Rapid containment of an Mpox outbreak, Uganda, Masindi Prison, June-October 2024
Authors: Janet Kobusinge Lubega 1, Emmanuel Mfitundinda 1, Emmanuel Okiror Okello 1, Cranima Turyakira 2, Mugasha Felix 2, Richard Migisha1, Benon Kwesiga1, Alex Riolexus Ario1 1Uganda Public Health Fellowship Program-Field Epidemiology Training Program, Uganda National Institute of Public Health, Kampala, Uganda, 2 Masindi Main Prison Correspondence*: Tel: +256 772 773664896, Email: jklubega@uniph.go.ug
Summary
Background: On 6 October 2024, the Ministry of Health (MoH) Uganda was notified of an Mpox outbreak in Masindi Prison. Given the high-risk nature of correctional facilities, where overcrowding and limited healthcare access facilitate disease spread, an investigation was conducted to determine to describe the outbreak, trace its source, evaluate containment measures, and recommend strategies for control and prevention.
Methods: We defined suspected and confirmed cases as per the MoH Uganda case definitions. Cases were identified through health record reviews, active case finding, and environmental assessments. We conducted contact tracing to establish links to potential sources. To describe the outbreak, we performed descriptive analysis of the cases.
Results: Two confirmed and 26 suspected Mpox cases were identified in Masindi Main Prison, with no reported deaths. The outbreak originated from two detainees arrested in Kijunjubwa Sub-County, an area with suspected community transmission, and transferred to the prison on 6 August 2024. The first suspected case appeared on 9 August, and the last on 20 October 2024. Despite high inmate density, the outbreak was officially declared contained on 14 November 2024, following two full incubation periods without new cases. We achieved rapid containment within 72 days through prompt implementation of infection control and surveillance measures. These included daily triage, active case finding, onsite sample collection, isolation of cases, improved hygiene practices, disinfection of shared items, provision of PPE, movement restrictions, staff training, and risk communication.
Conclusion: Early detection and swift containment measures limited Mpox spread in Masindi Prison. The rapid setup of surveillance, case isolation, improved hygiene, and onsite sample collection ensured timely intervention. Additional measures, including movement restrictions, disinfection of shared spaces, and staff sensitization, helped control the outbreak. Strengthening surveillance, improving prison sanitation, enforcing hygiene protocols, and enhancing pre-transfer screening for inmates are essential to mitigating future outbreaks in prison settings.
Background
Mpox, formerly known as monkeypox, is a zoonotic viral disease closely related to small pox but milder(1). Mpox was first identified in humans in Democratic Republic of Congo (DRC) in 1970 and periodically poses as a public health challenge due to its capacity for both zoonotic and human-to-human(2). Contributing factors to the spread of mpox has been attributed to key drivers of mpox transmission include environmental and socio-economic factors, such as climate change, habitat land use shifts, increased population density, cross-species contact, and globalization as well as its transmission through transnational tourism, animal movements and trade(2, 3).
On July 24, 2022, WHO declared mpox a global public health threat after a May 2022 outbreak that demonstrated its capacity to spread worldwide beyond its endemic regions in Central and West Africa (4). Uganda confirmed its first Mpox cases of the year in Kasese District, marking the beginning of a new wave of infections. On October 6, 2024, Masindi Prison reported its first two cases, drawing attention to the vulnerability of prison settings in facilitating disease transmission. Shortly after, Hoima District confirmed its first Mpox case on October 20, 2024.
Prison environments are characterized by high population densities, limited healthcare access, restricted ventilation, and frequent inmate transfers, all of which contribute to an increased risk of infectious disease outbreaks. We assessed the extent of the outbreak in Masindi prison and district, profiled confirmed cases, and evaluated public health interventions aimed at curbing transmission.
Methods
Outbreak area
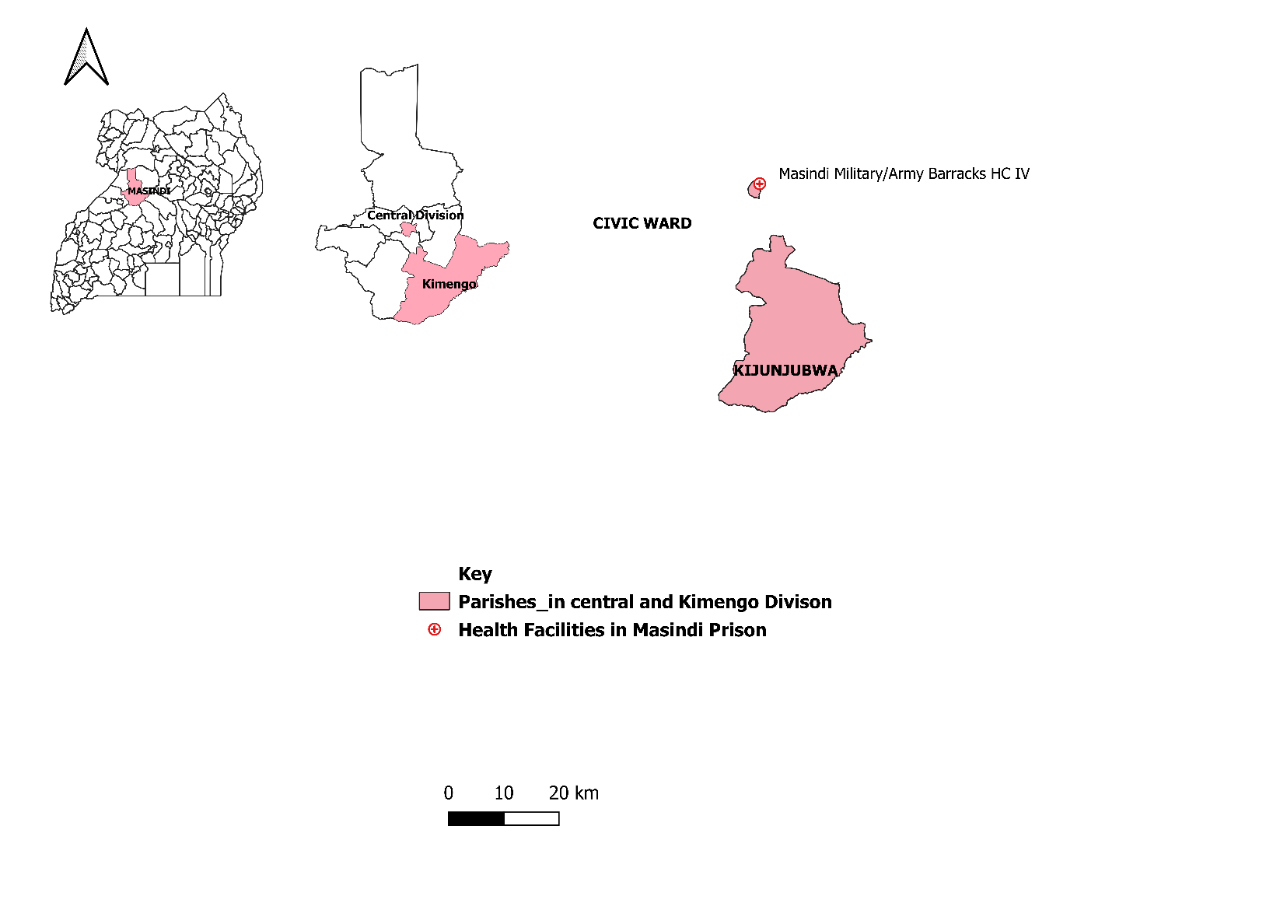
The outbreak occurred in Masindi District, located in Uganda’s Western Region. The district borders Nwoya to the north, Kiryandongo to the east, Nakasongola to the southeast, Kyankwanzi to the south, Hoima to the southwest, and Buliisa to the west all of which had experienced a surge of mpox cases. We focused the investigation on Uganda Government Prison Masindi, a high-security correction facility in Central Division, Masindi Municipality served by Masindi Prison Health Center III. The prison holds a large number of inmates under congested conditions, where prisoners share sleeping areas, have limited healthcare access, and experience restricted movement, increasing the risk of disease outbreaks. The facility consists of 18 blocks and two wards, each accommodating an average of 80 to 160 prisoners. New prisoners undergo triage at the ward near the entrance and spend 24 hours in the holding unit before admission.
Case definition and finding
Case identification involved reviewing prison health facility records, conducting active surveillance, and interviewing healthcare personnel. The study applied the World Health Organization’s suspected, probable, and confirmed case definitions for Mpox.
Laboratory investigations
We collected samples from suspected cases, including skin lesion swabs, oropharyngeal swabs, genital and rectal swabs and saliva. Laboratory analysis was conducted using real-time polymerase chain reaction (RT-PCR) to detect Mpox virus-specific DNA sequences.
Descriptive epidemiology
We constructed an epidemic curve to determine the distribution of mpox cases over time and described the distribution of signs and symptoms of the inmates fitting the case definition.
Environmental assessment
We visited the prison to conduct a physical inspection. We examined the overall layout of the facility, paying close attention to living conditions, available space, and hygiene infrastructure. Observations were made regarding how inmates were housed, their access to hygiene materials, and the state of sanitation facilities. We measured the capacity of the prison in comparison to the actual number of inmates. We reviewed the spacing arrangements and identified how inmates were accommodated within the available space. Special attention was given to whether isolation areas were designated for suspected cases. We examined the availability of essential hygiene materials, such as soap and clean water. We also reviewed the waste management system, inspecting sanitation facilities, including latrines, to assess their adequacy in maintaining cleanliness and preventing environmental contamination. The assessment included a review of infection prevention and control measures in place. This involved examining protocols for isolating suspected cases, assessing hygiene practices among inmates, and evaluating the overall sanitation management strategies implemented within the facility.
Ethical considerations
The Ministry of Health of Uganda gave the directive to investigate this outbreak. We also sought permission from the commissioner of Prison Services who gave us approval to investigate this outbreak within the prison system. The Office of the Associate Director for Science at the US Centres for Disease Control and Prevention (CDC) Uganda determined that this research did not involve human subject research and that its primary intent was public health practice or disease control.
Results
Descriptive epidemiology
We identified a total of 28 cases: 26 suspected, 2 confirmed, and no deaths. Although the Mpox outbreak in Masindi Prison was officially detected in early October 2024 when two cases were confirmed through laboratory testing on 26 September and 3 October retrospective case tracing revealed that symptoms had first appeared in early August. These earlier cases were among newly admitted detainees, indicating that transmission had begun weeks before confirmation. The outbreak was ultimately traced back to Kijunjubwa Sub-County, where suspected community transmission was ongoing. This conclusion was supported by an active case search that identified additional cases in the community and confirmed Kijunjubwa as the likely source of introduction (Figure 1).
On August 3, 2024, two individuals, identified as Detainee X and Detainee Y, were arrested for theft at Royal Ranch in Kijunjubwa Sub-County and detained at Kijunjubwa police post. Three days later, on August 6, 2024, they were transferred to Masindi Main Prison as newly admitted inmates.
One of them had previously worked at Royal Ranch as a cattle keeper, where he reported seeing a few people in the area with an unexplained rash illness before his arrest. Although neither detainee showed symptoms upon arrival at the prison, both developed a rash, fever, and body aches by August 8, 2024. The medical records show that the prison health team diagnosed and treated them for chicken pox.
First suspected inmate case
On August 10, 2024, an 18-year-old inmate, referred to as Detainee T, developed an itchy rash, fever, and swollen lymph nodes. It was discovered that Detainee T had close contact with Detainee X and Detainee Y, including sharing clothing without washing it. This marked the first suspected case of Mpox within the general prison population.
Subsequently, additional 23 suspected cases emerged among inmates as of October 2024, reinforcing the likelihood that the virus had already been circulating within Masindi Prison before detection.
On October 6, 2024, a prisoner E, who had recently been transferred from Masindi Prison to Nakasongola Prison developed Mpox symptoms on October 8,2024. His case was confirmed on October 9,2024 through PCR testing, raising concerns that Masindi Prison had been experiencing undetected transmission before his transfer. This event triggered a full review of cases at Masindi Prison previously diagnosed as chicken pox.
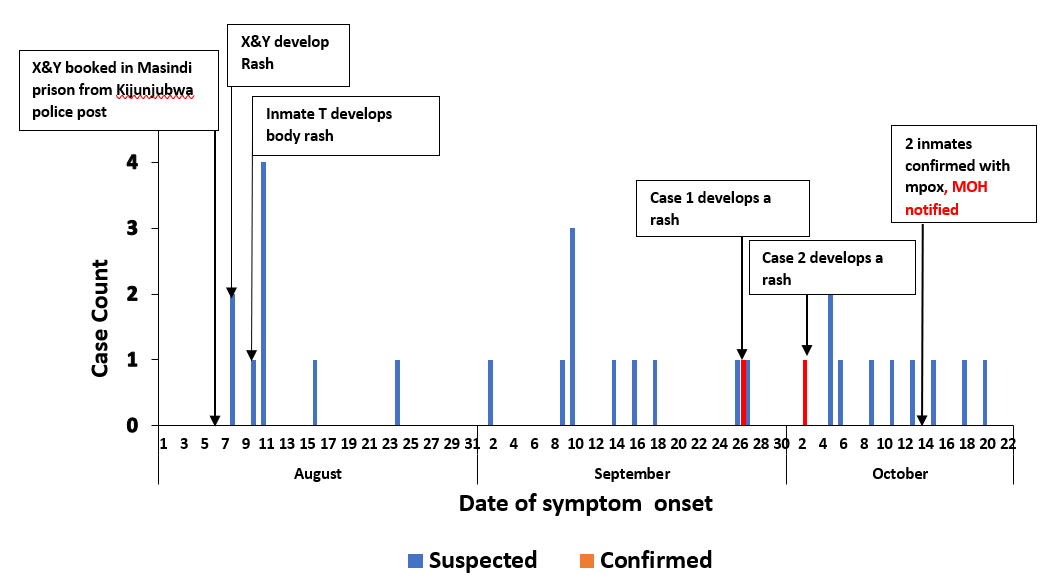
Following the confirmed case from the inmate transferred from Masindi to Nakasongola, the doctor in charge of Masindi Prison suspected an Mpox outbreak, when on September 26, 27 and October 3, 2024, suspects developed a generalized itchy rash. In response, samples were collected from three suspected inmates on October 10, 2024.On October 14, 2024, two cases were confirmed through PCR testing, officially verifying the presence of Mpox in Masindi Prison. These cases were later referred to as Case 1 and Case 2 and Ministry of health was notified of an outbreak of mpox in Masindi prison.
The first confirmed case of Mpox in Masindi Prison, Case 1, began experiencing prodromal symptoms, including headache, fever, and chills, on September 26, 2024. By September 27, 2024, an itchy rash appeared on his face, later spreading to the arms, back, chest, and scalp. A sample was collected on October 9, 2024, and results confirmed Mpox on October 14, 2024. By October 16, 2024, the patient was healing and requested discharge from isolation.
The second confirmed case, Case 2, had a more severe presentation. On October 3, 2024, the inmate developed prodromal symptoms, including headache, fever, chills, sore throat, and sensitivity to light. By October 3, 2024, a papular rash appeared on the abdomen, later bursting to release fluids and spreading to other body parts, including the mouth, penis, and anus, causing anorectal pain. A sample was collected on October 9, 2024, and results confirmed Mpox on October 14, 2024. By October 16, 2024, he was recovering, though a few new lesions were still appearing.
Containment measures and outbreak control
Early containment efforts were challenged by delayed recognition of the outbreak. Although symptomatic cases began to emerge in August and September, they were initially misdiagnosed, and the outbreak remained undetected. Limited diagnostic capacity and overlapping symptoms with other rash illnesses hindered early identification. It was not until early October, following a confirmed Mpox case in a transferred inmate, that a formal investigation was launched and containment efforts were initiated.
From October 10 to 15, immediate response measures were implemented. An isolation unit was established within the prison to separate confirmed and suspected cases from the general population. Daily triage was introduced to screen inmates for Mpox symptoms, and active case finding was initiated across the facility. Onsite sample collection was also organized to facilitate rapid testing and confirmation of suspected cases.
Between October 17 and 20, infection prevention and hygiene measures were intensified. All inmates were required to take mandatory showers, and the prison’s water supply was improved to support hygiene practices. Shared items such as uniforms and bedding were disinfected regularly, and personal protective equipment (PPE) was provided to healthcare workers to minimize their risk of exposure during clinical care and surveillance activities.
From October 23 onward, movement restrictions were enforced to prevent cross-contact between different groups of inmates. Prison staff received training on Mpox identification, isolation protocols, and infection prevention measures. Risk communication and hygiene promotion activities were scaled up, increasing awareness among inmates and staff and reinforcing adherence to the containment guidelines.
The last suspected case was identified on October 20, and no new cases were reported thereafter. The outbreak was officially declared contained on October 31, 2024, after one full incubation period passed without additional cases. Continued monitoring and preventive measures remained in place. Overall, the outbreak was successfully contained within 72 days of the first exposure, demonstrating the effectiveness of rapid, coordinated containment interventions in a high-risk correctional setting.
Discussion
The Mpox outbreak in Masindi Prison, which resulted in 28 identified cases (26 suspected and 2 confirmed), was successfully contained within one incubation period from the last confirmed case. This outcome is significant given the vulnerability of prison environments to infectious disease outbreaks due to overcrowding, restricted movement, poor ventilation, and inadequate healthcare infrastructure (5). The WHO recognizes prisons, detention centers, and refugee camps as high-risk environments for Mpox transmission and emphasizes the need for enhanced infection control measures (6). In contrast to outbreaks such as COVID-19 and tuberculosis, which have proven difficult to control in correctional settings due to delayed detection and weak health systems (7), the Masindi outbreak was curtailed quickly through early identification, isolation, and coordinated response. The rapid response in Masindi was driven by effective surveillance, timely sample collection, and strong collaboration between prison authorities, the Ministry of Health, implementing partners, and the Central Public Health Laboratory (CPHL). These measures aligned with the WHO strategic framework, which stresses the importance of isolating suspected Mpox cases, implementing minimum infection prevention and control (IPC) standards, and integrating correctional facilities into national surveillance systems (6). The prison adopted key interventions such as routine screening, risk communication, staff training, and improved sanitation. These efforts mirror successful strategies used in controlling respiratory outbreaks like COVID-19 and influenza in other countries, such as South Korea and Taiwan, where strict quarantine, testing, and early interventions helped limit spread (5, 8). However, challenges like limited space for isolation, inadequate PPE, and under-resourced prison health systems have undermined containment efforts in other regions, including Latin America and the United States (9).
Importantly, investigations traced the likely source of infection to Kijunjubwa Sub-County, highlighting the risk of disease introduction into prisons through incoming detainees. High inmate turnover and transfer without adequate screening increase the likelihood of similar outbreaks(10). To prevent future transmission, correctional facilities must adopt sustained prevention strategies, including systematic pre-admission screening, improved IPC infrastructure, and training for prison health workers to identify and manage cases early (6, 7). Long-term measures should also include vaccination strategies, STI screening, and health education focused on high-risk behaviors, including condom distribution, as recommended in the WHO Mpox guidelines (6). Strengthening these systems will help ensure a more comprehensive and sustainable approach to disease prevention in prison settings.
Study limitations
There was also potential for recall bias regarding travel history and close contacts, as inmates may have had difficulty recalling events accurately. Social desirability bias and fear of stigma especially around sexual behavior could have led to underreporting. The prison environment itself may have limited privacy and disclosure. However, the team conducted timely interviews and ensured confidentiality to encourage honest responses.
Conclusion
This mpox outbreak likely began in early August 2024, introduced by two detainees transferred from Kijunjubwa Sub-County, an area with ongoing community transmission. All cases were male inmates who presented with classic Mpox symptoms such as fever, rash, and lymphadenopathy. Transmission had started weeks before the official detection due to early misdiagnosis as chickenpox. Rapid implementation of control measures including isolation, daily triage, improved hygiene, staff training, and active case significantly reduced further spread. Despite the crowded and high-risk environment, we successfully contained the outbreak within 72 days. To prevent future outbreaks in correctional settings, we recommend routine pre-admission screening of new inmates, continuous training of prison healthcare staff, and sustained surveillance systems within prison facilities. Strengthening infection prevention infrastructure, integrating prisons into national outbreak preparedness plans, and ensuring timely risk communication will be essential to managing emerging public health threats in similar high-risk environments.
Conflict of interests
The authors declare that they have no conflict of interest.
Authors’ contributions
JL, EM, EO, CT, FM and FM participated in the design, field investigations, data collection, analysis, and interpretation. JL led the writing of the bulletin article. BK, RM, and ARA participated in bulletin writing and review to ensure scientific integrity and intellectual content. All the authors contributed to the final draft of the bulletin.
Acknowledgement
We appreciate the management of Uganda Prisons and Masindi Local Government for the stewardship, and the community for their participation in this investigation. We also thank the Ministry of Health, Public Health Emergency Operations Centre, World Health Organization for their technical support and the US CDC for funding this investigation.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Organization WH. Mpox (monkeypox). World Health Organization. 2023.
- Ullah M, Li Y, Munib K, Zhang Z. Epidemiology, host range, and associated risk factors of monkeypox: an emerging global public health threat. Frontiers in Microbiology. 2023;14:1160984.
- Ogunleye SC, Akinsulie OC, Aborode AT, Olorunshola MM, Gbore D, Oladoye M, et al. The re-emergence and transmission of Monkeypox virus in Nigeria: the role of one health. Frontiers in Public Health. 2024;11:1334238.
- WHO Director-General’s statement at the press conference following IHR Emergency Committee regarding the multi-country outbreak of monkeypox [press release]. 23 July 2022 2022.
- Augustynowicz A, Opolski J, Borowska M, Malczyk D, Kotwas A, Bartczak-Szermer D, et al. COVID-19 control measures in correctional facilities of selected countries–A literature overview. Annals of Agricultural and Environmental Medicine. 2022;29(4):471-6.
- Organization WH. Strategic framework for enhancing prevention and control of mpox 2024-2027: World Health Organization; 2024.
- Migisha R, Morukileng J, Biribawa C, Kadobera D, Kisambu J, Bulage L, et al. Investigation of a COVID-19 outbreak at a regional prison, Northern Uganda, September 2020. Pan African Medical Journal. 2022;43(1).
- Akiyama MJ, Spaulding AC, Rich JD. Flattening the curve for incarcerated populations—Covid-19 in jails and prisons. New England Journal of Medicine. 2020;382(22):2075-7.
- Mhlanga-Gunda R, Rusakaniko S, Chinyuku AN, Pswarayi VF, Robinson CS, Kewley S, et al. “We sleep 10cm apart so there is no social distancing”: COVID-19 preparedness in a Zimbabwean prison complex. International Journal of Prisoner Health. 2023;19(2):157-80.
- Sequera Buzarquis VG. Epidemiological dynamics of Tuberculosis within the prison population and the community. 2024.


Comments are closed.