Risk factors for Podoconiosis, Kamwenge District September 2015
Authors: By Christine Kihembo,1,2 B. Masiira,1,2 W. Z. Lari3, G. Matwale4, A. R. Ario5, M. Musenero2, M. Nanyunja,3; Affiliations: 1Public Health Fellowship Program – Field Epidemiology Track; 2Epidemiology and Surveillance Division, Ministry of Health, Uganda; 3World Health Organization, Uganda Country Office; 4Vector Control Division, Ministry of Health, Uganda
In September 2015, following alerts of increased elephantiasis cases in Kamwenge District, we set out to confirm the diagnosis and identify risk factors for the illness to guide control efforts. Using standard case definitions we identified cases in affected communities and ruled out filariasis. In a case-control study we compared shoe use and feet-washing practices among 40 probable case-persons and 80 asymptomatic neighborhood control-persons, matched by age and sex. We identified 52suspected cases in 2 sub-counties including 40 probable cases; incidence=2.9/100,000/year (1980-2015). There was no apparent increase in cases over time. Case control findings showed that not wearing shoes at work and at home and delay in feet washing after work were significantly associated with development of Podoconiosis ( ORMH= 7.7; 95% CI:2.0- 30). We verified that the reported elephantiasis was Podoconiosis, associated with prolonged foot exposure to soil. We recommended health education on foot protection and provision of protective shoes to Kamwenge residents.
Introduction: Podoconiosis is non-filarial elephantiasis char- acterized by asymmetrical lower limb lymphedema[1]. Podoconiosis is one of the neglected diseases yet it causes high levels of disability, reduced productivity and social stigma[2]. The disease is prevalent in the tropics with a prevalence of 5–10% among populations who work bare-foot on irritant volcanic soils[3]. In Uganda, the disease has been reported in Kapchorwa along Mt Elgon slopes and in Kabale district. Podoconiosis has never been documented in Kamwenge or surrounding districts[4].
In 2014, the World Health Organization (WHO) Uganda Country office was alerted of increased cases of elephantiasis Kamwenge district. A subsequent filarial mapping exercise ruled out filaria- sis. In August 2015, the WHO office received another alert of increasing cases of elephantiasis in Kamwenge district. The Ministry of Health (MOH) in collaboration WHO Uganda set up a team to identify the cause and risk factors for disease development in order to guide control interventions.
Materials and Methods: We conducted the investigation in Kamwenge and Busiriba sub-counties in Kamwenge district. Kamwenge district is located in Western Uganda and has a total
population of 421,470 who are mainly involved in subsistence farming. Kamwenge is generally hilly with deep rich fertile volcanic soils. We defined a Podoconiosis suspected case-person as a Kam- wenge resident with bilateral asymmetrical swelling of lower limbs lasting ≥1month, plus ≥1 of the following: skin itching, burning sensation, plantar oedema, lymph-ooze, prominent skin markings, rigid toes, mossy papillomata. We collected approximately 2ml of venous blood and tested for filarial antigen using the immuno-chromatographic card test (ICT). A probable case was a suspected case with negative microfilaria antigen ICT result. Between 22nd-29th September 2015, we conducted active case- finding in the affected communities.
Using standard questionnaires we interviewed initial case- persons and generated hypotheses. We tested the hypotheses in a matched case-control study and compared shoe use and feet- washing practices among 40 probable case-persons and 80 asymptomatic neighborhood control-persons, matched by sex and age (±5 years).
We collected five (5) soil samples at the surface and depth of 0.5 m from places around their homesteads where case-persons significant amount of time for free silicon and pH testing.
Results: By 31st September2015, we identified 52 suspected cases of Podoconiosis including 40 probable cases from Busiriba and Kamwenge sub-counties. The annual incidence rate based on the suspected cases was 2.9/100,000/year (1980-2015). Older people were more affected, mean aged 48 years, range 13-80 years. More females were affected with attack rate (AR) of 1.9/ 10,000 compared to
0.22/10,000 among Males.

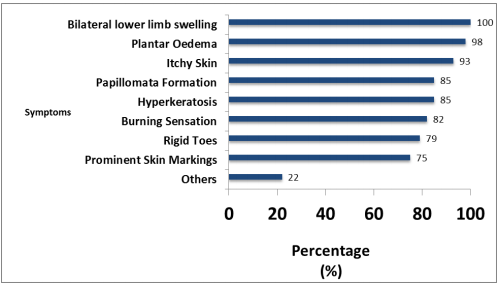
The commonest symptoms were plantar edema and lower limb skin itching. There was no genital involvement. Busiriba sub-county was more affected (AR 1.29/1000) com- pared (AR 0.65/1000) in Kamwenge sub-county (figure1).
The epidemic curve showed stable number of cases over time (figure 1).
All case-persons resided in areas with a relatively high altitude (median: 1263m above sea level; range: 1163-1328m).

Hypothesis generation:
Interview of 24 initial case-persons revealed that;
- all (100%) were farmers engaged in digging and growing various crops;
- 14 (63%) never wore shoes while at work and
- 16 (67%) only washed their feet at the end of the day as they retired to bed and never washed their feet during the day
Case-control study findings:
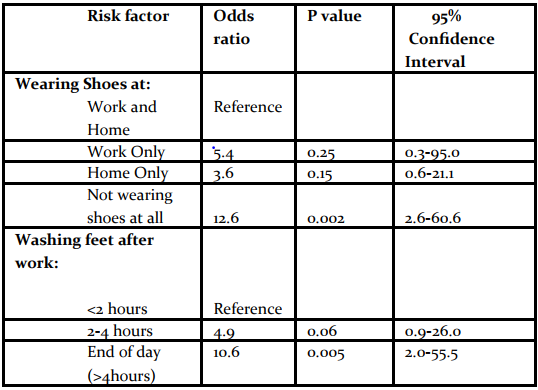
Not wearing shoes at work was significantly associated with the illness (odds ratio [OR]MH= 7.7; 95% Confidence Interval [CI] 2.0-30); so was not wearing shoes at home (ORMH= 5.2, 95% CI;1.8-15) (Table 2).
On stratified analysis, not wearing shoes neither at work nor at home 13 times more associated with developing Podoconiosis compared with wearing shoes both at work and at home (ORMH= 13, 95 % CI; 2.6-61).
Similarly, only washing feet at the end of the day as they retired to bed (compared to washing feet within 2 hours after working in the fields) was associated with elevated disease odds (ORMH= 11; 95% CI; 2.0- 56).
Illness status was not significantly associated with the type, structure, or cover of the floor at the participant’s homes or kitchen, nor with cultivating activities in valley areas or cultivating activities in the areas adjacent to the Kibaale Forest.
Much as more case-persons reported knowing at least one family member who had experienced similar symptoms, the association was not statistically significant when stratified in line of blood relations.
Laboratory findings: 40 suspected case-patients underwent ICT testing and all of them (100%) tested negative for filarial antigen on ICTs.
Soil analysis: Results pending, however soils in Kamwenge have been described as deep rich volcanic soils.
Discussion: Podoconiosis has been documented to be as a result of interplay between environmental risk and personal factors that predispose an individual to prolonged exposure with irritant soils[2, 5, 6].
In this study we found that much as there were no differences in occupation among cases and controls, not wearing shoes while at work or at home before onset of the disease was strongly associated with disease. More still those who wore gumboots while at work where there is maximum risk of exposure, and those who washed to get rid of soil from their skins by quickly washing their feet were less at risk of Podoconiosis.
This is in keeping with previous studies conducted in Ethiopia[7-9]. Unlike in the previous studies, this study however found no association between floor cover and disease.
Podoconiosis has been noted to have a genetic predisposition. Our investigation also found family clustering of the disease[3]. Much as more case -persons reported knowing at least one family member who had experienced similar symptoms, the association was not statistically significant when stratified in line of blood relations. The observed clustering could therefore be explained by family members being experiencing same risk factors.
Important to note is the fact that much as the case patients were observed to be using shoes after disease had been established, children and the general population in Kamwenge remained at risk, going about their business while with bare feet. Moreover, household members and other members of the public interfaced with during the study expressed not being in position to afford gumboots or shoes.


Comments are closed.