Trends and Treatment Outcomes of Pediatric Tuberculosis, Mbale Regional Referral Hospital, Uganda, 2013-2017
Authors: Fred Monje1, Daniel Kadobera1, Lilian Bulage1, Alex Riolexus Ario1; Affiliations: 1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda
Summary
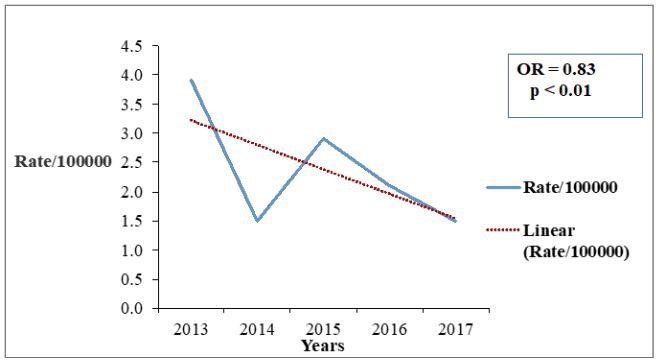
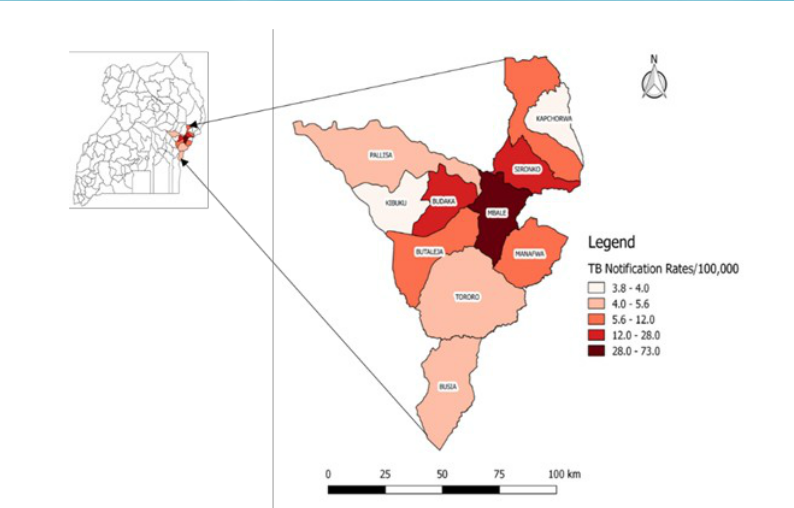
Neglected or missed Childhood TB often leads to missed opportunities for diagnosis, treatment, and prevention of transmission. We assessed trends in TB case notification rates, TB spatial distribution, TB treatment outcomes, and factors associated with completion of TB treatment in Children at Mbale Regional Referral Hospital (MRRH), East-ern Uganda. We identified 344 TB case notifications aged 0-14 years at MRRH; overall prevalence of 12 TB cases/100,000 population. The trend of TB case notification rates decreased from 3.9/100,000 in 2013 to 1.5/100,000 in 2017 (OR=0.83, p < 0.001). TB patients originated from 11 districts in Eastern Uganda. TB treatment completion was at 52% (179/344). In logistic regression, 67% (118/175) TB patients who resided ≤20km away from the hospital completed TB treatment com-pared to 36% (61/169) of TB patients who resided > 20km away from the hospital (AOR =3.3; 95%CI: 2.1-5.2). Childhood TB treatment completion rate was below the WHO recommendation of 85%. Better TB completion rate was associated with TB patients residing < 20km from the Hospital. To improve completion of TB treatment, MRRH should consider designing a means of follow up of TB patients who transfer out due to long distance to ensure they complete TB treatment in the scheduled period. Ministry of Health may open up more treatment facilities at lower levels closer to communities. Ministry of Health should consider educating communities on the importance of completing TB treatment.
Introduction
According to the Uganda National Tuberculosis and Leprosy Pro-gram (NTLP), children (0-14 years) are among the high risk groups for TB. Tuberculosis in children is often neglected by various professionals because children are hardly infectious and rarely develop severe TB disease (1). Unavailability of resources makes accurate diagnosis of childhood TB cases even more difficult, which leads to both un-diagnosed and under reporting of childhood TB (1). This dilemma of childhood TB will continuously provide a source for new TB infections in the population (1). Each missed TB case spreads TB to 10-15 people. Even the children who are correctly diagnosed as having TB, their treatment outcomes vary from region to region in Uganda (2). We assessed the trends in TB case notification rates, TB spatial distribution, TB treatment outcomes, and factors associated with completion of TB treatment in children at Mbale Regional Referral Hospital (MRRH), Eastern Uganda to guide control interventions.
Methods
We conducted a retrospective cohort study at MRRH. We re-viewed secondary TB data that’s routinely collected within the catchment area of MRRH in Eastern Uganda. We enrolled and reviewed records of all patients aged 0-14 years in the TB register at MRRH whose place of residence was among the Eastern districts of Uganda during the period 2013-2017. We excluded pediatric patients whose outcome of interest was missing.
We captured variables of TB patients from the TB registers such as patient residence (≤ 20km from MRRH or ≥20km away from MRRH), age (0<5; 5< 10; and 10< 15 years), sex, type of patient (patient continuing with TB treatment or patient newly initiated on TB treatment ), TB classification (PCD, EP and PBC), HIV status (positive or negative), treatment model (facility based treatment model or not), and treatment outcome (completed TB treatment or not). We computed the TB case notification rate (/100,000) for the period 2013 – 2017; performed a trend analysis of childhood TB and used QGIS to draw an area map to show the spatial distribution of childhood TB cases based on their recorded areas of residence. We used the estimated population of children from the hospital records of the catchment districts in Eastern Uganda to calculate the TB notification rate. We used logistic regression to identify predictors of completion of childhood TB treatment.
Results
We identified 344 TB case notifications aged 0-14 years at MRRH, 2013-2017; overall prevalence of 12 TB cases per 100,000 population. The trend of TB case notification rates decreased from 3.9/100,000 in 2013 to 1.5/100,000 in 2017 (OR=0.83, P < 0.001) (Figure 1).
Fifty three percent (181/344) of the pediatric patients were females. The mean age of TB patients was 6.3 years (Range = 0.17-14years). With regard to classification, 55% (188/344) of the TB patients were clinically diagnosed with pulmonary TB; 34% (119/344) diagnosed with extra pulmonary TB, and 11% (37/344) bacteriologically confirmed with pulmonary TB.
Tuberculosis patients originated from 11 districts with Mbale District showing the highest TB case notification rate (73/100,000) and Kapchorwa District showing the lowest TB case notification rate (3.8/100,000) (Figure 2).
One hundred seventy nine (52%) of the TB patients completed TB treatment. In logistic regression, 67% (118/175) TB patients who resided ≤ 20km away from the hospital completed TB treatment compared to 36% (61/169) of TB patients who resided > 20km away from the Hospital (AOR=3.3, 95% CI=2.1-5.2).
Discussion
Our investigation demonstrated that completion of TB treatment among children aged 0-14 years at MRRH in Uganda was associated with staying closer to the hospital (i.e. < 20km). Staying closer to MRRH /TB treatment centre (<20km away from MRRH) may have made it easy for the pediatric TB patients to access medication and complete the 6 months course of TB treatment. This agrees with a qualitative study conducted at selected health facilities in Asmara, Eritrea that indicated that access to health facility for TB treatment enabled them complete TB treatment because distance from their homes to the health facility was manageable (3). Other studies among TB patients in a TB treatment health facility in Ethiopia also indicated that completion of TB treatment was compromised if the distance from the patients home to the health facility was far (4,5).
We also found that the completion rate of childhood TB treatment was 52%. This TB treatment completion rate was lower than the targeted completion rate of 85% by WHO (6). This demonstrates that a good number of patients are unable to complete treatment which leads to increased transmission and possibly of multi drug resistant TB among the population.
There was a decline in the TB case notification rates at MRRH, from 2013 – 2017. The decline may be due to a scale up of Anti-Retroviral Therapy (ART) at MRRH. Since HIV is a major risk factor for developing TB, the scale up of ART could have reduced the TB case notifications. ART reduces the risk of TB infection in people living with HIV thereby reducing the TB transmissions and hence TB case notifications. This is consistent with other findings in Zimbabwe that pointed out that the declining TB case notifications was due to the scale up of ART(7).
However, our investigation had some limitations. The names of the health facilities to which the TB patients from MRRH transferred to were not indicated and therefore we could not tell if they eventually completed TB treatment or not. Failure to account for the TB treatment completion of the patients who transferred out from MRRH may have led to underestimation of the TB treatment completion rates among children.
Conclusions and recommendations
The TB treatment completion rate was below the WHO recommendation of 85%. Better TB completion rate was associated with TB patients residing ≤ 20km from the Hospital. To improve completion of TB treatment, MRRH should consider designing a means of follow up of TB patients who transfer out due to long distance to ensure they complete TB treatment in the scheduled period. Ministry of Health may open up more treatment facilities at lower levels closer to communities. Ministry of Health should consider educating communities on the importance of completing TB treatment.
References
1. Hamzaoui A, Yaalaoui S, Cherif FT, Saidi LS, Berraies A. Childhood tuberculosis: a concern of the modern world. European Respiratory Review. 2014 Sep 1;23(133):278–91.
2. National Tuberculosis and Leprosy Control Programme Revised National Strategic Plan 2015/16 – 2019/20 | Ministry of Health [Internet]. [cited 2018 Nov 25]. Available from: http://health.go.ug/content/national-tuberculosis-and-leprosy-control-programme-revised-national-strategic-plan-201516
3. Gebreweld FH, Kifle MM, Gebremicheal FE, Simel LL, Gezae MM, Ghebreyesus SS, et al. Factors influencing adherence to tuberculosis treatment in Asmara, Eritrea: a qualitative study. J Health Popul Nutr [Internet]. 2018 Jan 5 [cited 2019 Sep 21];37. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5756387/
4. Demissie M, Lindtjorn B, Berhane Y. Patient and health service delay in the diagnosis of pulmonary tuberculosis in Ethiopia. BMC Public Health. 2002 Sep 25;2:23.
5. Tadesse T, Demissie M, Berhane Y, Kebede Y, Abebe M. Long distance travelling and financial burdens discourage tuberculosis DOTs treatment initiation and compliance in Ethiopia: a qualitative study. BMC Public Health. 2013 May 1;13:424.
6. End_TB_Strategy.pdf [Internet]. [cited 2018 Nov 26]. Avail-able from: https://www.who.int/tb/strategy/End_TB_Strategy.pdf
7. Takarinda KC, Harries AD, Sandy C, Mutasa Apollo T, Zishiri C. Declining tuberculosis case notification rates with the scale-up of antiretroviral therapy in Zimbabwe. Public Health Action. 2016 Sep;6(3):164–8.


Comments are closed.