human interactions would return to normal levels. We estimated the level of compliance to COVID-19 preventive measures to inform phased lifting of the lockdown.
Methods
We used a structured questionnaire designed using Google Docs and administered online to the general public from 8th to 15th May, 2020. The questionnaire was composed of questions on socio-demographics including age, sex, education level, employment status, daily life during the lock down lifting including ability to return to work and the means of transportation used, COVID-19 preventive practices including practicing social distancing outside the home, having access to a face mask, wearing a face mask in public, proper hand washing practices, shaking people’s hands, and hugging people.
We also purposively selected six sites in Kampala Metropolitan and observed practices of the general public on COVID-19 preventive measures from 10th to 13th May, 2020. We selected central business district (CBD) at Ben Kiwanuka Street, Kisenyi (downtown Kampala), Parliamentary Avenue (uptown Kampala), Kireka (Kampala suburb), Katanga (informal slum settlement), and Kalerwe daily food market.
Results
Online survey
Socio-demographic characteristics of the participants during early phase of easing the lockdown restrictions in Kampala metropolitan area, May 8-15, 2020
| Characteristic (N=965) | Frequency | Percentage |
| District of Residence*(n=948)
Kampala Wakiso Mbarara Mukono Others |
308 224 53 53 310 |
32.5 23.6 5.6 5.6 32.7 |
| Sex
Male Female |
640 325 |
66.3 33.7 |
| Highest level of education attained
None Primary school Secondary school Vocational or technical institution College/University Post-university education |
0 4 20 31 529 381 |
0 0.4 2.0 3.0 55 40 |
| Current employment status
Private sector/Self-employed/Business Non-government Organization (NGO) Public sector Unemployed |
450 158 280 77 |
47.0 16.0 29.0 8.0 |
| Able to return to regular work
Yes No I work from home Unemployed |
252 503 138 72 |
26.1 52.1 14.3 7.5 |
| Means of transportation to work
Unable to move Work from home Walk Boda Boda/Motorcycle/Bicycle Privately-owned car or other means Government/Company transport van/bus Unemployed |
427 116 107 46 108 90 71 |
44.3 12.0 11.0 4.8 11.2 9.3 7.4 |
A total of 965 persons responded to the online survey. The mean age of the participants was 39 years (13-79) and 66% (640/965) were males. More than a half, 56% (532/948) of the respondents were residents of Kampala and Wakiso. Fifty five percent (529/965) had college or university highest level of education, and 47% (450/965) were working with the private sector or self-employed or business. More than half 52% (503/965) had not yet returned to work and majority 44% (427/965) were unable to move (Table 1).
Table 1: Socio-demographic characteristics of the participants during early phase of easing the lockdown restrictions in Kampala metropolitan area, May 8-15, 2020
The level of compliance with COVID-19 preventive measures among participants during early phase of easing the lockdown restrictions in Kampala metropolitan area, May 8-15, 2020
Overall, only 23% (222/965) of the respondents always practiced all the three key preventive measures (use of face mask in public, practicing social distance and proper hand hygiene). Despite the (652/965) 68% of the respondents having access to a face mask, only (293/965) 30% regularly used it in public. Among the respondents, (736/965) 83% practiced regular hand hygiene. However, only (496/965) 56% practiced social distancing outside of home (Table 2).
Table 2:
| Characteristic (N=965) | Frequency (percentage) | Frequency(percentage) |
| Always compliant with the three preventive measures (uses facemask in public, hand washing and social distancing) | Yes
222 (23.0) |
No
743 (77.0) |
| Always wear a face mask in public | 293 (30.0) | 672 (70.0) |
| Always practices social distancing (at least one meter from closest person) | 540 (56.0) | 425 (44.0) |
| Always practices proper hand washing and hygiene | 802 (83.0) | 163 (17.0) |
Community Observations of public face mask use and hand washing practices in Kampala metropolitan area, May 10-13, 2020
The community observations revealed that face mask use was very low from all the Kampala sites. In all the six sites, the proportion of those wearing face masks correctly was less than 30% (table 3).
Table 3: Community observation of public face mask use among 1,167 persons at different locations in Kampala metropolitan area, May 10-13, 2020.
| Venue | Correctly wearing mask (n) | Incorrectly wearing mask (n) | Not wearing mask at all (n) | Percentage wearing mask correctly |
| Central Business District | 8 | 4 | 108 | 6.7 |
| Kisenyi (down town) | 30 | 9 | 270 | 9.7 |
| Parliamentary avenue (up town) | 35 | 27 | 93 | 22.5 |
| Kireka (Kampala suburb) | 5 | 0 | 200 | 2.0 |
| Kalerwe foodmarket | 10 | 5 | 250 | 3.8 |
| Katanga (informal slum settlement) | 0 | 0 | 113 | 0.0 |
Hand washing was fairly practiced compared to use of face masks with some sites such as commercial banks observed with 100% compliance (table 4).
Table 4: Community observations of hand hygiene practices before gaining access to a public place among 170 persons in Kampala city, May 10-13, 2020
| Location | Hand washing
(n) |
Not hand washing (n) | Percentage of hand washing (%) |
| Kalerwe food market | 75 | 5 | 94.2 |
| Commercial bank | 40 | 0 | 100.0 |
| Office block | 23 | 7 | 76.0 |
| Super market | 16 | 4 | 78.6 |
Discussion
In the online survey, out of the 965 respondents, only 23% were always compliant with all the three key preventive measures of COVID-19.
Conclusion
Compliance to the COVID-19 preventive measures was low. Social distancing and consistent use of face masks in public were the least adhered to; many people were seen wearing face masks incorrectly. Hand washing was higly complied to, possibly due to the fact that hand washing facilities were provided free of charge in most public and private places. More enforcement and leveraging public access to face masks is required if compliance to COVID-19 preventive measures in public places is to be achieved.
References
- UDHS. Uganda Demographic Health Survey project (UDHS) in 2016 [Internet]. Uganda Bureau of Statistics Kampala, Uganda The DHS Program ICF Rockville, Maryland, USA; 2016. Available from: https://dhsprogram.com/pubs/pdf/FR333/FR333.pdf
Quarantine management during the COVID-19 Outbreak: A Case of Masindi District
Authors: Josephine Namayanja1, Geoffrey Amanya1, Immaculate Akusekera1, Bob Omoda Amodan1, Daniel Kadobera1
Institutions
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda.
Corresponding Author: jnamayanja@musph.ac.ug
Summary
On May 1, 2020 Masindi District reported a confirmed case of COVID, identified through the rapid community assessment survey. We supported the district to respond to the outbreak including conducting epidemiological investigations and setting up and managing of
BACKGROUND
On May 1, 2020 Masindi District reported a confirmed case of COVID-19, identified through the rapid community assessment survey. At the time Uganda had reported 83 COVID-19 positive cases with 52 recoveries (74 imported cases). By May 2, 104 persons had been identified to have been in direct contact with confirmed case-patient shortly before his evacuation. 34 of these were army officers and were being quarantined at Masindi Army barracks Secondary School, 28 who included family members of the case-patient and workmates who were in Masindi General Hospital quarantine whereas 42 were inmates in Masindi Police cells. The number of quarantined persons in the hospital increased (from 28 to 49 people) as more people were admitted, claiming to have been in contact with the case-patient and this caused congestion. Males and females were sharing the same toilet and bathroom facilities. At some point, male and female quarantined persons were sharing the same ward and much as the newly recruited contacts were being put in a separate wing of the ward, they could still cross to the wing of those who had been recruited earlier. The location of the Hospital quarantine was in itself not appropriate as it could expose the hospital staff given that the centers were holding high risk contacts. At the same time, the inmates were granted a police bond but they could not be left to return to the communities. Some of the facilities lacked records on when the contacts were last with the case and when they were recruited into the facility. Security was lacking at first which led to entry and exit of unauthorized people in the quarantine facilities. We supported Masindi District to respond to the outbreak including conducting epidemiological investigations and setting up and managing of quarantine centers to interrupt further transmission of the virus into the communities. In this article, we describe how the quarantine centres were set up and managed in order to interrupt the spread of the disease to the rest of the community members.
Methods
Set up and management
The Masindi District Task Force identified two schools (Masindi Public School and Kabalega Secondary School) which had the potential of being used as quarantine facilities. We assessed the schools for suitability to accommodate the contacts based on the provisions of the National Quarantine Guidelines of the Ministry of Health. According to the Uganda National Quarantine Guidelines, quarantine centers should have adequately ventilated spacious rooms in which beds could be placed atleast 1 metre apart; adequate food, water, and hand hygiene provisions for the quarantine period; toilet, bathrooms and waste disposal facilities; provision for regular cleaning and disinfection of the rooms, toilets and bathrooms; possibility for daily follow up of quarantined persons; and security measures. We liaised with the area police and military personnel to help with enforcement and ensured quarantined persons stayed in the facilities throughout the 14-day period. The security personnel also ensured that unauthorised people do not get into and out of the quarantine facilities. In addition, we developed registers which were given to the security personnel at the entrance/exit of the facilities for easy monitoring of the people entering the facilities. We checked the temperatures and monitored development of symptoms of the quarantined persons on a daily basis. All the details of the individual quarantined person were recorded using contact follow up forms. Appropriate samples of all quarantined persons (Oral-pharyngeal swabs) were collected and sent to the Uganda Virus Research Institute (UVRI) for testing. These samples were collected twice during the quarantine period, i.e. at the beginning and of the quarantine period (day 1 and day 13) to ensure none of them is discharged with the disease. We provided psychosocial support by visiting every quarantine facility at least twice a week and explained to the quarantined persons how COVID-19 is transmitted and the rationale of their quarantine. We also taught them good personal hygiene practices and measures to minimise contact with other quarantined persons. We ensured availability of transport to the hospital just in case anyone of the quarantined persons had developed a fever and other COVID-19 related symptoms or even other illnesses.
While in the quarantine, we ensured all residents were provided with three meals a day; i.e.; Breakfast, lunch and dinner as well as adequate safe drinking water
Achievements
A total of four institutional quarantine centres were set up and 125 persons who had been in direct contact put in quarantine. We relocated and redistributed contacts to the newly set up centers in order to adhere to the holding capacity given the space and other facilities. The setting up of new institutional quarantine facilities helped to reduce on the number of people accommodated in the respective facilities and this in turn facilitated maintenance of the recommended space and a distance of 1 metre between beds in the rooms. Adequate hand washing facilities provided in all the quarantine facilities prevented crossing of contacts from one wing to another to search for the same; hence there was no mixing. Separate toilet and bathroom facilities (for males and females) also prevented sharing by the different sexes. Waste bins were provided and placed adjacent to each room to ensure that there was no littering and a clean environment could be maintained. In addition, all the rooms were cleaned and disinfected twice every day, which provided a clean and friendly environment for the quarantined persons to stay. Daily follow up of quarantined persons was achieved which involved checking their temperatures and monitoring them for development of COVID-related symptoms. All quarantine facilities were enclosed in fences to ensure security of the quarantined persons and at the same time, the area Police and Military personnel were deployed for enforcement.
Lessons learnt
The district needed prior knowledge on the standard requirements for quarantine facilities including location, number to hold given the space among others.
There is need for the Ministry of Health to assess all quarantine centres in the country for suitability to accommodate contacts/suspects.
Psychosocial support and provision of appropriate environment keeps the quarantined persons happy which in turn leads to adherence to quarantine rules and regulations and easy management.
Record keeping is vital in quarantine management as it enhances proper monitoring of the quarantined persons while in the facility.
Collaboration with other stakeholders such as Security is critical in the management of institutional quarantines to enforce adherence to quarantine rules and regulations.
Challenges
The greatest challenge during the interventions was the limited financial resources in the district budget which delayed setting up of the required facilities such as hand washing facilities and establishment of water collection points in the quarantine
Conclusion
By the end of the response to COVID-19 outbreak in Masindi District, we had established and functionalized 4 institutional quarantine facilities and followed up 125 contacts.
The overall management improved characterized with less congestion in the facilities, proper record keeping was achieved, strengthened security, and appropriate use of hygiene facilities.
References
- Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19) Interim guidance –World Health Organization: 19 March 2020
- Guidelines on Quarantine of Individuals in the Context of Containment of Coronavirus Disease (COVID-19) in Uganda Version 2.824 April 2020
Sustained Vigilance, Preparedness, and Response to All Public Health Emergencies amidst COVID-19 Pandemic
By Sandra Nabatanzi
Uganda Public Health Fellowship Program, Kampala, Uganda
Introduction
The COVID-19 pandemic has disrupted economies not only in Uganda but the entire World. The health system too has been affected. In Uganda, there were 685 cumulative COVID-19 cases as of 13 June 2020 (1). Unfortunately, there have been 234 community cases reported in 33 districts despite stringent measures put in place by Government of Uganda to avoid spread of COVID-19. (Figure 1). Additionally, 27 health workers had also been infected by COVID-19 but no deaths reported.
During the COVID-19 Pandemic, the number of malaria cases reported at the health facilities has increased by 56% between January and April 2020. Over 70 districts have experienced surges in malaria cases. Health facility deliveries have decreased by 10% while antenatal care (ANC) 4
attendance decreased by 7% between March and April 2020 compared to the same period, last year. The immunization coverage for DPT-1, DPT-3, Polio 3, Measles, and PCV-3 dropped from December 2019 and has remained below the target of 95%. The low reporting rate may have led to the reduction in coverage of immunization during the same period. During the month of March, immunization coverage levels were below 70%. Between February and March 2020, there was a 3% reduction in the number of HIV tests conducted. March had the lowest number of HIV tests conducted this quarter. This may partly be attributed to the movement restrictions that have affected both health providers and patients. Testing yield reduced to 2.4% in March compared to 3.0% of the previous month.
The above identified gaps among many others are possibly due to the effects of COVID-19 on the health care system. A strained health care system increases Uganda’s vulnerability to suffer from other public health emergencies including Cholera, Measles, other immunizable preventable disease, Crimean Congo Hemorrhagic Fever among other diseases of epidemic potential.
In 2020, Uganda has so far reported public health emergencies of COVID-19, West Nile Virus Fever, Crimean Congo Haemorrhagic Fever, Rift Valley Fever, Yellow Fever, Cholera, Rubella, Measles, and floods (Table 1).
| Table 1: Public Health Emergencies in Uganda, January – June 2020Dates | Location | PHE | Cumulative | Confirmed | Deaths |
| 04Mar20 | Moyo | West Nile Virus Fever | 01 | 01 | 00 |
| 31Mar20 | Uganda | COVID-19 | 724 | 724 | 00 |
| 10Feb20 | Kampala | Rift Valley Fever | 01 | 01 | 00 |
| 28Feb20 | Kiboga | Rift Valley Fever | 01 | 01 | 01 |
| 21Jan20 | Kagadi | Crimean Congo Hemorrhagic Fever | 01 | 01 | 00 |
| 10Dec19 | Buliisa | Yellow Fever | 24 | 03 | 01 |
| 21Jan20 | Moyo | Yellow Fever | 10 | 04 | 06 |
| 07Feb20 | Maracha | Yellow Fever | 01 | 00 | |
| 20Jan20 | Busia | Cholera | 10 | 01 | 00 |
| 09Jan20 | Nakaseke | Rubella | 05 | ||
| 13Jan20 | Multiple districts | Measles | |||
| 27Apr20 | Moroto | Cholera | 377 | 00 | |
| 22May20 | Nabilatuk | Cholera | 419 | 10 | 00 |
In November 2019, the Ministry of Health conducted a country wide mass measles-rubella vaccination campaign in order to protect susceptible individuals, interrupt transmission, and protect against measles outbreaks in Uganda. This campaign was successful with a coverage of 103%. However, the number of measles cases reported in 2020 is gradually increasing as indicated (Figure 2). The increasing cases call for an urgent need to intensify routine measles vaccination in the country.
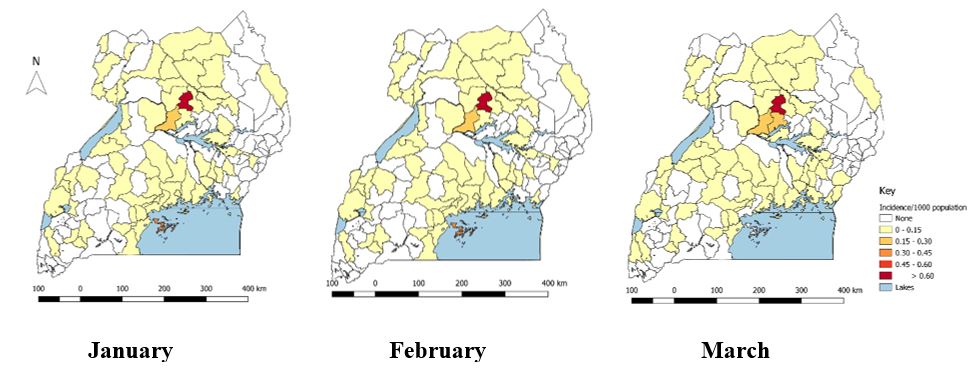
Figure 2: Trends of suspected measles cases in Uganda, 2020
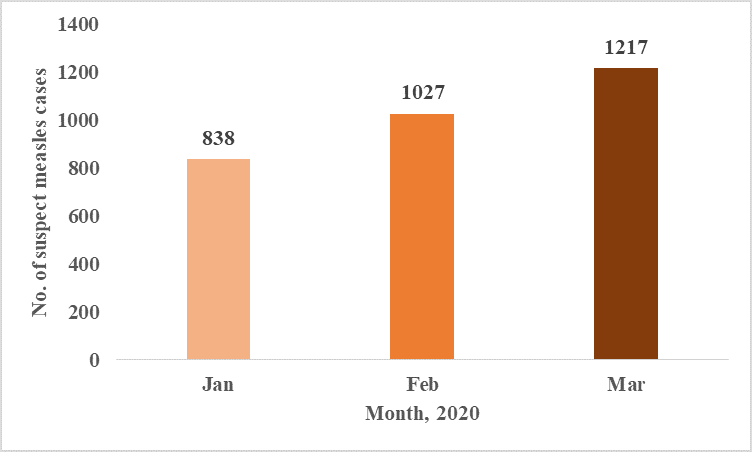
The overall cumulative incidence of suspected measles in Uganda was 9/1,000 population from January to March 2020. The most affected district was Kole District with a cumulative incidence of 2.1/1,000, followed by Apac (0.5), Kalangala (0.3), Kwania (0.3), Gulu (0.3) Obwongi (0.2). Iganga (0.2) and Lamwo (0.2). Over 85/135 districts have reported suspected measles cases in the months of January – March 2020 (Figure 3).
Neighboring countries like the Democratic Republic of Congo continue to battle with the biggest outbreak of Measles ever recorded. On 1 June 2020, the DRC also reported a new EVD outbreak in the Equateur Province. The 11th propagated EVD that affected Ituri and North Kivu, DRC and spilled to Uganda in June 2019 is not linked to current ongoing outbreak in Equateur Province. As 9 June 2020, a total of 12 cases and 8 deaths have been reported in Equateur Province (2).
Although the continuous occurrence of outbreaks of emerging and re-emerging infectious diseases in Uganda is likely primarily due to increased human interaction with forests, caves, and animals, geographic location in filovirus, meningitis, and yellow fever zones, effects of climate change – heavy rains and flooding, conflicts and population displacement in the Great Lakes region, and increased international movement of people among others, the effects of COVID19 on the health care system further increases Uganda’s vulnerability to outbreaks. There is critical need for enhanced vigilance for all PHEs during response to the COVID-19 Pandemic.
How can we maintain capacities built and vigilance to other PHEs amidst response to COVID-19?
Vigilance to all PHEs is critical and can be maintained through 1) Integrating preparedness and response activities for COVID-19 with all other emergencies; 2) Ensuring heightened surveillance and reporting in all districts; 3) Verifying all rumors and alerts and investigating all outbreaks in the country; 4) Decentralizing response mechanisms to district level to ensure efficiency; 5) Use COVID-19 as an opportunity to strengthen capacities to respond to PHEs at all administrative levels; and finally strengthen routine immunization by minimizing missed opportunities for vaccination at health facilities. Currently, Uganda National Expanded Programme on Immunization has encouraged District Health Officers to continue with static immunization at health facilities amidst COVID-19 Pandemic. However, due to the interference with immunization interventions in schools and communities (outreaches), the programme is developing a post recovery plan that will involve mass immunization of the highly affected pathogens.
Conclusion
Despite the stretched resources both human and financial, it is critical to integrate and decentralize response to other Public Health Emergencies with COVID-19. This will in turn enable quick detection and timely response which will avert deaths caused by other outbreaks aside COVID-19. The huge numbers of individuals affected will also cripple the fragile health system. Hence, it is important to be on high alert, rapidly detect, and respond to PHEs in the country.
References
- Ug_COVID-19_SitRep#119.pdf [Internet]. [cited 2020 Jun 22]. Available from: https://veoci.com/veoci/p/w/f/lz9vtf7eg84fnzkd/Ug_COVID-19_SitRep%23119.pdf
- SITREP_EVD_DRC_20200610-eng.pdf [Internet]. [cited 2020 Jun 16]. Available from: https://apps.who.int/iris/bitstream/handle/10665/332320/SITREP_EVD_DRC_20200610-eng.pdf
Rubella Outbreak among Vaccinated Children Propagated by Attending School X, Nakaseke District, Uganda, January 2020
Authors: Irene B. Kyamwine1*, Maureen Katusiime1, John Kamulegeya1, Benon Kwesiga1, Alex R. Ario1, Julie Harris2
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda,
2Centers for Disease Control and Prevention, Kampala, Uganda
Summary: On 10 January 2020, the Uganda National Expanded Program on Immunization was notified of five patients testing IgM-positive for rubella in Nakaseke District, Uganda. We investigated to determine the scope of the outbreak, identify transmission-related exposures, and recommend control and prevention measures. We defined a suspected case as fever and maculopapular rash, or suspicion of measles/rubella by a healthcare worker, in a resident or visitor of Semuto sub-county, Nakaseke District from 1 October 2019 to 2 March 2020. A confirmed case was a suspected case positive by rubella-specific IgM. We reviewed health facility records and conducted active community case-finding. In a case-control study, we compared potential exposures between 18 case-patients and 72 asymptomatic village- and age-matched controls. We identified 21 suspected case-patients, five confirmed (no deaths). The overall sub-county attack rate (AR) was 7.8/10,000. Males (AR=10/10,000) were more affected than females (AR=4.8/10,000). All case-patients were from a single parish. Seventeen (94%) case-patients received the MR vaccine in October 2019, a median of 61 days (range: 8-96) before symptom onset. The vaccine lot used in the affected parish was also used in other unaffected sub-counties. Vaccination was not associated with illness (OR(M-H)=3.0, CI: 0.41-22). Eight (44%) case-patients and 12 (17%) control-persons attended School X (OR(M-H)=3.9, CI: 1.2-12). We concluded that the recent rubella vaccination was ineffective in preventing this outbreak. This outbreak was likely propagated by patients mixing with other children attending School X. We recommended intensifying sensitization of communities and schools on rubella transmission and prevention and evaluation of the recent MR vaccine potency, vaccine storage and cold chain before more of the same vaccine is administered.
Background: Rubella is an acute viral infection transmitted by airborne droplets. It is less contagious than measles. The average incubation period for rubella is 14 days but can range from 12–23 days (1). Rubella causes a mild disease characterized by a rash, fever, arthritis and joint pain among children and adults(2). Rubella is diagnosed by detection of rubella specific IgM or Ig G antibody, positive viral culture for rubella or detection of rubella virus by polymerase chain reaction (PCR) from nasal, blood, throat, urine and cerebrospinal fluid specimens (1). Rubella infection is vaccine preventable. Following vaccination Ig M and Ig G antibodies develop within 2 weeks. However, I g M antibodies quickly fade away to almost undetectable after 2 months of vaccination (1). Despite the availability of the rubella containing vaccine since 1969 Uganda introduced a rubella‐containing vaccine into the routine schedule in October 2019 following measles-rubella outbreaks in the country in 2018 (1)(3). In Uganda, all suspected measles cases tested for anti-measles are also tested for antirubella immunoglobulin M (IgM) antibodies (4).
On 10 January 2020, Uganda Ministry of Health (Uganda National Expanded Program on Immunization) received notification of 5 patients testing Rubella IgM positive. We investigated to determine the scope of the outbreak, exposure risk factors, estimate vaccine effectiveness and vaccination coverage, and guide evidence-based control measures.
Methods: We defined a suspected case as a fever and maculo-papular rash, or a health care worker suspicion of measles in a resident or visitor of Semuto sub-county, Nakaseke District from 1 October, 2019 onwards; a confirmed case as a suspected case with a positive blood test for rubella-specific Ig M. We reviewed health facility records and conducted active case finding. We performed descriptive analysis of the cases and developed hypotheses. We conducted a case control study to identify exposures for transmission. We estimated rubella vaccination coverage (VC) using the percent of control-persons vaccinated assuming that the controls were representative of the general population.
Results: We identified 21 suspected cases in Semuto sub-county, 5 of whom were confirmed. The sub-county attack rate [AR] was 7.8/10,000 persons and no death. The epidemic curve shows a propagated outbreak (Figure 1).
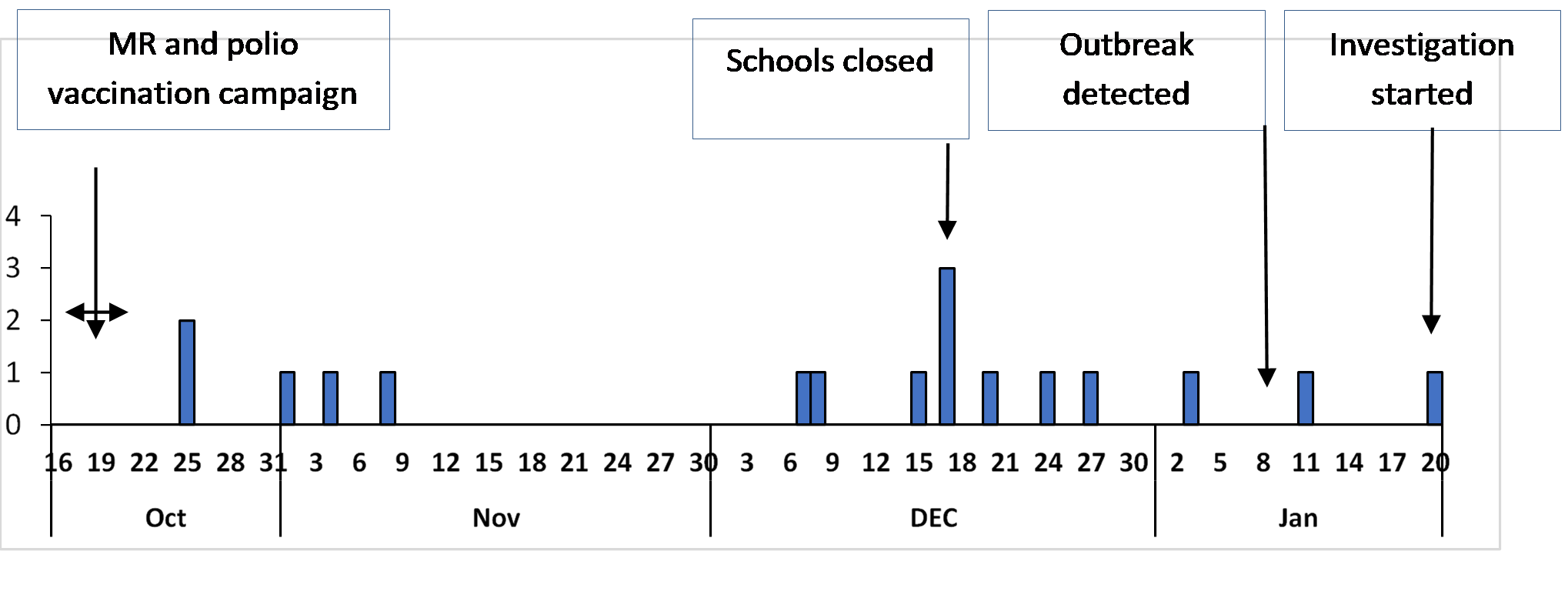
Median age was 5 years (Range: 1-15 years). Age-group 9 months-<15 years had the highest proportion of cases (20), >15 years had only one case and the age-group <9 months did not have any cases. Males (AR: 10/10,000) were more affected than females (AR: 4.8/10,000). Segalye parish was the only parish affected in Semuto sub-county. Nvunaanwa (20 cases) and Kalege (1 case) were the only villages affected in the parish. Attending school X was associated with rubella infection among 8 (44%) case-patients compared to 12 (17%) control-persons (OR(M-H)=3.9, CI: 1.2-12), (Table 1). The VC, estimated by the percent of control-persons who had a history of rubella vaccination, was 83%.
Table 1: Exposure status among Cases and Controls in a rubella outbreak, Semuto sub-county, Nakaseke District, January 2020
| Exposure | Number Exposed | Percent Exposed | Odds Ratio | 95%
CI |
||
| Cases | Controls | Cases | Controls | |||
| Attending school X | 8 | 12 | 44 | 17 | 3.9 | 1.2-12* |
| Contact with a person with febrile rash | 13 | 11 | 72 | 15 | 21 | 4.2-109* |
| Rubella Vaccination | 17 | 60 | 94 | 83 | 3.0 | 0.41-22 |
| Visiting public water source | 12 | 53 | 67 | 74 | 0.58 | 0.14-2.4 |
| Attending religious gatherings | 15 | 43 | 83 | 60 | 3.1 | 0.91-11 |
* Statistically significant OR
Discussion: Our investigation showed that attending school X was associated with rubella infection. The continuous transmission of rubella was likely propagated by school children continuing to attend school during illness, hence spreading the infection to others in class or during play time through sneezing and coughing at school. This finding is consistent with other studies conducted in Ethiopia and Chile where institutional outbreaks of rubella were registered (5,6). Our finding is also biologically plausible considering that rubella is spread through respiratory secretions. Isolation of the case-patients at home could have stopped the spread of rubella to school going children (7). Therefore, during rubella outbreaks, schools and communities should be advised to isolate children with fever and rash from other children.
We also, found that children below the age of 15 years were the most affected. This finding is similar with earlier studies in Zimbabwe, Ethiopia and Kenya. Chimhuya, et al and Mitiku, et al both demonstrated that over 90% of the rubella cases were children <15 years (8–10). The mean age in our study was 6 years which is similar with findings in Zimbabwe (11). The high incidence of rubella cases among younger children could be attributed to lack of immunity that the older people may have acquired from infection. This therefore, calls for intensifying the MR vaccination to ensure that all children are vaccinated.
Contrary to other rubella outbreaks, in this investigation almost all the cases were vaccinated with rubella vaccine. However, the rubella infection acquired after vaccination cannot be passed on to other people hence the vaccine could not have been the cause of this outbreak (12). Rubella could have occurred among vaccinated children due to vaccine failure. The outbreak could have occurred because the children did not mount immunity against rubella which would have interrupted transmission. In study by US CDC in 1992-94, 8% of the vaccinees were found to lack serologic evidence of immunity to rubella (CDC, unpublished data) (13) which could be the case in our outbreak. Therefore, sero-epidemiologic studies of IgG levels are needed to assess rubella immunity among the vaccinated population. This outbreak also highlights the importance of a thorough epidemiologic and laboratory investigation of suspected cases of measles and rubella, regardless of vaccination status, as well as the need for active surveillance.
Conclusion: The recent rubella vaccination was ineffective in preventing this outbreak. This rubella outbreak was associated with contact with a case and likely propagated at School X. Ministry of Health should evaluate the recent MR vaccine potency, vaccine storage, and cold chain records before more of the same vaccine is administered. We also, recommended intensifying sensitization of communities and schools on rubella transmission and prevention.
References
- rubella.pdf [Internet]. [cited 2020 Feb 10]. Available from: https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/rubella.pdf
- manual_diagnosis_lab_mea_rubella.pdf.
- Statement from Uganda’s Minister of Health on the National Measles-Rubella and Polio Immunisation Campaign 2019 – Uganda [Internet]. ReliefWeb. [cited 2020 Feb 11]. Available from: https://reliefweb.int/report/uganda/statement-uganda-s-minister-health-national-measles-rubella-and-polio-immunisation
- Tushabe P, Bwogi J, Abernathy E, Birungi M, Eliku JP, Seguya R, et al. Descriptive epidemiology of rubella disease and associated virus strains in Uganda. J Med Virol. 2020 Mar;92(3):279–87.
Policy brief: Using malaria channels based on percentiles to detect malaria epidemics in Uganda
Phoebe Nabunya1
1Uganda Public Health Fellowship Program, Kampala, Uganda
Executive summary
The WHO recommends the use of malaria epidemic thresholds derived from routine data to detect malaria epidemics. Multiple methods are recommended for use when setting the thresholds depending on the context. The Uganda epidemic preparedness and response plan recommends two methods to set threshold. This has caused conflict in the alerts created as the various methods produce different threshold levels. Recommending a single uniform method for setting thresholds at all administrative levels would ensure that there is harmonization of epidemic detection among stakeholders at all levels of the health system. Epidemics are picked at the same time without any conflicts.
Introduction
Malaria prevalence has been declining over the years from 42% in 2009 to 19% in 2016 and now is at a prevalence of 9% (MIS, 2019).These gains are however under threat with increased occurrence of malaria epidemics as seen in 2015 and 2019. Traditionally, epidemic prone areas have been the highlands areas like in Kigezi, however, this has increased with scale back of interventions such as scale back of IRS that led to the 2015 epidemic in Northern Uganda. In addition, the declining prevalence has also increased the areas that are epidemic prone due to decreasing immunity of the population in these areas. To be able detect increases in the malaria cases, the WHO recommends the development and implementation of effective early detection system (EDS) for malaria epidemics by using routine data to determine thresholds for epidemics for specific regions (1).
One of the key roles of the EDS is to come up with thresholds for when a malaria epidemic is declared. The WHO recommends the setting of these thresholds using a “normal epidemic channel”, a term used to describe the normal seasonal pattern of malaria in an area. The weeks in which cases exceed the threshold are declared routinely as epidemic weeks (1-3).
Determining whether there is a malaria epidemic using these methods requires the availability of 5-10 year historical data, from which a baseline of normal occurrences and threshold values can be determined (4). There are four methods WHO recommends for setting thresholds namely, (i) constant case-count thresholds; (ii) mean number of malaria cases plus standard deviations; (iii) percentiles over the median; and (iv) cumulative sum (C-SUM). All the methods are expected to capture an epidemic when the cases exceed a given level of the usually reported cases from a minimum of 5 years in a specific area and time (3). Of these, the Uganda Emergency Preparedness and Response guidelines recommend the mean +2SD and 3rd Quartile, largely because the C-sum and case-count works better with a small case-count.
Context and importance of the problem
The existence of the HMIS system (mTRAC and DHIS2) enables Uganda to collect weekly data on presumed and confirmed malaria cases from health facilities in the country providing a representative weekly data set which gives more accurate thresholds thereby enabling early detection(4, 5).
The Uganda EPR guidelines propose the use of mean +2SD to generate a threshold for malaria epidemics at district level and using median and the third quartile at health facility level from a minimum of 5 year weekly data(3). The use of mean+2SD requires eliminating epidemic years or years of unusually low transmission to the calculation of means+2SD (4). Unusual numbers could be due to seasonal variation, data quality, and scale up or down of interventions (6). In contrast, the percentile is able to accommodate the years with abnormally high incidence making it possible to use all the available data in the country (4, 7).
During the 2019 outbreak, malaria channels drawn using the percentile method were able to detect out breaks which had been missed by the mean +2SD. This created conflict at the districts during the response as some districts did not perceive the epidemic from the normal channels they had been monitoring. In the past five years, Uganda has experienced malaria epidemics in several parts of the country in 2015, 2016, and 2019 (8-10). This would render 3 years from the recommended 5 years historical data unsuitable for setting the thresholds when using mean +2SD as including them would overestimate the thresholds. This could explain why some malaria normal channels constructed at the district using mean +2SD did not pick the malaria epidemics picked when using percentiles. A validity study of the mean and Percentiles done in Sudan, which also has seasonal transmission of malaria found channels from percentiles to be more sensitive. Several studies done in African countries with a high burden of malaria have also found percentiles more effective in detecting epidemics compared to the mean (4).
The use of both percentiles and mean to set the thresholds also possess chances of disagreements in the alert threshold as the percentiles have consistently been found to produce lower cutoffs compared to the mean. The mean is also affected by skewed data which can possibly lead to false alarms or missed outbreaks and has been found to be generally less sensitive(4).
It is important for Uganda to have clear guidelines on which method to use when setting thresholds in order to detect the malaria outbreaks in a uniform and timely manner. Malaria epidemics have important impacts on health and the economy as time and finances are lost in treatment if not detected and mitigated early. The detection of these outbreaks is also very important now that the prevalence of malaria in the country has reduced and some areas including Kampala and Kigezi region have a very low burden of the disease making them epidemic prone (11, 12).
Critique of policy options
The EPR guidelines recommend the use of means+2SD and percentiles at different administrative points in the health system. This creates conflicts in the making of alerts as the mean+2SD are generally less sensitive compared to percentiles. Timely response which heavily relies on EDS detecting the epidemics early, a uniform method for setting thresholds at all levels would ensure uniformity in decision-making and action at the national, district, and local level.
Furthermore, the EPR guidelines don’t recommend the elimination of epidemic years yet Uganda has reported outbreaks in 2015 and 2019 which would lead to over estimation of the threshold(13, 14).
Despite the recommendation to have the malaria channels monitored at all levels from health facility to national level, the employment structure only allows for biostaticians at district level. All health facilities select HMIS focal persons who could be clinical officers, nurses, or laboratory staff. These carry out this role alongside their routine work which interferes with the routine construction of the channels.
Recommendations
As we move towards 2030, where Uganda hopes to have eliminated malaria, there is need to: 1) Recommend the use of percentiles as the universal method for setting thresholds for detecting malaria epidemics in the country right from the national, district, to heath facility level so as to ensure similar thresholds at all times. The health facilities can maintain the manual method of setting thresholds since most don’t have a computer. 2) Epidemic years should be removed from the historical data that is used to set epidemic thresholds in the malaria channel. This will ensure that only a true increase in cases from
those expected are detected and responded to. 3) Since majority of the districts in the country surpass the 75th percentile each year which restricts response due to limited resources, two thresholds; an alert threshold (75th percentile) and an epidemic threshold (85th percentile) can be set. The alert threshold once surpassed should initiate the country to assess its epidemic preparedness, assess ability to respond, provide an early warning. 4) There is also need to boost the capacity of health facilities with human resource with skills able to make and interpret the malaria channels. 5) Deaths and admissions should be monitored alongside the malaria cases reported. This can inform launching of an investigation at the start of the epidemic and inform prioritization of areas for intensified control measures in the event of an epidemic. 6) As the cases recorded decline, the low burden districts in Kigezi region can adopt, the case-count method for setting epidemic threshold. This would confirm the emergence of an epidemic early so that control measures such as health education, and case-management, can be intensified.
References
- WHO. Eliminating malaria. World Health Organization, 2016.
- WHO. Disease Surveillance for Malaria Elimination: An operational manual. 2012.
- WHO. Field guide for malaria epidemic assessment and reporting: Draft for field testing. Geneva: World Health Organization, 2004.
- Guintran J-O, Delacollette C, Trigg PI, WHO. Systems for the early detection of malaria epidemics in Africa: an analysis of current practices and future priorities. Geneva: World Health Organization, 2006.
- MOH. Uganda’s Electronic Health Information System/DHIS 2. 2019.
- MOH. GUIDELINES FOR PREPAREDNESS AND RESPONSE FOR MALARIA EPIDEMICS. 2012. p. 30-5.
- WHO. Malaria surveillance, monitoring & evaluation: a reference manual. WHO Press, World Health Organization. 2018.
- M.K. M, A. K, P. A, P. N, B. O, M. A, et al. Intermittent preventive treatment with dihydroartemisinin piperaquine in young Ugandan children in the setting of indoor residual spraying of insecticide. American Journal of Tropical Medicine and Hygiene. 2018.
- Raouf S, Mpimbaza A, Kigozi R, Sserwanga A, Rubahika D, Katamba H, et al. Resurgence of Malaria Following Discontinuation of Indoor Residual Spraying of Insecticide in an Area of Uganda With Previously High-Transmission Intensity. Clinical Infectious Diseases. 2017:6-8.
- Tukei BB, Beke A, Figueroa HL. Assessing the effect of indoor residual spraying ( IRS ) on malaria morbidity in Northern Uganda : a before and after study. Malaria Journal. 2017:1-9.
- Uganda Malaria Indicator Survey Preliminary Report 2017-2018, (2018).
- UBOS, editor Uganda Malaria Indicator Survey 2014-152015.
- NMCD. Malaria Quarterly Bulletin Issue 28: 1 January 2019– 31 March 2019. 2019. p. 1-7.
- Raouf S, Mpimbaza A, Kigozi R, Sserwanga A, Dorsey G. Resurgence of malaria after discontinuation of indoor residual spraying of insecticide in a previously high transmission intensity area of Uganda. The Lancet Global Health. 2016.
Read and Download full pdf below;

Comments are closed.