The Malaria Outbreak in Northern Uganda
Authors: Allen Eva Okullo and Myers Lugemwa; Affiliations: Malaria Control Program, Ministry of Health
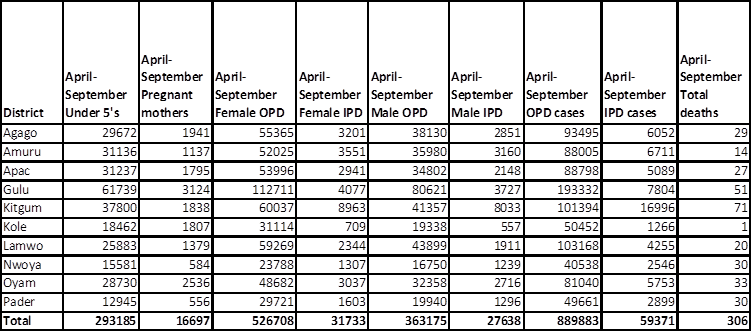
On July 9 2015, the Director General, Ministry of Health, Dr. Aceng Ruth gave a press release confirming a malaria outbreak in Northern Uganda [1]. The ten districts affected were: Nwoya, Amuru, Gulu, Kitgum, Lamwo, Pader, Agago, Apac, Oyam and Kole. Important to note is the fact that these are the same districts that had undergone Indoor Residual Spraying (IRS) over the last five years, IRS having been stopped in November 2014. This epidemic has claimed about 306 lives between April and September 2015, affected close to one million people with tens of thousands health facility admissions in the same period as shown in the table 1 below. The suspected outbreak was initially reported to the Malaria Control Program, Ministry of Health, by some of the affected districts in early June 2015. MOH respond- ed by sending a rapid response team (RRT) to confirm and respond to the outbreak in the affected districts. The RRT followed the Epidemic Preparedness and Response guidelines in reactivating the respective District Task Forces in collaboration with implementing Partners to provide support. The preparedness of the districts and health facilities to provide case management was assessed and used to fill the gaps.
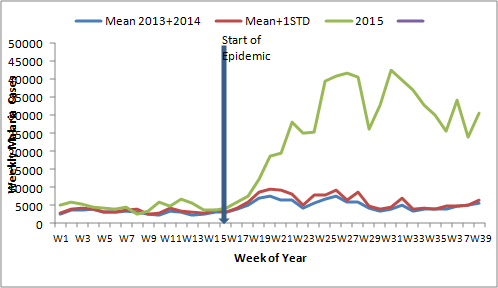
The Public Health Emergency Operation Center (PHEOC) was activated and a National Task Force (NTF) activated place to mobilize resources, give technical guidance and oversight, monitor and coordinate response activities by various implementing partners. This would be led by the Incident Management Team, and chaired by the Incident Commander and Pro- gram Manager, Malaria Control Program, Dr. Albert Peter Okui (RIP). Stakeholders from various implementing partners such as WHO, PMI-USAID, MSF, UNICEF, Malaria Consortium, USAID-ASSIST, USAID-CHC, Nakasero Blood Bank, along with the Ministry of Health teams formed the NTF. Overtime, the malaria cases in the epidemic districts started to decline as shown in the malaria normal channel graph( figure1). This decline could be attributed to the interventions put in place by MOH and various implementing partners. There is also a possibility that the gradual drop in the number of malaria cases could have been due to the change in malaria sea- sonality, as is usually the case.
Interventions implemented included:
- Onsite technical assistance at the districts by the MOH rapid response teams supported by WHO, Malaria Consortium, Makerere University School of Public Health -/Public Health Fellowship Program supported by
- Activation of district epidemic management task force with the Surveillance, Logistics and Behavioural Change and Communication (BCC) sub- committees by the MOH rapid response
- Intensified surveillance in the 10 epidemic districts by the MOH Emergency Operation
- Training of VHTs in the most affected sub counties in Mass Fever Treatment by PMI-USAID
- The provision of Anti-malarials from Joint Medical Stores to 72 most affected sub counties in the 10 districts for mass fever treatment by PMI-USAID.
- Intensified Behavioural Change Communication (BCC) in all 10 districts through various media channels and local leaders within the community by CHC-USAID.
- Emergency stock up of supply of anti-malarials within facilities for rapid treatment to reduce dis- ease burden and reduce mortality by
- Provision of 34,000 Long Lasting Insecticide treated Nets (LLINs) to the most affected sub-counties by PMI-USAID.
- Comprehensive malaria outbreak support to Kole district by
- Reactivation of the community VHTs stocked with anti-malarials and rapid diagnostic tests
- Scaling up blood supply to meet the need in the affected districts by the Uganda blood
- Direct support to the affected districts in monetary terms by UNICEF and MOH
- Training of health facility staff on integrated management of severe malaria by USAID-ASSIST
Though the malaria burden seems to be coming down, it is imperative that action is taken to prevent the recurrence of an upsurge especially given the El Nino rains alert. El Nino has been shown to have several health implications among which are an increase in malaria cases to epidemic levels. To sustain these achievements thus far, it is important that surveillance is intensified in every district to quickly pick up any upsurges and mount targeted interventions. This should be, hand in hand with case management of all malaria cases at health facilities and within communities and BCC in the communities.


Comments are closed.