Trends and distribution of acute flaccid paralysis cases and their outcomes among children below 15 years, Uganda, 2016–2023
Authors: Emmanuel Okiror Okello *1,2, Immaculate Ampaire2, Fred Nsubuga2, Sam Ofori2, Brenda Simbwa Nakafero2, Molly Birungi3, Peter Eliku3, Emmanuel Tenywa4, Annet Kisakye4, Hildah Tendo Nansikombi1, Richard Migisha1, Benon Kwesiga1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Uganda Expanded Program on Immunization, Ministry of Health Uganda, Kampala, Uganda,3Uganda Virus Research Institute, 4The World Health Organization, Uganda country office *Correspondence: Tel: +256 776 353542, Email: okiroreo@uniph.go.ug
Summary
Background: Uganda, in line with the global efforts to eradicate polio by 2026 identifies, investigates, and reports acute flaccid paralysis (AFP) cases among children <15 years for timely detection of polio. We analyzed secondary data from 2016–2023 to describe the demographic and clinical characteristics of AFP cases; determine trends and spatiotemporal distribution, and assess physical and laboratory outcomes of AFP cases in children under 15 in Uganda.
Methods: We conducted a retrospective study of secondary data archived in the EPI laboratory at UVRI of all AFP case samples tested in the country from January 2016 to December 2023. Our outcome variables included demographic characteristics, clinical characteristics, non-polio AFP (NPAFP) rates, physical and laboratory outcomes of AFP cases. Descriptive information was interpreted using frequencies, proportions and rates. We compared NPAFP rates across study years using trend analysis in STATA.
Results: A total of 6,409 AFP cases were cumulatively reported in the 8-years period. Of these, 5,837 (97%) were true AFP cases and 5,687 (89%) were detected early. The majority (59%) were children <5 years and most (58%) were males with a median age of 3 years (IQR: 1-7 years). Clinically, the majority (90%) of case-patients were identified from the community (not hospitalized); (91%) had fever at onset of paralysis, (86%) had paralysis progress in 3 days, (80%) had asymmetrical paralysis. and (57%) had only one limb of their bodies paralyzed. Of 5,744 case-patients, 4,960 (77%) had received 3+ doses of oral polio vaccine and 158 (3%) had not received any dose. In each year of the study period, 99.9% of all the districts in the country had achieved an NPAFP rate of ≥1.0/100,000 children <15 years. Of the 6,405 samples tested, 154 (2%) were suspected to have poliovirus and 8 (0.1%) had non-polio enterovirus (NPENT) plus poliovirus suspected. Of the 823 case-patients followed-up after 60 days, 250 (30%) still had residual paralysis present, 5(0.6%) were lost to follow-up and 9 (1%) had died before follow-up.
Conclusion: The AFP surveillance system in the country is active and well distributed as evidenced by 99.9% of all districts each year of the 8-years study period reporting at least one AFP case. However, the targeted NPAFP rate of ≥3/100,000 children <15 years was poorly achieved in some districts throughout the study period. This calls for a need to continuously support both the passive and active surveillance systems in these districts
Introduction
Acute Flaccid Paralysis (AFP) is defined as the sudden onset of weakness/floppiness or paralysis in any part of the body of a child below 15 years of age (1). The primary purpose of AFP surveillance is to increase the chances of early detection of any variant of poliomyelitis in populations of children below 15 years. It is also one of the strategies in the efforts to globally eradicate polio worldwide by 2026 (2). Poliomyelitis is a viral infection caused by Polio virus (PV) of genus Enterovirus (3). Acute flaccid paralysis and muscle weakness from polio infection manifests when the virus attacks the central nervous system, preferentially infecting and destroying motor neurons (3).
One of the indicators used in AFP surveillance is the non-polio AFP (NPAFP) rate. It is an indicator of surveillance sensitivity. NPAFP rate represents the number of non-polio AFP cases that are detected annually per 100,000 population aged <15 years (10). Where polio is present or where polio is a threat, this target, the objective is to detect at least two cases of non-polio AFP each year for every 100,000 children <15 years in all at-risk and outbreak countries, and to detect at least three cases of non-polio AFP each year for every 100,000 children under 15 years in endemic countries and outbreak-affected areas, where Uganda belongs (10). For every AFP case identified and investigated after 14 days from onset of paralysis (late case), a mandatory 60 days follow up has to be conducted by a trained medical/clinical officer (10).
Uganda conducts both passive and active surveillance for AFP among children <15 years as a notifiable condition. From this, hundreds of AFP cases are identified, investigated and reported through the country’s surveillance system annually. We described the AFP case-patients by person, place, and time characteristics; and their physical and laboratory outcomes following the 60 days follow up.
Methods
Study setting, design, and data source: We conducted a retrospective study using AFP surveillance data generated at the Uganda Virus Research Institute (UVRI) from the entire country, January 1, 2016 to December 30, 2023. As per the integrated disease surveillance and response, a true AFP case was defined as any child under 15 years of age with a sudden onset of flaccid/floppy paralysis on any limb identified within the 60 days from onset of paralysis, or a person of any age in whom polio is suspected by a clinician. An early AFP case on the other hand was defined as one identified within 14 days from onset of paralysis. A late AFP case was one detected after 14 days from onset of paralysis. A silent district was one that had not reported any single AFP case in a calendar year contributing a Non-Polio Acute Flaccid Paralysis (NPAFP) of 0/100,000 children <15years.
Study variables, data abstraction, and analysis
We abstracted data about the demographic variables including age, sex; clinical variables including hospitalization status of the case-person, fever at onset of paralysis, progression of paralysis within 3 days after onset of paralysis, and nature of the paralysis, number of doses received from either the routine or SIAs if vaccinated. We categorized the paralyses into four types based on the limbs affected that is monoplegia, hemiplegia, diplegia and quadriplegia.
The dataset was entered into EpiInfo and STATA software for analysis. We summarized the demographic and clinical characteristics, laboratory and physical outcomes of the AFP case-patients using frequencies and percentages. To demonstrate the trends and temporal-spatial distribution of AFP case-patients over the study period, we calculated the annual NPAFP rates for each year. We calculated the annual NPAFP rate as number of reported NPAFP cases <15 years in a year divided by the total number of children <15 years of age in that year multiplied by 100,000. We utilized projected under 15 years population estimates for each year from Uganda Bureau of Statistics (UBOS) as denominators. Comparison of NPAFP rates across years within the study period was done using trend analysis in STATA. Choropleth maps were drawn to show temporal-spatial distribution of NPAFP rates in districts using QGIS software.
Ethics approval
Our study utilized routinely aggregated surveillance data with no personal identifiers complied and archived at the Uganda Virus Research Institute. The Uganda Public Health Fellowship Program is part of the National Rapid Response Team and has been granted permission to access and analyze surveillance data in the DHIS2 and other data such as survey and field investigation data to inform decision-making in the control and prevention of outbreaks and public health programming. Additionally, the Ministry of Health has also granted the program permission to disseminate the information through scientific publications. We stored the abstracted dataset in a password-protected computer and only shared it with the investigation team.
Results
Demographic and clinical characteristics of Acute Flaccid Paralysis case-patients among children <15 years, Uganda, 2016–2023
A total of 6,409 AFP cases were cumulatively reported in the 8-years period. Of these, 5,837 (97%) were true AFP cases and 5,687 (89%) were detected early. Median age of case-patients was 3 years (IQR: 1-7 years); the majority (59%) were children <5 years and males (58%).
In terms of clinical history, the majority (90%) of case-patients were identified from the community (not hospitalized). Of the 6409 case-patients, 5816 (91%) had reported fever at onset of paralysis, 5,476 (86%) reported that paralysis had progressed in 3 days and 5,097 (80%) had asymmetrical paralysis. The majority (57%) of case-patients had only one limb of their bodies paralyzed (monoplegia). Of the 4,548 case-patients, 533 (12%) had received an injection before onset of paralysis. Of the 5,744 case-patients who had revealed their OPV vaccination history, 4960 (77%) had received 3+ doses and 158 (3%) had not received any dose (Table 1).
Table 1: Demographic and clinical characteristics of Acute Flaccid Paralysis case-patients among children below 15 years, Uganda, 2016–2023
| Demographic and clinical characteristics of AFP cases | Mean proportion | |
| N=6409 | N | (%) |
| True AFP | 5,837 | 97 |
| Early cases | 5,687 | 89 |
| Late cases | 722 | 11 |
| Demographic characteristics | ||
| Age (years)* | ||
| <5 years | 3,801 | 59 |
| ≥ 5 years | 2,608 | 41 |
| Sex | ||
| Female | 2,706 | 42 |
| Male | 3,703 | 58 |
| Clinical characteristics | ||
| Hospitalization status | ||
| Yes | 431 | 10 |
| No | 3,913 | 90 |
| Clinical history | ||
| Fever at onset of paralysis | 5,816 | 91 |
| Paralysis progressed in 3 days | 5,476 | 86 |
| Paralysis Asymmetrical | 5,097 | 80 |
| Type of paralysis | ||
| Monoplegia | 3,682 | 57 |
| Right Hemiplegia | 525 | 8 |
| Left Hemiplegia | 662 | 10 |
| Upper Diplegia | 218 | 3 |
| Lower Diplegia | 1,157 | 18 |
| Quadriplegia | 165 | 3 |
| Any Injection given before paralysis (n=4,548) | ||
| Yes | 533 | 12 |
| No | 4,015 | 88 |
| Vaccination status (n=5,744) | ||
| Zero dose | 158 | 3 |
| 1–2 doses | 626 | 10 |
| 3+ doses | 4,960 | 77 |
*Median age 3 years (IQR: 1-7 years)
Trends and temporal-spatial distribution of Acute Flaccid Paralysis case-patients among children <15 years, Uganda, 2016–2023
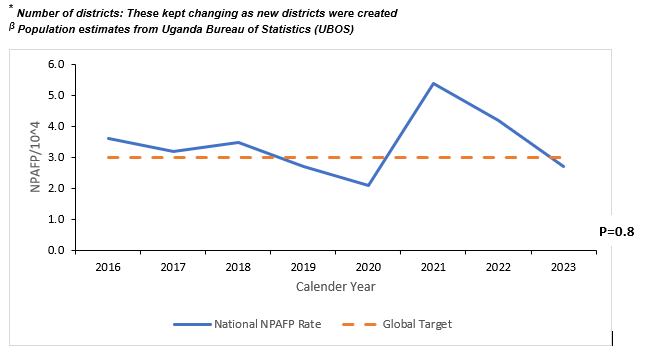
The national annual NPAFP rate was ≥3.0/100,000 children <15 years in 5 out of the 8 study years with an average of 3.4/100,000 children <15 years in the 8-years study period. There was a noted decrease in the NPAFP rate from 3.6/100,000 children <15 years in 2016 to 2.7/100,000 children <15 years with no statistically significant trend (p=0.8), (Figure 1).
Greater than 50% of all districts each year except in 2020, throughout the study period had achieved the global NPAFP rate target (≥3.0) for an endemic and outbreak prone country. In each year of the study period, 99.9% of all the districts in the country had achieved an NPAFP rate of ≥1.0/100,000 children <15 years (Table 2 and Figure 2).
Table 2: Non-polio Acute Flaccid Paralysis rate per 100,000 children below 15 years performance at districts level, Uganda, 2016–2023
| Year | <15 years populationβ | Number of Districts* | True AFP cases | National Annual NPAFP Rate | Districts with NPAFP ≥3.0 |
Districts with NPAFP <1.0 |
Silent District (s) | |||
| N=5837 | n/100,000 | N | (%) | N | (%) | N | (%) | |||
| 2016 | 19,030,648 | 112 | 679 | 3.6 | 69 | (62) | 8 | (0.07) | 1 | (0.01) |
| 2017 | 19,647,524 | 116 | 621 | 3.2 | 66 | (57) | 2 | (0.02) | 1 | (0.01) |
| 2018 | 20,281,924 | 116 | 701 | 3.5 | 79 | (68) | 2 | (0.02) | 0 | (0) |
| 2019 | 20,931,456 | 128 | 573 | 2.7 | 119 | (93) | 8 | (0.06) | 0 | (0) |
| 2020 | 21,594,820 | 135 | 456 | 2.1 | 51 | (38) | 23 | (0.2) | 2 | (0.01) |
| 2021 | 22,272,224 | 135 | 1,208 | 5.4 | 119 | (88) | 1 | (0.01) | 0 | (0) |
| 2022 | 22,962,368 | 135 | 955 | 4.2 | 101 | (75) | 3 | (0.02) | 0 | (0) |
| 2023 | 23,664,160 | 135 | 644 | 2.7 | 107 | (79) | 4 | (0.03) | 0 | (0) |
Laboratory and physical outcomes of Acute Flaccid Paralysis case-patients among children <15 years, Uganda, 2016–2023
Of the 6,405 samples tested, 154 (2%) were suspected to have poliovirus and 8 (0.1%) had Non-polio enterovirus (NPENT) plus poliovirus suspected. The majority (86.2%) of the samples tested negative.
Of the 823 case-patients followed-up, 250 (30%) still had residual paralysis present, 5(0.6%) were lost to follow-up and 9 (1%) had died before follow-up. The majority (67.9%) had made complete recovery with no residual paralysis present.
Discussion
In our study, the majority of case-patients were children <5 years of age and males by sex. Clinically, greater than three quarters of all case-patients had reported fever at onset of paralysis, had paralysis progress in 3 days, had asymmetrical paralysis and had received more than 3 doses of OPV. For each year of the study period except in 2020, greater than half of all the districts had attained an NPAFP rate greater than the recommended global NPAFP rate (≥3.0) for an endemic and outbreak prone country. There was no significant trend in the national annual NPAFP rate throughout the 8-years study period. The majority of stool samples from case-patients tested negative and only 2% were suspected for polio. Less than half of the followed-up case-patients 60 days later had residual paralysis and less than 2% had either died or were lost to follow up.
The majority (59.3%) of cases in the 8-years period were children <5 years of age and most (57.8%) were males by sex. These findings are consistent with those reported in a large dataset study in East and South Africa, also in Ghana, Nigeria and Bangladesh (12, 13, 14, 15). Infants and children <5 years who are not yet toilet-trained and also play in dirty environments are more at risk for contracting polio. This is because polio is most often spread from poor hygiene practices. This includes poor handwashing practices and ingestion of food or water that is contaminated by faeces (17). Therefore, a surveillance system such as this that captures a majority of AFP cases among this age group has more chances of early detection, reporting and investigation of a polio infection.
The majority (91%) of the cases had reported fever at onset of paralysis, (86%) reported that paralysis had progressed in 3 days, (80%) had asymmetrical paralysis and of the 5,744 case-patients who had revealed their OPV vaccination history, 4960 (77%) had received 3+ doses. Similar documentation was noted in studies conducted in Zambia and Ethiopia (21, 22). This signifies that our case-patients were actual AFPs cases and that there was good clinical history capture of the cases by the surveillance team. This good documentation is also important for follow up of contacts of such cases and for final classification by the National Polio Expert Committee (NPEC) (20).
The majority (90%) of case-patients were identified from the community (not hospitalized). Similar findings were reported in a study in Zambia (18).This underpins the importance of community-based surveillance (CBS) including the utilization of community health structures like village health teams (VHTs) and community extension workers (CHEWs) to support AFP surveillance. The World Health Organization guides that CBS is a key method to access hard-to-reach areas and communities that are not reached by the regular AFP surveillance system. Community-based surveillance is particularly useful in settings or areas at high risk of undetected poliovirus transmission or at risk of new outbreaks following importation or vaccine-derived poliovirus (VDPV) emergence (20).
The national annual NPAFP rate was ≥3.0/100,000 children <15 years in 5 out of the 8 study years with an average of 3.4/100,000 children <15 years in the 8-years study period. Other studies had similar findings with average annual NPAFP rates being above the WHO recommendation including in Zambia, Ethiopia, Ghana, Uganda and Bangladesh (21,22,13, 23,18). Overall, the country achieved the required NPAFP rate of ≥3.0/100,000 children <15 years in the 8 years period which signifies a sensitive surveillance system in an endemic and outbreak prone country. The drop in the rate noted in 2019 and 2020 is largely attributable to disruption in surveillance and health services caused by the COVID-19 pandemic (21).
Greater than 50% of all districts each year except in 2020, throughout the study period had achieved the global NPAFP rate target (≥3.0) for an endemic and outbreak prone country. In each year of the study period, 99.9% of all the districts in the country had achieved an NPAFP rate of ≥1.0/100,000 children <15 years. Another study in Uganda had similar findings though the researchers used the ambitious national target of ≥4.0/100,000 children <15 years (21). In October 2006, Uganda was declared polio free after 10 years of not reporting any indigenous cases of polio (22). But since then there have been pockets of outbreaks of polio in different parts of country, most being imported from the neighboring countries and from environmental surveillance. For this reason, the country is still considered endemic and outbreak prone and is recommended by WHO to have an NPAFP rate of ≥3.0 per 100,000 population of children <15 years per annum (20). Despite some districts not achieving the required NPAFP rate (≥3.0), these findings are indicative of a sensitive AFP surveillance system in the country.
Of the 6,405 samples tested, 154 (2%) were suspected to have poliovirus and 8 (0.1%) had NPENT plus poliovirus suspected. Poliovirus is the most sought cause of paralysis among children <15 years of age but there are other etiologies too. Poliovirus is of genus enterovirus, the spinal type presents with asymmetric paralysis that most often involves the legs and the bulbar polio leads to weakness of muscles innervated by cranial nerves (3). Several studies have as well implicated non-polio enteroviruses (NPENT) in AFP including enterovirus 71 (EV-A71), enterovirus-D68 (EV-D68), Japanese encephalitis and West Nile virus (6, 7, 8, 9). This implies that these enteroviruses are circulating among the Ugandan communities and causing paralysis. Therefore, it is important to have definitive laboratory tests to pinpoint the specific enteroviruses for easy management
Of the 823 case-patients followed-up, 250 (30%) still had residual paralysis present, 5(0.6%) were lost to follow-up and 9 (1%) had died before follow-up. Many studies have shown similar findings (10, 11, 13). According to WHO, a case that has inadequate stool specimens (late case) and has residual paralysis after 60 days of onset of paralysis or the patient is lost to follow up or dies within 60 days of symptom is classified as compatible with polio. Presence of such cases that are compatible for polio implies possibility of presence of actual polio virus variants and surveillance should keep the vigilance and investigate all AFP cases diligently.
Study limitations
Some variables had missing data elements for example, of the 6409 case-patients reported, 29% had not answered the question on having had an injection before onset of paralysis. Also, there could have been misclassification bias during entry of the primary data which is hard to adjust in secondary data. However, standard operating procedures were used in entry of this data which could have reduced presence of such bias.
Conclusion
The AFP surveillance system in the country is active and well distributed as evidenced by a large proportion of AFP being detected early and nearly all districts each year of the 8-years study period reporting at least one AFP case. The majority of case-patients identified were true AFP cases; most were detected from the community, had received >3 doses of OPV and had only one limb of their bodies paralyzed. A few case-patients were compatible for Polio. However, the presences of such case-patients underpin the importance of a continued surveillance for AFP to improve the chances of early detection of actual polio cases.
For districts that consistently failed to achieve the required NPAFP rates, we recommend the following as measures to improve identification, investigation and reporting of AFP cases; i) Intensify active case search for AFP in both health facilities and communities. This can be done by utilizing existing surveillance structures in the health facilities and communities such as health facility/health sub-district surveillance focal persons, village health team members; ii) Absorb and integrate private health facilities including physiotherapy and massage centers as well as other informal points of health care such as traditional healers, bone setter in surveillance for AFP. Many AFP cases seek for care; iii) Intensify community mobilization and sensitization for AFP surveillance. Findings from our study highlight that the majority of AFP were not hospitalized. This means that these cases were detected in the community. It is therefore important to have the community members involved in active identification and reporting of any AFP in their communities.
There was a lot of missing data on some important variables, for example, of the 6409 case-persons reported, only 4,548 of them answered the question on having had an injection before onset of paralysis. To mitigate such, it is important for surveillance officers to use standard case investigation forms and make sure that they are filled completely.
Conflict of interests
The authors declare no conflict of.
Authors’ contributions
EOO conceptualized the study idea, obtained data, analyzed it, and wrote the manuscript. IM, FN, SO, BSN, MB, PE, ET, AK, HT, RM, BK, and ARA participated in editing and reviewing the bulletin article to ensure scientific integrity and intellectual content. All the authors contributed to the final draft of the bulletin.
Acknowledgement
We appreciate all the co-authors and we to acknowledge their respective organizations including Uganda Virus Research Institute, UNEPI, WHO and UNIPH for their technical support and the US CDC for funding this investigation. We also want to acknowledge and appreciate all the surveillance officers in the country for their tireless efforts to detect and investigate all AFP cases in their catchment areas.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
Reference
- WHO_EPI_GEN_98.01_Rev.2.pdf [Internet]. [cited 2024 Mar 3]. Available from: https://iris.who.int/bitstream/handle/10665/64165/WHO_EPI_GEN_98.01_Rev.2.pdf?sequence=1
- Bandyopadhyay AS, Macklin GR. Global Polio Eradication: Progress and Challenges. In: Ahmad SI, editor. Human Viruses: Diseases, Treatments and Vaccines : The New Insights [Internet]. Cham: Springer International Publishing; 2021 [cited 2024 Mar 3]. p. 629–49. Available from: https://doi.org/10.1007/978-3-030-71165-8_30
- Singh R, Monga AK, Bais S. Polio: a review. Int J Pharm Sci Res. 2013;4(5):1714.
- Laffont I, Julia M, Tiffreau V, Yelnik A, Herisson C, Pelissier J. Aging and sequelae of poliomyelitis. Ann Phys Rehabil Med. 2010 Feb 1;53(1):24–33.
- Jin C qiang, Dong H xin, Sun Z xiang, Zhou J wei, Dou C yun, Lu S hua, et al. Acute immune thrombocytopenic purpura as adverse reaction to oral polio vaccine (OPV). Hum Vaccines Immunother. 2013 Aug 8;9(8):1739–40.
- Poliomyelitis [Internet]. [cited 2024 Nov 23]. Available from: https://www.who.int/news-room/fact-sheets/detail/poliomyelitis
- Namageyo-Funa A, Greene SA, Henderson E, Traoré MA, Shaukat S, Bigouette JP, et al. Update on Vaccine-Derived Poliovirus Outbreaks — Worldwide, January 2023–June 2024. 2024;73(41).
- Uganda in mass polio immunization following outbreak | WHO | Regional Office for Africa [Internet]. 2024 [cited 2024 Nov 24]. Available from: https://www.afro.who.int/news/uganda-mass-polio-immunization-following-outbreak
- POLIO OUTBREAK CONFIRMED IN UGANDA | Uganda Virus Research Institute [Internet]. [cited 2024 Nov 24]. Available from: https://www.uvri.go.ug/news/polio-outbreak-confirmed-uganda
- Global-AFP-guidelines-pre-publiucation-version-2023.pdf [Internet]. [cited 2024 Apr 20]. Available from: https://polioeradication.org/wp-content/uploads/2023/03/Global-AFP-guidelines-pre-publiucation-version-2023.pdf
- Uganda Demographics 2023 (Population, Age, Sex, Trends) – Worldometer [Internet]. [cited 2024 Apr 16]. Available from: https://www.worldometers.info/demographics/uganda-demographics/
- Manyanga D, Byabamazima C, Masvikeni B, Daniel F. Assessment of acute flaccid paralysis surveillance performance in East and Southern African countries 2012 – 2019. Pan Afr Med J [Internet]. 2020 Jun 8 [cited 2024 Sep 7];36(1). Available from: https://www.ajol.info/index.php/pamj/article/view/211382
- Odoom JK, Ntim NAA, Sarkodie B, Addo J, Minta-Asare K, Obodai E, et al. Evaluation of AFP surveillance indicators in polio-free Ghana, 2009–2013. BMC Public Health. 2014 Dec;14(1):687.
- Raji IA, Abubakar AU, Ahmad A, Gidado S, Olorukooba AA, Lawal BB, et al. Evaluation of acute flaccid paralysis surveillance indicators in Sokoto state, Nigeria, 2012–2019: a secondary data analysis. BMC Public Health. 2021 Jun 15;21(1):1148.
- Habib KR. Polio Eradication in Bangladesh: Evaluation of AFP Surveillance Indicators, 2011-2015. Int J Immunol. 2017 Feb;13(3):11–9.
- Chirambo RM, Baboo KS, Siziya S. Performance of acute flaccid paralysis surveillance system in Zambia: 2000 to 2009-analysis of secondary data. Int J Public Health Epidemiol. 2014;3(10):075–81.
- Fast facts about poliomyelitis (polio) | UNICEF Sudan [Internet]. [cited 2024 Sep 20]. Available from: https://www.unicef.org/sudan/stories/fast-facts-about-poliomyelitis-polio
- Bessing B, Dagoe EA, Tembo D, Mwangombe A, Kanyanga MK, Manneh F, et al. Evaluation of the Acute flaccid paralysis surveillance indicators in Zambia from 2015–2021: a retrospective analysis. BMC Public Health. 2023 Nov 12;23:2227.
- Tegegne AA, Fiona B, Shebeshi ME, Hailemariam FT, Aregay AK, Beyene B, et al. Analysis of acute flaccid paralysis surveillance in Ethiopia, 2005-2015: progress and challenges. Pan Afr Med J. 2017 Jun 9;27(Suppl 2):10.
- Global-AFP-guidelines-pre-publiucation-version-2023.pdf [Internet]. [cited 2024 Sep 4]. Available from: https://polioeradication.org/wp-content/uploads/2023/03/Global-AFP-guidelines-pre-publiucation-version-2023.pdf
- Amodan BO, Kisakye A, Okumu PT, Ahirirwe SR, Kadobera D, Driwale A, et al. Trends of key surveillance performance indicators of acute flaccid paralysis: a descriptive analysis, Uganda, 2015–2020. BMC Public Health. 2022 Sep 7;22:1694.
- Uganda IPV Polio Fact Sheet.pdf [Internet]. [cited 2024 Sep 15]. Available from: https://www.unicef.org/uganda/media/3271/file/Uganda%20IPV%20Polio%20Fact%20Sheet.pdf
- Solomon T, Willison H. Infectious causes of acute flaccid paralysis. Curr Opin Infect Dis. 2003 Oct;16(5):375.
- Bitnun A, Yeh EA. Acute Flaccid Paralysis and Enteroviral Infections. Curr Infect Dis Rep. 2018 Jun 29;20(9):34.
- Sejvar JJ, Lopez AS, Cortese MM, Leshem E, Pastula DM, Miller L, et al. Acute flaccid myelitis in the United States, August–December 2014: results of nationwide surveillance. Clin Infect Dis. 2016;63(6):737–45.
- Turgay C, Emine T, Ozlem K, Muhammet SP, Haydar AT. A rare cause of acute flaccid paralysis: human coronaviruses. J Pediatr Neurosci. 2015;10(3):280.
- Van Haren K, Ayscue P, Waubant E, Clayton A, Sheriff H, Yagi S, et al. Acute flaccid myelitis of unknown etiology in California, 2012-2015. Jama. 2015;314(24):2663–71.
- Kaushik R, Kharbanda PS, Bhalla A, Rajan R, Prabhakar S. Acute Flaccid paralysis in adults: Our experience. J Emerg Trauma Shock. 2014;7(3):149.


Comments are closed.