Trends and distribution of malaria mortality among children and adolescents aged 0-17 years, Uganda, 2023: descriptive analysis of Medically Certified Cause of Death data
Authors: Jimmy Patrick Alunyo*1,2,3, Sarah Rachael Akello1,2,3, Daniel Wenani4, Olivia Nabulya3,4, Michael Turyasigura3, Paul Edward Okello5, Job Morokuleng5, Caroline Kyozira5, Caroline Nanziri5, Alex Riolexus Ario5, Godfrey Bwire3, Allan Muruta3 Institutional affiliations:1Mbale Clinical Research Institute, Mbale, Uganda, 2Department of Public Health, Busitema University Faculty of Health Sciences, 3Ministry of Health, Kampala, Uganda, 4Department of Epidemiology and Biostatistics, Makerere School of Public Health, Kampala, Uganda, 5Uganda National Institute of Public Health, Kampala, Uganda *Correspondence: Email: alunyo.j.patrick@gmail.com
Summary
Background: Malaria remains a leading cause of mortality in sub-Saharan Africa, accounting for 95% of global malaria deaths, with children under five being the most affected. Uganda ranks among the top five contributors to malaria cases and deaths, despite ongoing control efforts such as insecticide-treated nets (ITNs) and artemisinin-based combination therapies (ACTs). We analyzed trends and distribution of malaria deaths among children aged 0–17 years, Uganda, 2023, using Medically Certified Cause of Death (MCCD) data, to inform targeted interventions and improve malaria mortality surveillance.
Methods: We conducted a secondary analysis of MCCD data in the District Health Information Software version 2 (DHIS2) from January 1-December 31, 2023. We analyzed MCCD data with malaria deaths disaggregated by age group, sex, region, and health facility type. Spatial distribution by region was depicted by the use of Quantum Geographic Information Software.
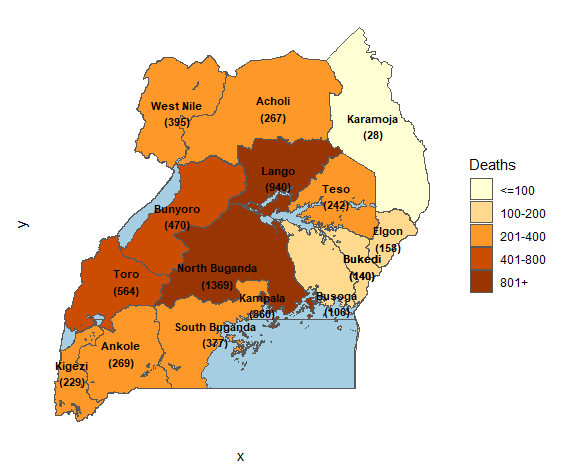
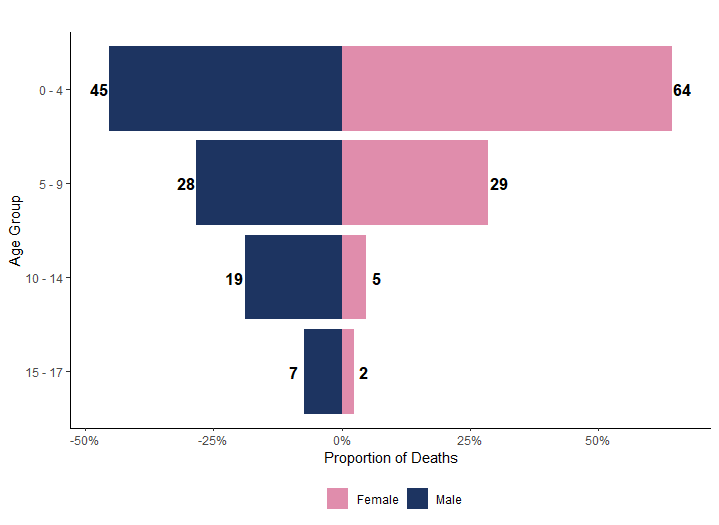
Results: A total of 5,002 deaths were recorded among children and adolescents aged 0-17 years. The highest mortality rates were observed in the North Buganda (1369) and Lango (940) regions accounting for 40.7% of the total deaths. The majority of malaria deaths occurred in children aged 14-17 years (36.5%) and 0-4 years (36.1%), accounting for 64% of female deaths and 45% of male deaths.
Conclusion: We highlight disparities in malaria mortality among children and adolescents in Uganda, with marked variations by sex, age, and region.
Background
Malaria remains one of the leading causes of morbidity and mortality worldwide, particularly in low- and middle-income countries. In 2022, an estimated 619,000 malaria deaths occurred globally, with sub-Saharan Africa accounting for 95% of these deaths. [1]. Children under five years are disproportionately affected, contributing to 80% of malaria deaths in the region [1]. The persistent burden of malaria in sub-Saharan Africa is driven by high Plasmodium falciparum transmission, vector resistance to insecticides, and gaps in healthcare access. In East Africa, Uganda ranks among the top five contributors to global malaria cases and deaths, with high transmission rates occurring year-round[1].
Despite significant investments in malaria prevention and control, including insecticide-treated nets (ITNs) and artemisinin-based combination therapies (ACTs), Uganda continues to experience a high malaria burden, with 478 cases per 1,000 people annually[1][2]. Malaria accounts for 30–50% of outpatient visits, 15–20% of hospital admissions, and 37,195 deaths in 2023 [3]. The highest malaria prevalence is observed in northern and eastern Uganda, where healthcare infrastructure is often inadequate. Children remain the most affected due to delayed diagnosis, limited access to treatment, and severe complications[4–6]. Additionally, geographic disparities in malaria mortality persist, with higher deaths in regions with poor healthcare access and low intervention coverage[7].
Understanding the burden and distribution of malaria deaths is crucial for guiding targeted interventions and policy decisions. By identifying high-risk age groups and regions, interventions to address the lack of age- and region-specific malaria mortality data, would be crucial for enhancing the effectiveness of Uganda’s malaria control and prevention programs. Additionally, it will contribute to improving death reporting systems, and demonstrate confidence in using the available data on the National Mortality Surveillance dashboard [8]. We analyzed trends and distribution of malaria deaths among children aged 0-17 years, Uganda, 2023 using Medically Certified Cause of Death (MCCD) data.
Methods
Study setting, design, and data source
Uganda is located in the East African region and the civil registration and vital statistics (CRVS) system is still evolving. While progress has been made in birth registration, especially for children under five, death registration remains underdeveloped. As of 2023, fewer than half (49%) of reported deaths were officially notified, and only 34.1% were medically certified [9].
We conducted a retrospective descriptive study using data from MCCD dataset available in District Health Information Software version 2 (DHIS2). The MCCD dataset compiles data on deaths recorded in Uganda with a focus on those medically certified deaths. It includes vital mortality data, where the cause of death has been formally determined by a medical professional. Data is collected from various health facilities across Uganda, including hospitals and health centers, where death notifications and medical certifications are processed. The dataset includes detailed information on the demographic characteristics of the deceased, such as age, sex, residence, and medical cause of death, with specific codes assigned based on the International Classification of Diseases (ICD). The MCCD form is completed by physicians based on clinical assessment, diagnostic findings, and available medical records, ensuring standardized cause-of-death reporting. Data is collected at health facilities and community level during patient death certification and subsequently compiled into national mortality databases by filling out form 100, which in turn feeds that data into DHIS2.
Study variables, data abstraction, and data analysis
The dependent variable was malaria deaths. Independent variables included age (0-17 years), gender (male and female), geographic region (high vs. low malaria transmission areas), health facility level (district hospitals, health centers, or private clinics), and cause of death certification (the proportion of medically certified deaths). These variables were analyzed to identify patterns and disparities in malaria mortality.
Data for all these variables was abstracted from the MCCD data base and exported in Microsoft ExcelTM and analysis in R software. Descriptive statistics were calculated to including deaths by age, gender, and geographic location. Proportions of malaria deaths per age group, gender and region were calculated, and geographic and temporal variations in malaria deaths were depicted using Quantum Geographic Information System (QGIS) to identify high-burden regions and trends over time.
Ethical consideration
This study utilized secondary data from the Medically Certified Cause of Death (MCCD) dataset, which does not involve direct interaction with human participants. As such, formal ethical review and approval were not sought. However, administrative permission to access the data was obtained from the Director General of Health Services and the Division of Health Information, Ministry of Health, Uganda. These permissions ensured compliance with national regulations regarding the use of public health data. The study adhered to ethical principles related to confidentiality and data security, ensuring that all data were anonymised and securely stored to protect individual privacy.
Results
Geographic distribution of malaria deaths among children aged 0-17 years, Uganda, 2023
A total of 5,700 malaria deaths were reported across all age groups. Of these deaths, 5,002 were of children and adolescents aged 0 -17 years, with regional disparities (Table 1).
The highest malaria mortality was reported in regions of North Buganda (1,369 deaths) and Lango (940 deaths), accounting for 40.7% of the total deaths. The sub-regions of Toro (564 deaths), Bunyoro (470 deaths), and South Buganda (337 deaths) reported moderate mortality rates, collectively contributing to 24.3% of the total deaths (Figure 1). The regions of Karamoja (28 deaths), Busoga (106 deaths), and Elgon (158 deaths) reported the lowest mortality rates, representing 5.3% of the total deaths
Age-specific mortality among children aged 0-17 years, Uganda, 2023
Of the 5,002 medically certified deaths, 274 (100%) were malaria deaths and the majority were reported among children aged 14-17 years (36.5%) of age (Table 1).
Table 1: Distribution of malaria deaths by age group among children and adolescents,0–17 years, Uganda, 2023
| Age groups (years) | Malaria deaths | Total deaths | % malaria deaths per age group | |
| n | (%) | |||
| 0-4 | 99 | (36.1) | 1,287 | 7.7 |
| 5-9 | 52 | (19.0) | 153 | 34.0 |
| 10-14 | 23 | (8.4) | 106 | 21.7 |
| 15-17 | 100 | (36.5) | 3,456 | 2.9 |
| Total | 274 | (100) | 5,002 | 66.3 |
Gender distribution of malaria deaths among children aged 0-17 Years, Uganda, 2023
More malaria deaths occurred among females (64%) than males (45%). In the 5–9 age group, mortality was similar between males (29%) and females (28%). The disparity widened in the 10–14 age group, where male deaths (19%) outnumbered female deaths (5%). In the 15–17 age group, male deaths (7%) were more than triple those of females (2%). Overall, while younger females had higher mortality, older males exhibited the highest death rates, particularly in the 10–14 and 15–17 age groups (Figure 2).
Distribution of malaria deaths among children and adolescents, 0-17 years by health facilities, Uganda, 2023
Lira Regional Referral Hospital (RRH) reported the highest number of malaria deaths, with 58 deaths (31.52%) (Table 2). This was followed by Kagadi General Hospital (GH) with 21 deaths (11.41%), and both Hoima and Kayunga RRHs, each reporting 16 deaths (8.70%). The remaining facilities reported fewer deaths, with most facilities recording under 5 deaths (2.72%), including Buvuma HCIV, Dr. Ambrosoli Memorial Hospital Kalongo, Kangulumira HCIV, Luwero GH, Mubende RRH, and St. Mary’s Hospital Lacor, each reporting 1 death (0.54%) (Table 2).
Table 2: Distribution of malaria deaths among children and adolescents, 0-17 years by health facility, Uganda, 2023
| Health facility | Malaria deaths (n) | (%) |
| Lira Regional Referral Hospital (RRH) | 58 | (31.52) |
| Kagadi General Hospital (GH) | 21 | (11.41) |
| Hoima RRH | 16 | (8.70) |
| Kayunga RRH | 16 | (8.70) |
| Kiryandongo GH | 14 | (7.61) |
| Mbale RRH | 8 | (4.35) |
| Arua RRH | 6 | (3.26) |
| Virika Hospital | 6 | (3.26) |
| Kagando Hospital | 5 | (2.72) |
| Kiboga GH | 5 | (2.72) |
| Kyegegwa GH | 5 | (2.72) |
| Soroti RRH | 4 | (2.17) |
| Entebbe RRH | 3 | (1.63) |
| Ibanda Hospital | 3 | (1.63) |
| China Uganda Friendship (Naguru) RRH | 2 | (1.09) |
| Gulu RRH | 2 | (1.09) |
| Itojo GH | 2 | (1.09) |
| Nakaseke GH | 2 | (1.09) |
| Buvuma Health Centre (HC) IV | 1 | (0.54) |
| Dr. Ambrosoli Memorial Hospital Kalongo | 1 | (0.54) |
| Kangulumira HC IV | 1 | (0.54) |
| Luwero GH | 1 | (0.54) |
| Mubende RRH | 1 | (0.54) |
| St. Mary’s Hospital Lacor | 1 | (0.54) |
| Total | 184 | (100) |
Monthly trends in malaria deaths among children and adolescents, 0-17 years, Uganda, 2023
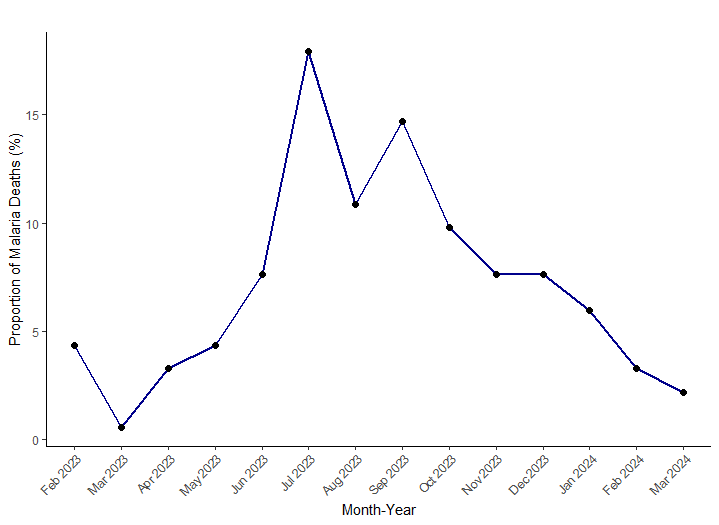
Malaria deaths exhibit a seasonal pattern, with a notable decline from January through March (Figure 3). Mortality begins to rise in April, reaching a peak in July. This was followed by a sharp decline in August. there is a secondary increase observed in September before the trend resumes a steady decline from October through January.
Annual gender-disaggregated trends in malaria mortality among children (0–17 Years) in Uganda, 2023
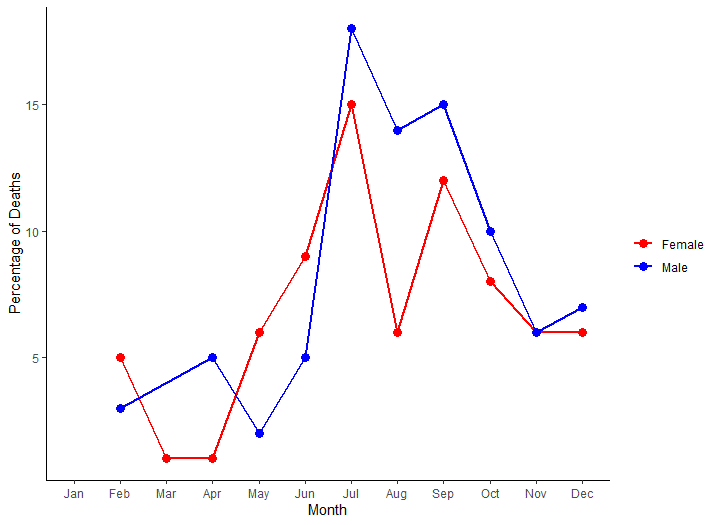
Malaria deaths exhibit a seasonal pattern, with unequal mortality distribution across the 12 months for both sexes. However, the highest mortality for females was in July and September. For males, the highest mortality came in the months of July and September. Throughout the year, male mortality consistently surpasses female mortality (Figure 4)
Discussion
In this nationwide analysis of medically certified malaria mortality among children and adolescents aged 0-17 years in Uganda, we found substantial sex, age, temporal, and regional specific disparities. Overall, malaria mortality was markedly higher in males than females, with notable seasonal peaks in July and September. Geographically, Lango sub-region and North Buganda region exhibited disproportionately high malaria mortality. Children aged 0–4 years bore the highest mortality burden across both sexes, whereas younger females had higher mortality than males, a trend that reversed in the older age groups.
In this study, we found that there was a significant geographic variation in malaria mortality across Uganda. The highest mortality rates were observed in regions such as North Buganda (1,369 deaths) and Lango (940 deaths), which together accounted for nearly 41% of all malaria deaths. In contrast, regions like Karamoja, Busoga, and Elgon reported the lowest mortality rates, contributing only 5.3% of the total deaths. The geographical disparities found in this study could be attributed to several factors, including variations in malaria transmission intensity, local healthcare infrastructure, access to prevention and treatment services, and issues of underreporting [10]. Whereas regions like North Buganda and Lango, which are in high malaria transmission areas, are more likely to experience a higher burden of malaria deaths, effective surveillance and targeted interventions are crucial to reducing mortality in these areas Conversely, the lower mortality rates in regions like Karamoja and Elgon could reflect either underreporting or lower transmission rates in these areas. Our findings are in line with previous studies in sub-Saharan Africa, including Uganda, which have consistently shown that malaria mortality is disproportionately concentrated in high-transmission areas. For instance, Wanzira et. al., (2016) observed similar regional disparities in Uganda, with northern and eastern regions bearing a higher burden of malaria mortality [11]. Our findings underline the need for targeted malaria interventions that focus on high-burden regions. Policies should prioritize increased access to malaria prevention and treatment services in the most affected regions, including more robust surveillance and mortality tracking systems.
Additionally, in the analysis of age-specific mortality, we found that children aged 0-4 years and adolescents aged 5-9 years were particularly vulnerable to malaria deaths. We reckon that the higher proportion of malaria deaths we saw in the younger age group could be attributed to problems of delayed diagnosis and limited prevention measures taken by caregivers of these children.
Furthermore, we also found high malaria mortality among male children. This we we think could be backed by evidence of male children having a higher susceptibility to malaria due to genetic and immunological differences. Additionally, it could be explained by exhibited behavioural patterns of male children, such as increased outdoor activities among boys, which can elevate their exposure to malaria vectors, thereby increasing infection and mortality rates. However, our finding is in line with what Mseza and others found in Western Uganda, which found male gender was independently associated with higher odds of cerebral malaria [12].
In our analysis, malaria mortality among children and adolescents in Uganda peaked notably during July and September. This temporal pattern aligns with seasonal variations in malaria transmission, which are closely associated with the country’s climatic conditions. Uganda experiences two primary rainy seasons: March-May and August–October. These periods of increased rainfall create favourable breeding environments for Anopheles mosquitoes, the vectors responsible for malaria transmission. Consequently, a rise in malaria cases typically follows these rainy seasons. Our observed mortality peaks in July and September correspond to these transmission patterns, with the July peak following the first rainy season and the September peak aligning with the onset of the second. This seasonal trend found in our study is consistent with previous studies in Uganda. For instance, a study conducted in Gulu District by Ouma and others reported biannual peaks in malaria infections during June–July and September–October, periods that closely match our mortality findings[13]. Similarly, another study by Kamya and colleagues also highlighted two annual peaks in malaria transmission following the rainy seasons, reinforcing the link between rainfall and increased malaria incidence[7].
Limitations and strengths
Despite using MCCD data, our study findings could have been limited by the underreporting of deaths that characterised mortality surveillance in Uganda, particularly in rural and hard-to-reach areas. However, we ensured that we downloaded the latest mortality surveillance dataset for the year 2023. Additionally, some malaria deaths may have been misclassified due to challenges in accurate diagnosis and cause-of-death certification. However, we anticipated this and used ICD 11 code cause of death for malaria. Nonetheless, our study used a descriptive analysis of malaria mortality in Uganda using the MCCD dataset in children and adolescents 0-17 years, hence providing a valuable resource for understanding mortality patterns in the context of incomplete death registration. The study also leverages existing mortality data, which allows for large-scale analysis without the logistical challenges of primary data collection.
Conclusion
There are significant geographic and age-specific disparities in malaria mortality, with high mortality in the Lango region and North Buganda region and among older children and adolescents. Designing and implementing malaria control strategies that address the specific needs of high-burden regions and vulnerable age groups, including adolescents is critical. Increase public awareness about the importance of death reporting and improve the training of healthcare workers on cause-of-death certification.
Conflict of interests
The authors declare that they have no competing interests.
Authors’ contributions
The primary author contributed to this study by conceptualising the Research design and drafting the initial manuscript. All the coauthors provided expertise in critically revising the manuscript for intellectual content. The last author supervised the overall review, provided guidance throughout the manuscript drafting, and critically reviewed and revised the manuscript for important intellectual content. All authors have read and approved the final version of the manuscript.
Acknowledgements
We thank the Department of Integrated Epidemiology, surveillance and Public Health Emergencies, Division of Health Information, CDC Foundations and IDEA fellowship program for their technical support during the conceptualisation and drafting of this study
Copyrights and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citations as to source, however, are appreciated. Any Article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
[1] WHO. World malaria report 2021 [Internet], https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021 (2021).
[2] WHO. Uganda MPs Move to End Malaria, https://www.afro.who.int/countries/uganda/news/uganda-mps-move-end-malaria?utm_source=chatgpt.com (2023).
[3] Minstry of Health. National Mortality Surveillance Dashboard, https://hmis.health.go.ug/dhis-web-dashboard/#/HzH08CdXEdU (2023).
[4] Marie A, Zalwango G, Bulage L, et al. Quarterly Epidemiological Bulletin: April – June, 2023. 2023; 8: 2017–2021.
[5] Olum J, Mukunya D, Nambozo B, et al. Severe malaria readmissions in Northern Uganda : a cross ‑ sectional study. Malar J. Epub ahead of print 2025. DOI: 10.1186/s12936-025-05307-8.
[6] M NA. Challenges of Malaria Control in Northern Uganda : Infrastructure , Access , and Healthcare Delivery.
[7] Kamya MR, Arinaitwe E, Wanzira H, et al. Malaria transmission, infection, and disease at three sites with varied transmission intensity in Uganda: Implications for malaria control. Am J Trop Med Hyg 2015; 92: 903–912.
[8] Ministry of Health. National Mortality Surveillance Dashboard, https://hmis.health.go.ug/dhis-web-dashboard/#/HzH08CdXEdU (2025).
[9] Zalwango M, Kyozira C, Nambuya M, et al. A Rapid Assessment of Mortality Surveillance in Uganda. 2024. Epub ahead of print 28 August 2024. DOI: 10.1101/2024.08.28.24312727.
[10] Yeka A, Gasasira A, Mpimbaza A, et al. Malaria in Uganda: Challenges to control on the long road to elimination. I. Epidemiology and current control efforts. Acta Trop 2012; 121: 184–195.
[11] Wanzira H, Katamba H, Okullo AE, et al. The challenge of using intermittent preventive therapy with sulfadoxine/pyrimethamine among pregnant women in Uganda. Malar J 2016; 15: 1–7.
[12] Mseza B, Kumbowi PK, Nduwimana M, et al. Prevalence and factors associated with cerebral malaria among children aged 6 to 59 months with severe malaria in Western Uganda: a hospital-based cross-sectional study. BMC Pediatr 2024; 24: 704.
[13] Simple O, Mindra A, Obai G, et al. Influence of Climatic Factors on Malaria Epidemic in Gulu District, Northern Uganda: A 10-Year Retrospective Study. Malar Res Treat; 2018. Epub ahead of print 2018. DOI: 10.1155/2018/5482136.


Comments are closed.