Trends and spatial distribution of human anthrax outbreaks, Uganda, 2017–2024
Authors: Loryndah Olive Namakula1*, Richard Migisha1, Joshua Kayiwa2, Simon Kyazze2, Issa Makumbi2, Lilian Bulage1, Benon Kwesiga1, Patricia Eyu1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2National Public Health Emergency Operations Center, Ministry of Health, Kampala, Uganda Correspondence*: Email: olivenamakula@uniph.go.ug, Tel: 256777650580
Summary
Background: The incidence of anthrax, a zoonosis of outbreak potential caused by category A bioterrorism agent bacillus anthracic has declined in some regions. However, outbreaks continue to occur in Uganda among other countries. A single confirmed case of human anthrax constitutes an outbreak. We described the trends and geographical distribution of anthrax outbreaks, Uganda, 2017–2024, to inform prevention and control strategies.
Methods: We reviewed data on outbreaks in Uganda from the electronic Public Health Emergency Management (ePHEM) database, 2017–2024. Data were presented as frequencies and proportions of outbreaks, case counts, fatalities, and case fatality rates (CFR). We used the Mann-Kendall test to test the significance of the trends.
Results: Uganda experienced 39 human anthrax outbreaks, 2017–2024, ranging from 2–14 annually, with most (14, 36%) occurring in 2024. A significant increase in the frequency of outbreaks was observed from 2020 to 2024 (p=0.043). The outbreaks resulted in 1,165 cases and 35 deaths, with an overall case fatality rate (CFR) of 3%. Anthrax spread across all regions, with the eastern and western regions most affected (14/39 outbreaks each). Twenty of the country’s 146 districts, primarily in the cattle corridor, experienced outbreaks, with recurrent cases in Kween, Ibanda, and Madi-Okollo.
Conclusion: The increase in outbreaks, coupled with the geographical spread across various districts demonstrates anthrax as a growing public health challenge. Strengthening anthrax preparedness and control programs, particularly in recurrent outbreak areas, and targeting high-risk districts with tailored interventions, could reduce future outbreaks and improve public health outcomes.
Background
Anthrax, caused by a gram-positive aerobic spore-forming bacterium, Bacillus anthracis is a zoonotic disease.(1) The spores can stay and survive in harsh environments and soil for many years, and animals typically get infected by eating the spores while grazing.(2) Among the human population, anthrax is spread through contact with an infected animal or its products and has an incubation period of 1-6 days. Depending on the transmission routes and clinical features, human anthrax infections are categorized into; cutaneous, gastrointestinal, inhalational, and injection-use anthrax, a relatively new form of anthrax among injection drug users.(2) Approximately 95% of all naturally occurring anthrax cases are of cutaneous anthrax, which is also the least fetal with a case fatality rate (CFR) of <1% if treated, and 20% if untreated.(3) According to the World Health Organization (WHO), anthrax does not typically spread from animal to animal, or human to human(4)
It is an outbreak-prone public health emergency, and a single confirmed case of human anthrax constitutes an outbreak(7) Bacillus anthracis produces extremely potent toxins, and is can be used for bioterrorism as a category A bioterrorism agent, making anthrax a potential global health security threat(8) According to WHO, the basis of anthrax control is in breaking the cycle of infections, and elimination of known potential infectious sources without delay(4) Anthrax among humans continues to be uncommon in some parts of the world, with some countries only reporting a few sporadic cases(5) On the contrary, anthrax outbreaks continue to occur in Uganda, among other countries(9, 10). We described the trends and spatial distribution of anthrax outbreaks, Uganda, January 2017-October 2024 to guide programming.
Methods
Study setting
Uganda is a country in East Africa with an estimated population of 45.9 million people with 10.8 million households,(11) and the majority (80%) of the households cultivate land or rear livestock for livelihood(12) It has a cattle corridor, which is an agroecological stretch from southwestern to north-eastern Uganda that is predominantly a livestock farming zone. The country is divided into four regions; Eastern, Western, Northern, and Central regions, which are further divided into subregions, that are further divided into smaller administrative units, districts, and the country currently has 146 districts.
Study design and data source
We conducted a descriptive study using the outbreak surveillance data from the Public Health Emergency Management (ePHEM) database hosted at the Ministry of Health (MoH), 2017-2024. Systematic recording of data on anthrax outbreaks started, through ePHEM.
Study variables, data abstraction, management, and analysis
We abstracted data on anthrax outbreaks including date of onset, number of cases (suspected, confirmed), fatalities, affected districts, laboratory results, press releases, situation reports, and outbreak investigation reports. Using Microsoft Excel, we conducted descriptive analyses and presented data as frequencies and proportions of the human anthrax outbreaks, cases, fatalities, case fatality rates, and affected districts and regions. Trends were presented using line graphs, and the Man-Kendall test was used to assess the significance of the trend. Quantum Geographic Information System was used to generate maps to demonstrate the spatial distribution of the anthrax outbreaks.
Ethical approval and consent to participate
Our study utilized outbreak investigation data from ePHEM at the MOH, with no personal identifiers. The Uganda Public Health Fellowship Program is part of the National Rapid Response Team, and has been granted permission to access and analyse outbreak data in ePHEM, and other data such as survey and surveillance data to inform decision making in the control and prevention of outbreaks and public health programming. Additionally, the MOH has also granted the program permission to disseminate the information through scientific publications. We stored the abstracted dataset in a password-protected computer and only shared it with the investigation team. In-addition, this activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.§ §See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
Results
Human anthrax outbreaks, Uganda, 2017-2024
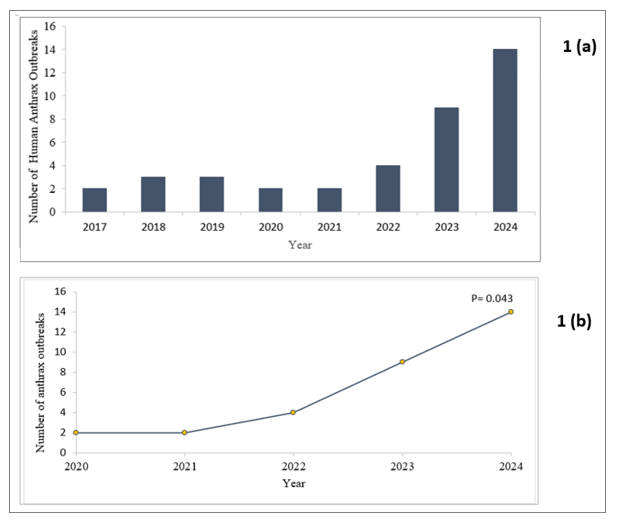
During the study period, Uganda experienced 39 human anthrax outbreaks, ranging from 2 to 14 annually, with the majority (36%) occurring in 2024 (Figure 1(a)). These outbreaks resulted in 1,165 cases, including 149 confirmed cases (12.8%), and 35 fatalities, yielding an overall case fatality rate (CFR) of 3% (35/1,165). Most (61.5%) of the outbreaks did not register fatalities. There was a significant increase in outbreaks from 2020 to 2024 (p=0.043) (Figure 1(b))
Spatial distribution of anthrax outbreaks, Uganda, January 2017–December 2024
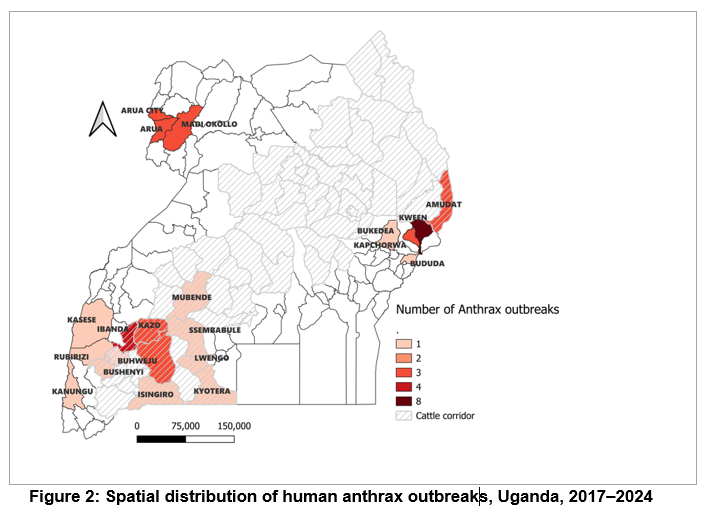
Overall, 20 (14%) of Uganda’s 146 districts experienced anthrax outbreaks, with 12 (60%) located in the cattle corridor (Figure 2). Kween District was the most affected, with 8 outbreaks over the 8 study period, followed by Ibanda with 4 outbreaks, then Madi-Okollo, Arua, Kazo and Kiruhura with 3 outbreaks each. Kween, Ibanda, and Madi-Okollo districts had recurrent outbreaks over the last three consecutive years (2022–2024), with Arua also having recurrent outbreaks from 2017–2019.
Discussion
We described the trends and spatial distribution of human anthrax outbreaks in Uganda, 2017–2024. There was an increase in human anthrax outbreaks, with most occurring in 2024. The majority of the outbreaks did not register fatalities, and the total CRF was 3%. Human anthrax outbreaks involved newer districts over the years, some of which reported higher CFRs. Kween District was the most affected with 8 outbreaks over the 8-year study period, and Kween, Ibanda and Madi-Okollo Districts had recurrent human anthrax outbreaks.
The significant increase of anthrax outbreaks in Uganda underscores an urgent need to strengthen and scale up anthrax preparedness and control to avert health, social, and economic loss(13). This increase could be attributed to changes in environmental conditions, such as droughts or floods, which could have influenced the distribution of anthrax(14, 15) Additionally, socio-economic factors, such as increased livestock movements, health system factors such as limited access to veterinary services, and inadequate public health infrastructure, may have contributed to the spread of the disease.
Anthrax outbreaks involving newer districts in different regions of the country over the years is concerning, highlighting a growing public health challenge, and implications for planning strategies. This highlights the need for comprehensive strategies to enhance preparedness, detection, and prompt response to anthrax outbreaks from all levels.
The finding that some districts including Kween, Ibanda, and Madi-Okollo experienced recurrent anthrax outbreaks could suggest that certain areas may be facing persistent risk factors such as; inadequate livestock vaccination programs, poor veterinary surveillance, or environmental and social behavioral factors that facilitate the survival and transmission of Bacillus anthracis spores.(17, 18) (19-21) (22, 23). The recurrence of anthrax outbreaks in these districts makes them anthrax outbreak hotspots, highlighting the need for further studies to understand the cause of the recurrence for more targeted interventions.
Study limitations
This study relied on secondary data from ePHEM, which does not capture the details of the case persons. We were not able to make a person description of the cases in terms of most affected persons, age group, sex, and other specific factors.
Conclusion
The increase in outbreaks, coupled with the geographical spread across various districts, reflects the evolving nature of anthrax transmission dynamics in the country, demonstrating anthrax as a growing public health challenge. Strengthening anthrax preparedness and control programs, particularly in recurrent outbreak areas, and targeting high-risk districts with tailored interventions, could reduce future outbreaks and improve public health outcomes.
Conflict of interest
The authors declare that they have no conflict of interest.
Author contribution
LON conceptualized the study idea, organized data from ePHEM, analyzed it, and wrote the bulletin. JK, SK, IM, LB, RM, BK PE, DK, and ARA supported in editing, and reviewing of the bulletin. All authors read and approved the final bulletin
Acknowledgments
The authors extend their gratitude to the staff of Uganda Public Health Fellowship Program for their technical support. The authors also acknowledge the teams at the Ministry of Health under the National Public Health Emergency Operations Center for support in accessing the data.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source is however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- CDC. About Anthrax 2024 [Available from: https://www.cdc.gov/anthrax/about/index.html#:~:text=Anthrax%20is%20a%20serious%20disease%20usually%20caused%20by,contact%20with%20infected%20animals%20or%20contaminated%20animal%20products.
- CDC U. About Anthrax 2024 [Available from: https://www.cdc.gov/anthrax/about/index.html.
- Health JHBSoP. Factsheet. Bacillus anthracis (Anthrax) 2023 [cited 2024 18th Dec]. Available from: https://centerforhealthsecurity.org/sites/default/files/2023-11/anthrax.pdf.
- WHO. Anthrax 2016 [Available from: https://www.who.int/europe/news-room/questions-and-answers/item/anthrax.
- Control EUCfDPa. Anthrax Annual Epidemiological Report for 2021 2021 [cited 2024 17th Feb]. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/anthrax-annual-epidemiological-report-for-2021.pdf.
- Ashique S, Biswas A, Mohanto S, Srivastava S, Hussain MS, Ahmed MG, et al. Anthrax: A narrative review. New Microbes and New Infections. 2024;62:101501.
- MOH. National Technical Guidelines for Integrated Disease Surveillance and Response 2012 [Available from: https://www.health.go.ug/cause/national-technical-guidelines-for-integrated-disease-surveillance-and-response/.
- CDC. Bioterrorism and Anthrax: The Threat 2024 [Available from: https://www.cdc.gov/anthrax/bioterrorism/index.html.
- Times NY. Mystery Amid an Anthrax Outbreak in Africa 2023 [Available from: https://www.nytimes.com/2023/12/19/health/anthrax-africa.html
- Africa VO. WHO Says Anthrax Strikes Five Countries in East and Southern Africa 2023 [Available from: https://www.voaafrica.com/a/who-says-anthrax-strikes-five-countries-in-east-and-southern-africa-/7394637.html.
- UBOS. National Population and Housing Census 2024 2024 [Available from: https://www.ubos.org/wp-content/uploads/2024/07/Censu-2024-PRELIMINARY-report.pdf.
- UBOS. Annual Agricultural Survey (AAS) 2019 – Statistical Release 2019 [Available from: https://www.ubos.org/wp-content/uploads/publications/05_2022Uganda_UBOS_StatRelease_AAS2019-Final.pdf
- Kabami Z, Agaba B, Naiga HN, Simbwa BN, Zavuga R, Kizito SN, et al. Emergence of anthrax in Bududa District, Eastern Uganda, February-May 2022: implications for prevention and control. PAMJ-One Health. 2024;14(15).
- Hugh-Jones M, Blackburn J. The ecology of Bacillus anthracis. Molecular aspects of medicine. 2009;30(6):356-67.
- Otieno FT. Environmental and socio-economic predictors of anthrax spatial distribution in Kenya 2023.
- Ratnayake R, Tammaro M, Tiffany A, Kongelf A, Polonsky JA, McClelland A. People-centred surveillance: a narrative review of community-based surveillance among crisis-affected populations. The Lancet Planetary Health. 2020;4(10):e483-e95.
- Bales ME, Dannenberg AL, Brachman PS, Kaufmann AF, Klatsky PC, Ashford DA. Epidemiologic responses to anthrax outbreaks: a review of field investigations, 1950–2001. Emerging Infectious Diseases. 2002;8(10):1163.
- Islam MS, Hossain MJ, Mikolon A, Parveen S, Khan MSU, Haider N, et al. Risk practices for animal and human anthrax in Bangladesh: an exploratory study. Infection ecology & epidemiology. 2013;3(1):21356.
- Kisaakye E, Ario AR, Bainomugisha K, Cossaboom CM, Lowe D, Bulage L, et al. Outbreak of anthrax associated with handling and eating meat from a cow, Uganda, 2018. Emerging Infectious Diseases. 2020;26(12):2799.
- Ntono V, Eurien D, Bulage L, Kadobera D, Harris J, Ario AR. Cutaneous anthrax outbreak associated with handling dead animals, Rhino Camp sub-county: Arua District, Uganda, January–May 2018. One Health Outlook. 2021;3(1):8.
- Chakraborty A, Khan SU, Hasnat MA, Parveen S, Islam MS, Mikolon A, et al. Anthrax outbreaks in Bangladesh, 2009–2010. The American journal of tropical medicine and hygiene. 2012;86(4):703.
- Nakanwagi M, Ario AR, Kwagonza L, Aceng FL, Mwesigye J, Bulage L, et al. Outbreak of gastrointestinal anthrax following eating beef of suspicious origin: Isingiro District, Uganda, 2017. PLoS Neglected Tropical Diseases. 2020;14(2):e0008026.
- Migisha R, Mbatidde I, Agaba DC, Turyakira E, Tumwine G, Byaruhanga A, et al. Risk factors for human anthrax outbreak in Kiruhura District, Southwestern Uganda: a population-based case control study. 2021.


Comments are closed.