Rapid Assessment of HIV Service Delivery in Bidibidi Refugee Settlement, Yumbe District, March 2017
Author: Miriam Nakanwagi1, Denis Okethwangu1, Benon Kwesiga1, Alex R. Ario1; Affiliations: 1Uganda Public Health Fellowship Program – Field Epidemiology Track
Summary
Bidibidi Refugee Settlement in Yumbe District North Western Uganda was opened in August 2016, to resettle refugees fleeing the conflict in South Sudan. It currently shelters 272,000 refugees. We assessed HIV prevention and care services in the settlement, as part of the rapid health assessment, so as to identify gaps and make necessary recommendations. We collected data through household and health facility surveys, key informant interviews with health care providers, focus group discussions with the village health team members and local leaders, and review of secondary data from the UNHCR Health Information System (HIS) database for the camp. Of the 210 house- hold heads surveyed, 103 (49%) reported having had an HIV test and of these, 25 (12%) reported an HIV positive result. Almost all the facilities assessed conducted HIV counseling and testing but only 10% provided comprehensive HIV prevention and care services. The main challenges in HIV care provision cited were; lack of facility accreditation to offer HIV care, drug and test kits stock out and poor adherence to ART by the refugees. We recommend- ed HIV care outreaches to facilities in the settlement and later on accreditation of these facilities to offer HIV care services, training and mentoring of staff in health facilities in the settlement on HIV care, reporting and stock management and finally good ANC attendance should be an avenue for scale up of comprehensive PMTCT services .
Introduction
The political unrest in South Sudan and the resulting violence, food scarcity, and financial instability led to an influx of many South Sudanese refugees into Uganda from July 2016 to date. Bidibidi Refugee Settlement in Yumbe district was opened in early August 2016 to resettle them. It has a current refugee population of about 272,000 and no more refugees were being received in this settlement by March 2017 (1). In refugee settlements, information on HIV is limited because food, shelter, water and emergency health care take precedence (2). However, HIV spreads fastest in conditions of poverty, socio-economic powerlessness and social instability which are highly prevalent among refugees (3). Thus an understanding of the HIV prevention and care services in refugee settlements is crucial to limit further spread in this vulnerable population. In March 2017, we conducted an assessment of HIV care provision in the Settlement. Our aim was to establish the number of health facilities and scope of HIV services in the settlement, challenges encountered in the provision of HIV services and assess the refugee population’s knowledge of HIV prevention and transmission methods.
Figure 1: Map of Uganda showing Yumbe district, home to Bidibidi refugee settlement

Methods
We used the modified cluster-sampling technique and sampled 30 villages across the five zones. We then randomly selected 7 households within the sampled villages.
We thus administered questionnaires in a sample of 210 househeads. Of the sixteen facilities in the settlement, we randomly selected 10 health facilities and purposively selected three health facilities where refugees were commonly referred.
We conducted key informant interviews with health care providers and held focus group discussions with the village health team members and local leaders. We also had a key informant interview with a representative of Infectious Disease Institute (IDI) in Yumbe District.
Focus group discussions were limited to local leaders of the settlement and village health team members (VHTs).
We also reviewed refugee reports from Yumbe District Health Office, and HIS data from Real Medicine Foundation (RMF), the lead UNHCR implementing and coordinating partner for health.
Results
Of the 210 house-heads sampled, 99% were South Sudanese. The median age of the house-head was 31 years (IQR: 26-41), 117(56%) were female and 7(3.5%) were child-headed. From the household survey, 103(49%) of the respondents had tested for HIV and of these, 12 (12%) reported positive test. More than two thirds of the household heads had knowledge of the correct means of HIV transmission. About 70% of the household heads reported having knowledge of availability of HIV services provided at the facilities. The health facilities in the camp are at a level of a HC.
However, none of these is accredited to offer ART and apart from one facility, Bidibidi reception area HC III, the rest of the facilities sampled refer HIV positive patients to government facilities near the settlement. Bidibidi HCIII was the only facility that offered comprehensive HIV care services of those assessed. They run a daily clinic and see close to 20 patients per day but only 20% of these are refugees. They offer adult and paediatric ART, cotrimoxazole prophylaxis and anti- TB medicines and limited PMTCT services.
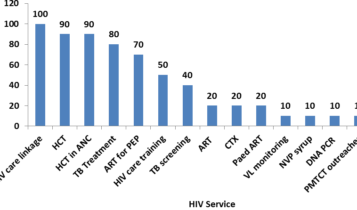
However, dried blood spot for HIV DNA PCR for infants and viral load (VL) monitoring are not done and patients are referred for this service to public facilities. In other settlement facilities, the commonly provided services are HIV counseling and testing (HCT), Post Exposure Prophylaxis (PEP) and linkage to HIV care services. Others such as ART, Cotrimoxazole (CTX) prophylaxis, Paediatric ART (Paed ART) and EID testing (DNA PCR) are offered in only 2 (20%) of the facilities that were sampled. Isoniazid preventive therapy (IPT) is not provided at any facility in the settlement. (See figure 2)
Figure 2: Availability of HIV services in Bidibidi refugee settlement, October to March 2017
Condom distribution is mainly by some facilities. Voluntary Medical Male Circumcision is not provided in all the facilities. There are no known hot spots of female sex workers in the settlement however there are truckers. There is no implementing partner supporting HIV care in the settlement although Infectious Diseases Institute (IDI) sometimes offers a supervisory role.
The challenges reported were: Stock out of test kits, NVP syrup and some ARVs in January and February, 2017, lack of training on HIV care, poor ART adherence due to an unstable population, under reporting of HIV indicators by facilities supported by agencies in the settlement, inadequate personnel, and parallel sample transportation making result follow- up complex.
Conclusions
The self-reported HIV prevalence in this assessment was much higher than the known HIV prevalence Yumbe and South Sudan (0.9% and 2.5% respectively).
However, HIV service provision in the camp is sub-optimal with very few facilities offering comprehensive HIV care services.
On a positive note, most of the refugee population was knowledgeable about the correct modes of HIV transmission as well as the HIV services.
Recommendations
Prior to accreditation of facilities in the settlement, there is need to carry out HIV care outreaches to support the facilities in the settlement provide HIV care and treatment. The Yumbe district health team (DHT) and RMF, the lead agency for health in the settlement should ensure that staffs in health facilities in the settlement are trained and routinely mentored in HIV care provision, stock monitoring, fore-casting and ordering to improve quality and access to these services.
Similarly, since all the facilities are Health Centre IIIs and thus conduct deliveries, RMF and the DHT can help them scale up comprehensive PMTCT services through provision of Nevirapine syrup and training on DBS sample collection to minimize attrition of infants through the PMTCT cascade.
Finally, UNHCR, Uganda’s Ministry of Health and Implementing Partners should work with Yumbe’s DHT and support the facilities in the settlement towards accreditation to offer comprehensive HIV service provision in order to increase treatment access in the settlement.
Acknowledgements
Yumbe district Health team , IDI, RMF CDC and the PHFP.
References
- United Nations High Commission for Refugees Conflict and HIV: A framework for risk assessment to prevent HIV in con- flict-affected settings in Africa: MockEmail, Nancy B; Duale, Sambe; Lisanne F Brown; Mathys, Ellen; O’Maonaigh, Heather C; Abul-Husn,Nina KL and Sterling Elliott, accessed on 3rd April 2017 at https://ete-online.biomedcentral.com/articles/10.1186/1742-7622-1-6.
- Vulnerability to HIV/AIDS Report of the Seminar on NGO Action, 28 -29 October 1996, London , accessed on 3rd April 2017 at http://reliefweb.int/sites/reliefweb.int/files/resources/31CCA21E053DD731C1256DC200372DAD-ukcon-ref- 96.pdf


Comments are closed.