Trends of anemia in pregnancy and uptake of prevention measures during antenatal care, Uganda, 2020-2024
Authors: Lubega Janet Kobusinge1*, Richard Migisha1, Benon Kwesiga1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program-Field Epidemiology Training Program, Uganda National Institute of Public Health, Kampala, Uganda Correspondence*: Tel: +256 772 773664896, Email: jklubega@uniph.go.ug
Summary
Background: Anemia remains a significant health challenge in Uganda, particularly for pregnant women, leading to complications like maternal mortality and preterm births. Despite Ministry of Health guidelines for free antenatal services, including iron and folic acid supplementation, 23%-37% of pregnant women remain anemic. We analyzed trends in anemia and the uptake of anemia prevention services, Uganda, 2020–2024 to inform programming.
Methods: We analyzed DHIS2 data on ANC1 and ANC4 visits in Uganda between 2020 and 2024. Anemia was defined as hemoglobin levels below 10 g/dL. We also calculated the percentage uptake of iron/folate supplements (IFA), intermittent preventive therapy (IPT), and long-lasting insecticidal nets (LLINs). Trends were assessed using the Mann-Kendall test at p < 0.05.
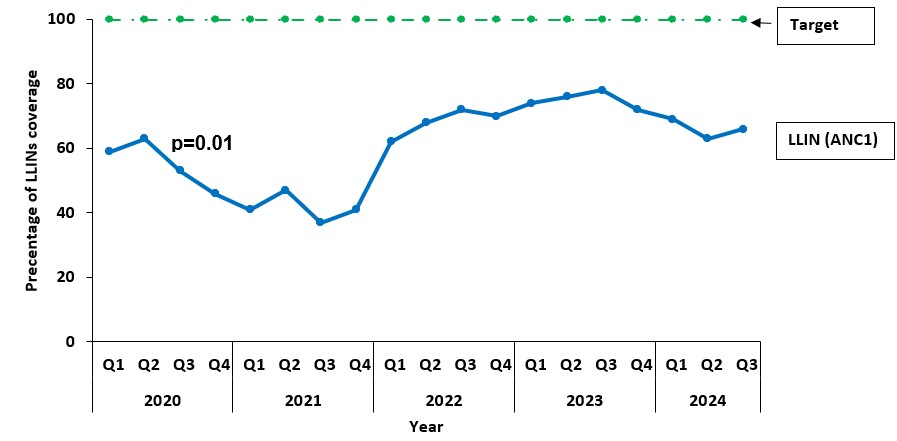
Results: Anemia prevalence at ANC4 significantly declined from 20% in 2020 to 10% by 2021 (p = 0.001), while ANC1 prevalence remained stable at 7% to 10%, both above the 5% target. Screening coverage at ANC4 improved significantly from 14% in 2020 to 25% in 2024 (p = 0.001), whereas ANC1 coverage increased modestly from 5% to 9% (p = 0.14). IFAS coverage consistently exceeded the 65% target, ranging from 67% to 70%, though variability was observed at ANC4 (p = 0.1). IPT1 coverage declined significantly from 98% in 2020 to 75% in 2024 (p = 0.001), while IPT3 averaged 56% and remained below the 66% target (p = 0.29). LLIN distribution improved significantly from 59% in 2020 to 66% in 2024 (p = 0.01) but remained below the 100% target.
Conclusion: Anemia rates declined from 2020 to 2024, with significant trend observed in the prevalence of anemia and screening at ANC4. Strengthening prevention measures including IFA, IPT, and LLIN uptake, is crucial to addressing anemia, particularly in high-burden regions. Further studies are needed to understand factors driving high anemia prevalence at the district level.
Introduction
Anemia remains a major public health challenge, with the highest burden observed in low- and lower-middle-income countries such as Uganda. It disproportionately affects vulnerable populations, including young children, menstruating adolescent girls, pregnant, and postpartum women (1, 2). Anemia in pregnancy, defined by hemoglobin levels below 11g/dL, compromises the oxygen-carrying capacity of blood and increases the risks of maternal and perinatal morbidity and mortality, preterm birth, low birth weight, and complications such as cardiac failure and postpartum hemorrhage (3) (4).
In Uganda, with the 2018 UDHS reporting that 32% of women aged 15-49 are anemic (7). Among pregnant women, a pooled prevalence of 43.2% was observed from UDHS data between 2006-2016(8). Anemia rates were higher in rural areas (33%) than urban areas (27%), with regional variation ranging from 17% in Kigezi to 47% in Acholi(9).
The Uganda Ministry of Health (MoH) has established guidelines to prevent and manage anemia in pregnancy, as recommended by the World health Organization (WHO), a minimum of eight ANC contacts for pregnant women. Additionally, promoting routine iron and folic acid supplementation (IFAS), intermittent preventive treatment for malaria (IPTp), and distribution of long-lasting insecticidal nets (LLINs) (10) (11, 12) (3). Despite this, adherence to this guideline in Uganda remains suboptimal. Many women attend fewer than the recommended number of ANC visits, limiting their access to essential preventive services such as anemia screening, iron supplementation, and malaria prophylaxis (13). This indicating ongoing challenges in healthcare delivery and adherence to treatment protocols. While the intervention package has clear goals, understanding its uptake over time and evaluating its effectiveness in reducing anemia prevalence among pregnant women is critical. Previous studies assessing anemia prevalence among pregnant women have relied primarily on survey data from specific districts or regions. However, none have utilized the comprehensive District Health Information System (DHIS2) datasets to explore nationwide trends in anemia and the associated prevention interventions. This study addressed this gap by providing a detailed analysis of anemia in pregnancy, focusing on its prevalence, trends, as well as the uptake and trends of prevention measures provided during antenatal care (ANC) from 2020 to 2024.
Methods
We conducted a descriptive analysis of anemia trends and the uptake of prevention services (iron and folic acid supplementation, long-lasting insecticidal net distribution, and intermittent preventive treatment with fansidar) among pregnant women attending their first antenatal visit (ANC1) and fourth antenatal visit (ANC4) antenatal care visits, Uganda, 2020-2024. We utilized anemia and anemia-prevention services surveillance data from Uganda’s District Health Information Software version 2 (DHIS2), managed by the Ministry of Health.
Data on anemia prevalence and uptake of preventive services were extracted from DHIS2 and analyzed using Microsoft Excel and STATA 16. Indicators were summarized and disaggregated by period for ANC1 and ANC4 to evaluate trends over time. Data was analyzed quarterly rather then annually to capture higher frequency, allowing for finer resolution in trend identification, better detection of seasonal variations, short-term fluctuations, and emerging patterns that might be obscured in annual aggregates.
From the total ANC attendance, we identified those tested for anemia and calculated the proportion diagnosed with anemia with those having a hemoglobin concentration level of less than 10 g/dL. The data was then disaggregated into quarters. Anemia was then classified into public health significance categories ranging from severe to normal(14). Uptake of iron and folic acid supplementation (IFAS), intermittent preventive treatment (IPT), and insecticidal net distribution was calculated separately for ANC1 and ANC4. For IFAS, the percentage was determined by dividing the number of women who received supplementation at ANC1 or ANC4 by the total number of ANC visits at the respective stage. IPT was calculated as IPT1 and IPT3, where IPT1 was determined by dividing the number of women who received the first dose of IPT at ANC1 by the total ANC1 visits, and IPT3 was calculated as the number of women who received the third dose of IPT divided by the total number of ANC1 visits. For insecticidal net distribution, the percentage was obtained by dividing the number of women who received nets at ANC1 or ANC4 by the total number of ANC visits at the corresponding stage. These calculations reflect the proportion of women who accessed these interventions at specific points during their ANC visits. The percentage utilization of each intervention was compared to national targets. For anemia screening, the target was set at 65% at ANC1, while iron and folic acid supplementation (IFAS) aimed for 65% utilization at ANC1, Intermittent preventive therapy (IPT) targeted 66% utilization with a minimum of three doses, and long-lasting insecticidal nets (LLINs) were expected to achieve 100% distribution during ANC1 (15, 16).
To analyze trends in anemia prevalence and service uptake, the Mann-Kendall test was employed at a significance level of p < 0.05. Analyses were conducted for national-level data, providing insights into yearly variations and overall changes.
Our study utilized routinely collected aggregated program surveillance data that did not have any personal identifiers. We obtained permission to use the HMIS data from the Ministry of Health Resource Centre which has the overall mandate to collect and store health-related information. Additionally, the U.S. Centers for Disease Control and Prevention (CDC) Center for Global Health determined our study was non-research whose primary intention was to address public health problems. We stored data in password-protected computers and data was not shared with anyone outside the investigation team.
Results
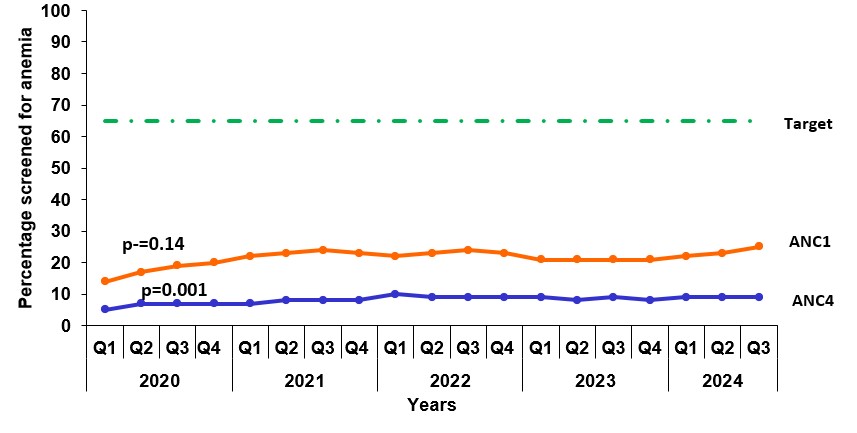
Trends of pregnant women screened for anemia at antenatal care 1 and antenatal care 4, Uganda, 2020-2024
From Quarter 1 2020 to Quarter 3 2024, anemia screening coverage averaged 21% at ANC1 and 8% at ANC4, falling significantly short of the 65% target throughout the period. At ANC1, screening rose from 14% in Q1 2020 to 25% by Q3 2024, while ANC4 screening increased from 5% to 9% but remained consistently lower than ANC1. A statistically significant upward trend was observed for ANC4 screening (p = 0.001), whereas the trend for ANC1 was not significant (p = 0.14) (Figure 1).
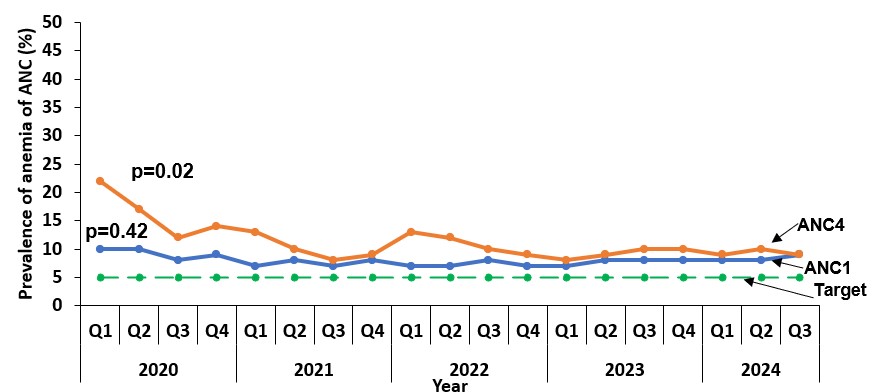
Trends for prevalence of anemia in pregnancy at antenatal 1 and antenatal 4, Uganda, 2020-2024
The average prevalence of anemia was 9% at ANC1 and 13% at ANC4, consistently still above the 5% target throughout the study period. At ANC1, prevalence remained relatively stable, starting at 10% in Q1 2020 and slightly declining to 9% in Q3 2024. In contrast, ANC4 prevalence significantly declined from 22% in Q1 2020 to 10% by Q2 2021, stabilizing thereafter at around 9% by Q3 2024. The decline at ANC4 was statistically significant (p = 0.02), while no significant change occurred at ANC1 (p = 0.42) (Figure 2).
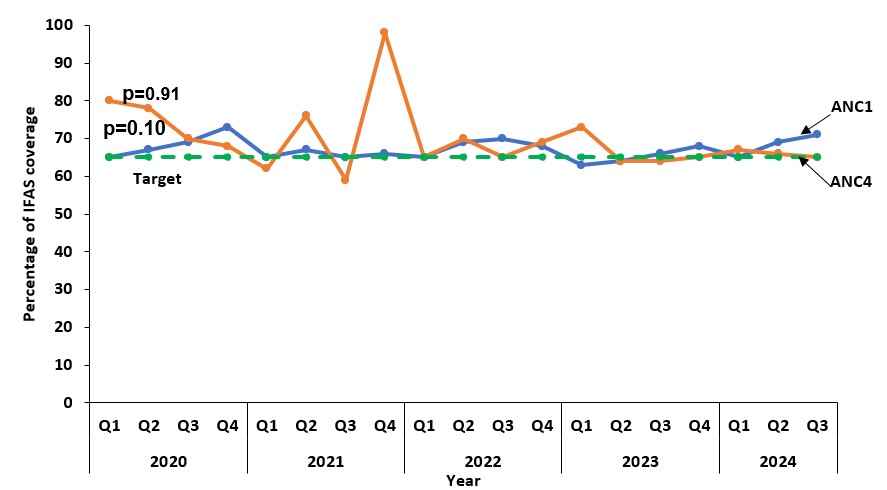
Trends of iron and folic acid supplementation coverage at antenatal care 1 and antenatal care 4, Uganda, 2020-2024
Quarterly trends in iron and folic acid supplementation (IFAS) uptake during ANC1 and ANC4 from Q1 2020 to Q3 2024 show that coverage was between 67% and 70% which consistently exceeded the national target throughout the study. ANC1 coverage rose steadily from 65% in Q1 2020 to 71% in Q3 2024, showing minimal fluctuations. ANC4 coverage started at 80% in Q1 2020, peaked at 98% in Q4 2021, and declined to 68% by Q3 2024, with notable variability. Neither trend was statistically significant (ANC1: p = 0.91; ANC4: p = 0.1) (Figure 3).
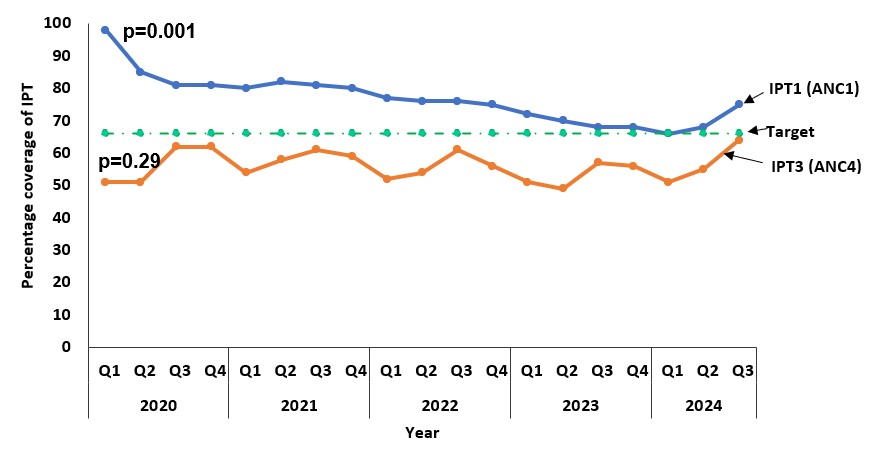
Trends of Intermittent Preventive Treatment coverage at antenatal care 1 and antenatal care 4, Uganda, 2020-2024
Quarterly trends in intermittent preventive treatment (IPT) coverage during ANC1 and ANC4 visits from Q1 2020 to Q3 2024 show that average IPT1 utilization was 77%, consistently exceeding the 66% target, while IPT3 utilization averaged 56% and never met the target. IPT1 coverage significantly declined from 98% in Q1 2020 to 75% in Q3 2024 (p = 0.001). IPT3 coverage increased from 51% in Q1 2020 to 64% in Q3 2024, but the trend was not statistically significant (p = 0.29) (Figure 4).
Trends of Long-Lasting Insecticidal Nets coverage at antenatal care 1 and antenatal care 4, Uganda, 2020-2024
The quarterly trends in the uptake of LLINs during ANC1 visits from Q1 2020 to Q3 2024. LLIN coverage started at 59% (282,096/480,831) in Q1 2020, and then declined to 37% (175,494/471,341) by Q3 2021. There was a notable increase to 66% (347,721,530,022) in Q3 2024. Overall, average LLIN utilization was 61%, falling below the 100% target. The distribution coverage showed a statistically significant increase (p = 0.01) indicating improvements over the study period (Figure 5).
Discussion
From 2020 to 2024, maternal health interventions in Uganda showed mixed progress. Anemia screening coverage remained below target, with improvements observed at ANC4, while anemia prevalence declined significantly only at later stages of care. Iron and folic acid supplementation consistently exceeded targets, but intermittent preventive treatment showed declining coverage for initial doses and unmet targets for subsequent doses. Long-Lasting Insecticidal Net distribution improved over time but still fell short of the target. These findings underscore the need for stronger efforts to meet maternal health objectives.
The prevalence of anemia among pregnant women in Uganda remains a significant public health concern. Higher anemia rates at ANC4 compared to ANC1 suggest reduced ANC attendance later in pregnancy, consistent with findings from Uganda and Ghana, where social, financial, and geographical barriers, along with knowledge gaps, limit access to care beyond initial visits (17, 18, 19). As a result, achieving the WHO recommended eight ANC visits is rare, with many women receiving far fewer than the recommended number.
Preventive measures such as iron and folic acid supplementation, IPT for malaria, and LLINs are critical in managing anemia. However, uptake of these interventions remains suboptimal. This study found that iron and folic acid supplementation never exceeded 75% coverage, and IPT coverage showed a downward trend over time. Low adherence to supplementation and IPT, along with inadequate dietary intake and malaria burden, especially in regions with high malaria transmission contributes to the anemia (26, 27, 28). The poor coverage of anemia prevention measures can be attributed to several factors, including inconsistent access to healthcare services, particularly in rural areas. Barriers such as healthcare access, long distances to facilities, financial constraints, and frequent stock-outs of supplements exacerbate the issue. Cultural beliefs, misconceptions, and inadequate health literacy further reduce adherence to preventive measures (27). Addressing these challenges requires improved healthcare access, consistent supply chains for preventive interventions, and enhanced community education to promote adherence to ANC recommendations. Strengthening these areas is essential for reducing anemia in pregnancy and improving maternal health outcomes (24, 26). Additionally, healthcare system inefficiencies, such as frequent stock-outs of essential supplements and commodities, further reduce access. Low health literacy, cultural beliefs, and misconceptions about the importance of these preventive measures also contribute to poor adherence, with healthcare providers sometimes failing to emphasize the importance of continued care and treatment adherence during ANC visits.
Addressing these gaps requires improving healthcare access and ensuring that pregnant women receive consistent and adequate testing and prevention measures throughout their pregnancy. Enhancing health literacy through community engagement and education campaigns can improve adherence to ANC recommendations. At the healthcare system level, strengthening supply chains to ensure the availability of key preventive interventions, such as iron/folic acid supplements and antimalarial prophylaxis, is critical to reducing anemia in pregnancy.
Study limitations
We utilized secondary data associated with missing data. This likely led to an underestimation of the magnitude of the study outcomes. A number of private health facilities do not report or inconsistently report data to the DHIS2. This also likely led to an underestimation of the magnitude of the study outcomes.
Conclusion
While anemia prevalence showed a declining trend, it still did not reach below the national target, indicating a persistent burden that requires intensified prevention and management efforts. The reduction in prevalence reflects the impact of ongoing interventions but underscores the need for continued focus on maternal anemia as a significant health risk.
Screening at ANC4 improved but remained sub-optimal, indicating the need to strengthen service delivery later in pregnancy. IPT1 coverage declined, pointing to challenges in early preventive care, while LLIN distribution increased but did not meet targets, highlighting gaps in accessibility. In contrast, IFAS coverage consistently exceeded the target, demonstrating the success of supplementation programs. These trends show progress in some areas while revealing critical gaps in achieving universal coverage for maternal health interventions.
Addressing these challenges will require enhanced service delivery, improved preventive care, and strengthened efforts to ensure comprehensive coverage of essential maternal health interventions throughout pregnancy.
Conflict of interest
The authors declare that they no conflict of interest
Authors’ contribution
JKL conceptualized the idea, analyzed and interpreted the data, and drafted the manuscript. a. RM, BK, LB, and ARA reviewed the bulletin for intellectual content.
Acknowledgements
We thank the staff of the Public Health Fellowship Program for the technical support and guidance offered during this study.
Copyright and licensing
All material in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission. However, citation as to the source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO. Anemia-Fact sheet 2023 [Available from: https://www.who.int/news-room/fact-sheets.
- Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. The Lancet Global Health. 2013;1(1):e16-e25.
- Organization WWH. The global prevalence of anaemia in 2011. Geneva; 2015.
- Edelson PK, Cao D, James KE, Ngonzi J, Roberts DJ, Bebell LM, et al. Maternal anemia is associated with adverse maternal and neonatal outcomes in Mbarara, Uganda. The Journal of Maternal-Fetal & Neonatal Medicine. 2023;36(1):2190834.
- Sun D, McLeod A, Gandhi S, Malinowski AK, Shehata N. Anemia in pregnancy: a pragmatic approach. Obstetrical & gynecological survey. 2017;72(12):730-7.
- Gebreweld A, Tsegaye A. Prevalence and factors associated with anemia among pregnant women attending antenatal clinic at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Advances in hematology. 2018;2018(1):3942301.
- Report UBoSP. Uganda Demographic and Health
Survey.
- Bongomin F, Olum R, Kyazze AP, Ninsiima S, Nattabi G, Nakyagaba L, et al. Anemia in Ugandan pregnant women: a cross-sectional, systematic review and meta-analysis study. Trop Med Health. 2021;49(1):19.
- Wasswa R, Kananura RM, Muhanguzi H, Waiswa P. Spatial variation and attributable risk factors of anaemia among young children in Uganda: Evidence from a nationally representative survey. PLOS Global Public Health. 2023;3(5):e0001899.
- Kiwanuka TS, Ononge S, Kiondo P, Namusoke F. Adherence to iron supplements among women receiving antenatal care at Mulago National Referral Hospital, Uganda-cross-sectional study. BMC research notes. 2017;10:1-6.
- Uganda Malaria Indicator Survey 2018-2019 [Internet]. Available from: https://www.dhsprogram.com/pubs/pdf/MIS34/MIS34.pdf.
- Organization WH. Guideline: Daily iron and folic acid
supplementation in pregnant women 2012.
- UBoS I. Uganda demographic and health survey 2016. Kampala, Uganda and Rockville, Maryland, USA. 2018.
- Organization WH. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization; 2011.
- Health Mo. Annual Health Sector Performance Report 2022/23. Kampala: Ministry of Health; 2023.; 2023.
- ICF UBoSUa. Uganda Demographic and Health Survey 2022: Key Indicators Report. Kampala, Uganda: UBOS, and Rockville, Maryland USA. 2022.
- Duodu PA, Bayuo J, Mensah JA, Aduse-Poku L, Arthur-Holmes F, Dzomeku VM, et al. Trends in antenatal care visits and associated factors in Ghana from 2006 to 2018. BMC Pregnancy and childbirth. 2022;22(1):59.
- Nachinab GT-e, Adjei CA, Ziba FA, Asamoah R, Attafuah PA. Research Article Exploring the Determinants of Antenatal Care Services Uptake: A Qualitative Study among Women in a Rural Community in Northern Ghana. 2019.
- Wilson M, Patterson K, Nkalubo J, Lwasa S, Namanya D, Twesigomwe S, et al. Assessing the determinants of antenatal care adherence for Indigenous and non-Indigenous women in southwestern Uganda. Midwifery. 2019;78:16-24.
- Mahamoud NK, Mwambi B, Oyet C, Segujja F, Webbo F, Okiria JC, et al. Prevalence of anemia and its associated socio-demographic factors among pregnant women attending an antenatal care clinic at Kisugu Health Center IV, Makindye Division, Kampala, Uganda. Journal of blood medicine. 2020:13-8.
- Zerfu TA, Baye K, Faber M. Dietary diversity cutoff values predicting anemia varied between mid and term of pregnancy: a prospective cohort study. Journal of Health, Population and Nutrition. 2019;38:1-9.
- Wilunda C, Massawe S, Jackson C. Determinants of moderate‐to‐severe anaemia among women of reproductive age in T anzania: Analysis of data from the 2010 T anzania demographic and health survey. Tropical Medicine & International Health. 2013;18(12):1488-97.
- Nankinga O, Aguta D. Determinants of Anemia among women in Uganda: further analysis of the Uganda demographic and health surveys. BMC public health. 2019;19(1):1757.
- Obai G, Odongo P, Wanyama R. Prevalence of anaemia and associated risk factors among pregnant women attending antenatal care in Gulu and Hoima Regional Hospitals in Uganda: A cross sectional study. BMC pregnancy and childbirth. 2016;16:1-7.
- Udho S, Nankumbi J, Namutebi M, Mukunya D, Ndeezi G, Tumwine JK. Prevalence of anaemia in pregnancy and associated factors in northern Uganda: a cross-sectional study. South African Journal of Clinical Nutrition. 2023;36(4):136-41.
- Dickson KS, Boateng EN, Adde KS, Ameyaw EK, Munro-Kramer ML. Non-adherence to WHO’s recommended 8-contact model: geospatial analysis of the 2017 Maternal Health Survey. BMC Pregnancy and Childbirth. 2023;23(1):192.
- Uldbjerg CS, Schramm S, Kaducu FO, Ovuga E, Sodemann M. Perceived barriers to utilization of antenatal care services in northern Uganda: a qualitative study. Sexual & Reproductive Healthcare. 2020;23:100464.
- Gebremichael TG, Welesamuel TG. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: Cross-sectional study. PLoS One. 2020;15(1):e0227090.


Comments are closed.