Trends and distribution of Leprosy cases, Uganda, 2020–2024, tracking progress towards elimination
Authors: Gertrude Abbo1, Richard Migisha1, Geofrey Amanya2, Rose Kengonzi2, Alex Mulindwa2, Stavia Turyahabwe2, Henry Luzze2, Benon Kwesiga1, Alex Riolexus Ario1 Affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda 2National Tuberculosis and Leprosy program, Ministry of Health, Kampala, Uganda Correspondence: Tel: +256773237156, Email: abbog@uniph.go.ug
Summary
Background: Leprosy is targeted for eradication worldwide. In 2021, the World Health Organization instigated a new Global Leprosy Strategy, termed “Towards Zero Leprosy”. However, Uganda still reports ≥1 case/1,000,000 population. We described the trends and distribution of leprosy cases, in Uganda, 2020 to 2023, and assessed progress toward elimination.
Methods: We conducted a descriptive analysis of leprosy surveillance data abstracted from the District Health Information System (DHIS2), Uganda, 2020-2023. Incidence rates of leprosy cases were calculated by age, sex, Grade 2 Disability (G2D), region, and district. To assess the significance of observed trends, we used the Mann-Kendall test.
Results: During 2020–2024, 1,899 leprosy cases were reported, with an overall incidence of 49 per 1,000,000 population. The most affected group was those >15 years (13 per 1,000,000); incidence was equal between genders (9 per 1,000,000). Of the cases, 86% were multi-bacillary, 14% pauci-bacillary, and 23% had G2D. Incidence peaked in 2022 (13 per 1,000,000) and was lowest in 2020 (6 per 1,000,000), showing a non-significant upward trend (p=0.2207). The West Nile Region had the highest incidence (56–280 per 1,000,000), with Obongi District in the West Nile Region reporting the highest G2D rate (99 per 1,000,000).
Conclusions: Uganda’s progress toward leprosy elimination is facing challenges, with ongoing cases and delayed diagnoses as indicated by the high G2D rates. The high incidence in the West Nile Region highlights the need for targeted interventions. Further studies are needed to explore the underlying factors contributing to the persistent incidence, especially in the most affected districts.
Background
Leprosy, a chronic infectious disease caused by Mycobacterium leprae, primarily affects the skin, peripheral nerves, upper respiratory tract, and eyes. Delayed diagnosis and older age worsen the progression of physical deformities associated with the disease(1). Leprosy has a lengthy and varied incubation period, typically averaging 5 years but potentially extending up to 20 years before symptoms appear(2). Leprosy primarily spreads through direct or indirect contact between infected individuals and healthy people (3). The World Health Organization (WHO) classifies patients for treatment purposes into two groups: paucibacillary (PB) with up to five skin lesions and multibacillary (MB) with six or more. This classification helps guide treatment and assess the risk of leprosy reactions and nerve damage(7).
Leprosy remains endemic in over 120 countries globally, with approximately 200,000 new cases reported annually(4). Global elimination of leprosy as a public health issue—defined as a prevalence of <1 per 10,000 population—was officially achieved in 2000, following World Health Assembly resolution 44.9, and in most countries by 2010(5).
Despite intensive community-based contact tracing and improved adherence support, leprosy remains endemic in Uganda, with 40% of districts reporting at least one case to the National Tuberculosis and Leprosy Program (NTLP) as of 2016(8). The incidence of grade 2 disability surged to 1.72 per million, over three times the NSP target(10). We described the trends and distribution of leprosy cases, Uganda, 2020–2024 to inform targeted control interventions.
Methods
Our study utilized data generated from the entire country. Leprosy diagnosis and treatment is free in Uganda. The hospitals receive suspected leprosy cases from health facilities called Health Centers II, III, and IV (MOH, 2015). Six health facilities, five general hospitals, and one HC III, currently have leprosy treatment centers. These include two facilities in Eastern Uganda, three in Northern Uganda, and one in Western Uganda. In 2021, the Ministry of Health launched the Community Awareness, Screening, Testing and Treatment to end TB and Leprosy in Uganda Campaign (CAST), an enhanced case-finding approach for the un-diagnosed TB and leprosy cases (including those missed during the COVID-19 pandemic period) towards combating community TB and leprosy transmission and end TB and leprosy in Uganda.
We conducted a descriptive analysis of leprosy surveillance data abstracted from the district health information system from 2020 to 2024. We abstracted data about leprosy cases by age, sex, type of leprosy, and disability grades. We calculated the incidence of leprosy by person, place, and time. We also abstracted data on the proportions of leprosy by type, that is, multibacillary and G2D to observe the trends in the country over time from 2020 to 2024.
We drew maps to demonstrate the spatial distribution of leprosy cases using Geographic Information Systems (GIS). To visualize trends, we plotted line graphs showing annual leprosy incidence against time. Data analysis was performed using R software, with trend significance evaluated using the Mann-Kendall test, while Sen’s slope test was employed to determine the direction of the trend.
This analysis used surveillance data from DHIS2. This data is aggregated with no individual patient identifiers. However, we sought and obtained permission from the MoH to use the data. The US Centers for Disease Control and Prevention (CDC) also provided the non-research determination for non-human subjects, which waives the need for a full Institutional Review Board. We collected de-identified data. All data was stored in password-protected computers and access was limited to the study team.
Results
Descriptive epidemiology of leprosy cases in Uganda, 2020-2024
Overall, the incidence of leprosy was 49/1,000,000 in the population over the five years. The incidence of leprosy increased from 6/1,000,000 population in 2020 to 13/1,000,000 population in 2022. The incidence later declined to 6/1,000,000 population in 2024. We identified a total of 1,899 leprosy cases from 2020 to 2024, of which 13% involved children < 15 years of age, 55% were females, 86% were multi-bacillary, and 23% presented with Grade 2 Disability (G2D) (Table 1).
Table 1: Person characteristics of Leprosy cases notified in Uganda, 2020-2024
| Variable | 2020 | 2021 | 2022 | 2023 | 2024 | Total |
| Annual cases n(%) | 234(12) | 467(26) | 581(30.5) | 342(18) | 275(13.5) | 1899(100) |
| Sex | ||||||
| Male n(%) | 123(14) | 218(25.5) | 254(30) | 144(17) | 113(13.5) | 852(45) |
| Female n(%) | 111(11) | 249(24) | 327(31) | 198(19) | 162(15.5) | 1047(55) |
| Type of leprosy | ||||||
| MB n(%) | 211(13) | 358(22) | 531(32) | 298(18) | 238(14.5) | 1636(86) |
| PB n(%) | 23(9) | 109(41) | 50(19) | 44(17) | 37(14) | 263(14) |
| G2D n(%) | 92(21) | 86(19.5) | 101(23) | 83(19) | 78(18) | 440(23) |
| Age in years | ||||||
| <15 years n(%) | 29(11) | 54(21) | 72(28) | 56(22) | 47(18) | 258(13) |
| ≥15 years n(%) | 210(13) | 413(25) | 509(31) | 286(17) | 228(14) | 1646(87) |
G2D: Grade 2 disability; PB: Pauci-bacillary; MB: Multi-bacillary
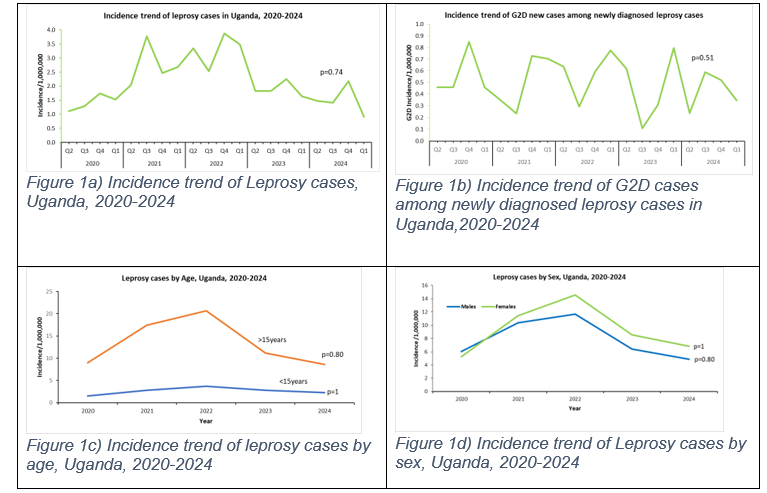
There was an insignificant increase in the incidence of leprosy cases from 2020, with cases peaking in 2022 (p=0.74). Leprosy incidence increased from 2/1,000,000 population in 2020 to 4/1,000,000 population in 2021 and 2022 (Figure 1a).
Similarly, there was a consistent rise and fall in the incidence of G2D cases reported throughout the five years, although this trend was not statistically significant(p=0.51). G2D cases peaked with 1/1,000,000 people reported every July to September (Q3) for the five years (Figure 1b).
There was an insignificant rise in the incidence of leprosy in both adults above 15 years and children below 15 years from 2020 to 2022 and later a drop in the incidence of leprosy from 2022 to 2025(p=0.80 and p=1, respectively). The age group > 15 years was the most affected with a mean incidence of 13 cases/1000,000 population. Leprosy incidence was highest in 2022 across both males and females as well as both age groups (Figure 1c).
Overall, the incidence of leprosy was higher among females compared to males. The incidence of leprosy among males was higher in 2020, with males at 6/1,000,000 population compared to 5/1,000,000 among females. The incidence was higher in both sexes in 2022 compared to other years. On average, there was no observed difference in incidence in both sexes at 8/1,000,000 population and 9/1,000,000 population for males and females, respectively(p=0.80&p=0.1) (Figure 1d).
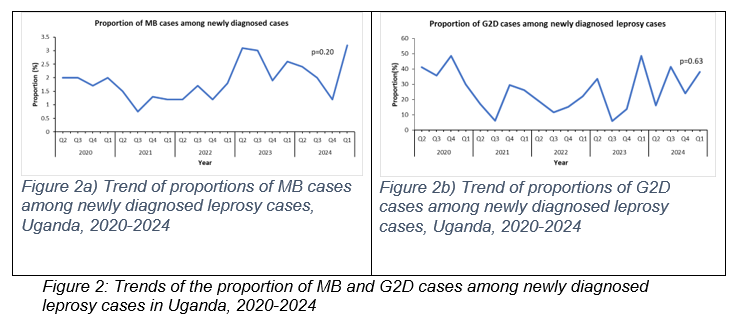
Trends of the proportion of MB and G2D cases among newly diagnosed leprosy cases in Uganda, 2020-2024
Overall, there was a non-significant increase in the proportion of MB and G2D cases among the newly diagnosed leprosy cases throughout the five years (Figure 2).
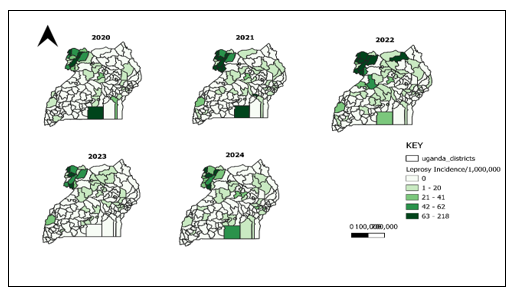
Spatial distribution of leprosy cases, Uganda, 2020-2024
Approximately 72/146 (49%) of the districts in Uganda reported ≥1 new case of leprosy in the five years. There was an increase in the number of districts reporting leprosy cases, rising from 33 out of 146 districts (23%) in 2020 to 41 out of 146 districts (28%) in 2021 and further to 44 out of 146 districts (30%) in 2022. There was a drop in the number of districts reporting cases in 2023 from 44/146(30%) in 2022 to 34/146(23%) in 2023 and an increase in 2024 with 39/146(27%). The overall mean annual incidence of leprosy cases in the five years in the districts was 10 cases/1000,000 population. The mean annual Incidence of leprosy increased from 7 cases/1000,000 population in 2020 to 13 cases/1000,000 population and 15 cases/1000,000 population in 2021 and 2022. The incidence later dropped to 7/1,000,000 population in 2023 and increased to 8/1,000,000 population in 2024 with fewer districts affected (Figure 4a). The districts of Terego, Obongi, Madi okollo, and Koboko were the most affected districts with an overall incidence of > 100 cases/1000,000 population across the five years. 8/9(80%) of the most affected districts were predominantly from the West Nile region located in the northwestern part of the country.
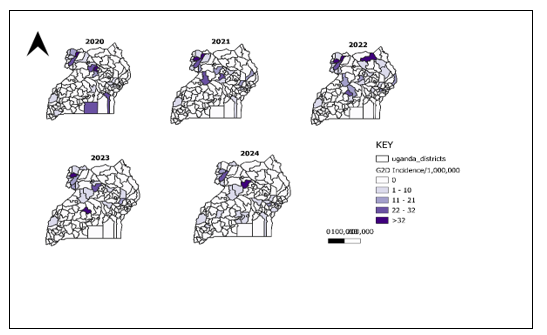
Spatial distribution of G2D cases in Uganda from 2020 to 2023
Overall, there was a steady rise in the incidence of G2D cases reported annually with an average incidence of 1 case/1000,000 population. The proportion of districts reporting at least one case of G2D increased between 2021 and 2022 from (20/146 (14% to 27/146 (19%. The year with the least number of districts reporting was 2023 (17/146), 12%. Overall, 2021 and 2022 recorded the highest mean annual incidence of G2D cases at 3 cases/1000,000 population, while 2020 and 2023 reported the lowest incidence of 2 cases/1000,000 population. The most affected districts each year were Kole District with an incidence of 70 cases/1000,000 population in 2020, Obongi District with an incidence of 99 cases/1000,000 population in 2021, Terego District with an incidence of 69 cases/1000,000 population in 2022, Kiboga District with an incidence of 65 cases/1000,000 population and Oyam district with an incidence of 56 cases/1,000,000 population in 2024. (Figure 4b).
Discussion
The overall incidence of leprosy had increased over time with equal rates across both genders. Most of the cases reported were multibacillary type leprosy with 23% of the multi-bacillary cases classified as G2D. The districts in the West Nile Region were the most affected in the country during 2020-2024.
Thirteen percent of the leprosy cases identified across the country were children. This is double the National Strategic Plan (NSP) target of 6%, which may imply evidence of active spread of the disease among the population, as cited in the WHO leprosy report of 2022(11)
Eighty-six percent of the cases notified were multibacillary cases, which may suggest the occurrence of active transmission of the disease and, consequently, greater potential to incapacitate the affected individuals. This may also signify late case detection, which may result in late diagnosis and, eventually, disability. In addition, people who are affected by multibacillary forms of the disease have a greater chance of developing health problems, Leprosy is highly disabling when not properly treated in the population, which can influence academic school performance (and future occupation) and cause problems related to social limitations, discrimination, self-esteem, and stigma experienced by the affected person(12).
There was a growing trend in the number of G2D cases from 2022 to 2023, which may indicate that the country faces difficulties in the early diagnosis of the disease and ongoing transmission. Our study was entirely descriptive, covering the whole population; however, the fact that there is an increasing trend of G2D cases is concerning, as it falls far short of the WHO goal of zero disability in children.(13)
In our study, the highest number of leprosy cases was reported in 2022, which coincided with the period following the launch of the Community Awareness, Screening, Testing, and Treatment (CAST) campaign in 2021 at ending TB and leprosy in Uganda. (14).
Study limitations
Among the limitations of the study, the use of secondary data, with the presence of untimely reporting and incomplete data can’t be overlooked. This could have underestimated the incidence of the disease across the country. We, however, catered for this gap by cross-referencing our findings with what the national TB and leprosy program had reported, making our findings reliable and valid.
Conclusion
Uganda is not yet on track for leprosy elimination, with ongoing cases and delayed diagnoses indicated by G2D. The high incidence in the West Nile Region highlights the need for targeted interventions. To accelerate progress toward elimination, further studies are needed to explore the underlying factors contributing to the persistent incidence, especially in the most affected districts. We recommend further studies to evaluate the surveillance system for Leprosy, especially in the most affected districts and regions. We also recommend further studies to understand the factors associated with the increase in leprosy cases particularly G2D and multibacillary cases reported among the most affected districts of the country.
Conflict of Interest
The authors declared no conflict of Interest
Author Contributions
GA, AG, RM, AM, BK, RK, ARA, ST wrote the protocol of the study. GA analyzed and interpreted the data. GA drafted the initial bulletin, GA, AG, RK, and RM contributed to the first draft and all authors read and approved the final bulletin. Permission to publish the article was obtained from all the bulletin authors.
Acknowledgements
We appreciate the technical support of the Uganda Public Health Fellowship Program and NTLP.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source is however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Yang J, Li X, Sun Y, Zhang L, Jin G, Li G, et al. Global epidemiology of leprosy from 2010 to 2020: A systematic review and meta-analysis of the proportion of sex, type, grade 2 deformity and age. Pathog Glob Health. 116(8):467–76.
- Ogunsumi DO, Lal V, Puchner KP, Brakel W van, Schwienhorst-Stich EM, Kasang C, et al. Measuring endemicity and burden of leprosy across countries and regions: A systematic review and Delphi survey. PLoS Negl Trop Dis. 2021 Sep 20;15(9):e0009769.
- Sarode G, Sarode S, Anand R, Patil S, Jafer M, Baeshen H, et al. Epidemiological aspects of leprosy. Dis Mon. 2020 Jul 1;66(7):100899.
- The International Journal of Mycobacteriology [Internet]. [cited 2024 Aug 29]. Available from: https://journals.lww.com/ijmy/fulltext/2017/06030/challenges_beyond_elimination_in_leprosy.2.aspx
- Leprosy [Internet]. [cited 2024 May 26]. Available from: https://www.who.int/news-room/fact-sheets/detail/leprosy
- Global leprosy (Hansen disease) update, 2021: moving towards interruption of transmission [Internet]. [cited 2024 May 23]. Available from: https://www.who.int/publications-detail-redirect/who-wer9736-429-450
- Classification of Leprosy | Infolep [Internet]. [cited 2024 May 23]. Available from: https://www.leprosy-information.org/resource/classification-leprosy-11
- Spatial distribution and temporal trends of leprosy in Uganda, 2012-2016: a retrospective analysis of public health surveillance data – PubMed [Internet]. [cited 2024 May 23]. Available from: https://pubmed.ncbi.nlm.nih.gov/31783799/
- National Tuberculosis and Leprosy Control Programme Revised National Strategic Plan 2015/16 – 2019/20 | MOH Knowledge Management Portal [Internet]. [cited 2024 May 26]. Available from: http://library.health.go.ug/communicable-disease/tuberculosis/national-tuberculosis-and-leprosy-control-programme-revised
- NATIONAL STRATEGIC PLAN FOR TUBERCULOSIS AND LEPROSY CONTROL 2020/21 – 2024/25 – Ministry of Health | Government of Uganda [Internet]. [cited 2024 May 23]. Available from: https://www.health.go.ug/cause/national-strategic-plan-for-tuberculosis-and-leprosy-control-2020-21-2024-25/
- Leprosy | WHO | Regional Office for Africa [Internet]. 2024 [cited 2024 Nov 6]. Available from: https://www.afro.who.int/health-topics/leprosy
- Júnior JFM, Ramos ACV, Alves JD, Crispim J de A, Alves LS, Berra TZ, et al. Inequality of gender, age and disabilities due to leprosy and trends in a hyperendemic metropolis: Evidence from an eleven-year time series study in Central-West Brazil. PLoS Negl Trop Dis. 2021 Nov 16;15(11):e0009941.
- Leprosy (Hansen’s disease): interrupting transmission and achieving zero autochthonous cases [Internet]. [cited 2024 Dec 5]. Available from: https://www.who.int/news/item/26-04-2021-leprosy-(hansen-s-disease)-interrupting-transmission-and-achieving-zero-autochthonous-cases
- New Vision [Internet]. [cited 2024 Jul 4]. Let us work together to end TB in Uganda – WHO. Available from: https://www.newvision.co.ug/articledetails/NV_156724
- Alrehaili J. Leprosy Classification, Clinical Features, Epidemiology, and Host Immunological Responses: Failure of Eradication in 2023. Cureus. 15(9):e44767.


Comments are closed.