Pre-exposure prophylaxis initiation and its associated factors among Adolescent Girls and Young Women in Uganda, 2017–2022
Authors: Susan Waako¹*, Innocent Ssemanda¹, Lilian Bulage¹٬², Benon Kwesiga¹٬²‚ Richard Migisha¹٬², Edirisa Junior Nsubuga¹٬⁴ Herbert Kadama⁵, Peter Mudiope⁵, Alex Riolexus Ario¹٬²; Institutional affiliations: ¹Uganda Public Health Fellowship Program; ²Uganda National Institute of Public Health, Kampala, Uganda; ⁴Uganda National Public Health Emergency Operations Centre, Ministry of Health Uganda; ⁵AIDS Control Program, Ministry of Health, Kampala, Uganda; Correspondence*: Tel: +256774835047, Email: swaako@uniph.go.ug
Summary
Background: Adolescent girls and young women (AGYW) aged 15-24 years are disproportionately affected by HIV, accounting for 28% of new HIV infections in Uganda. Oral pre-exposure prophylaxis (PrEP) is highly effective in reducing the risk of HIV acquisition for people at risk including AGYW. We describe oral PrEP initiation and associated factors among AGYW, Uganda, 2017−2022.
Methods: We analyzed nationwide PrEP data among AGYW reported through the PrEP tracker, an electronic Ministry of Health data management tool. We abstracted data on HIV testing, the PrEP cascade (screening, eligibility, and initiation), reasons for declining PrEP, and factors associated with PrEP initiation. We summarized the data for the various PrEP cascade indicators as frequencies and proportions. We used modified Poisson regression to determine factors associated with PrEP initiation.
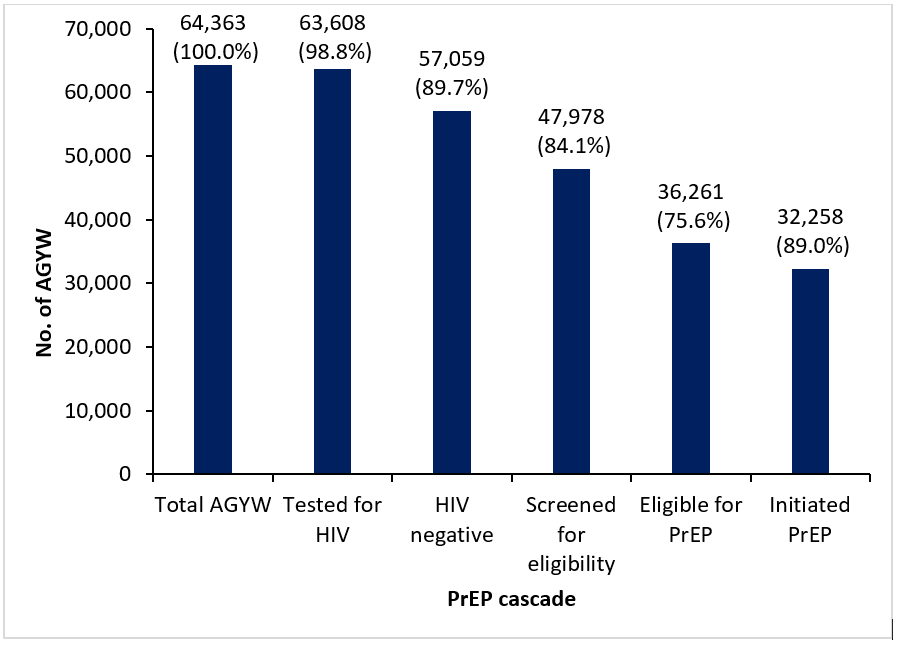
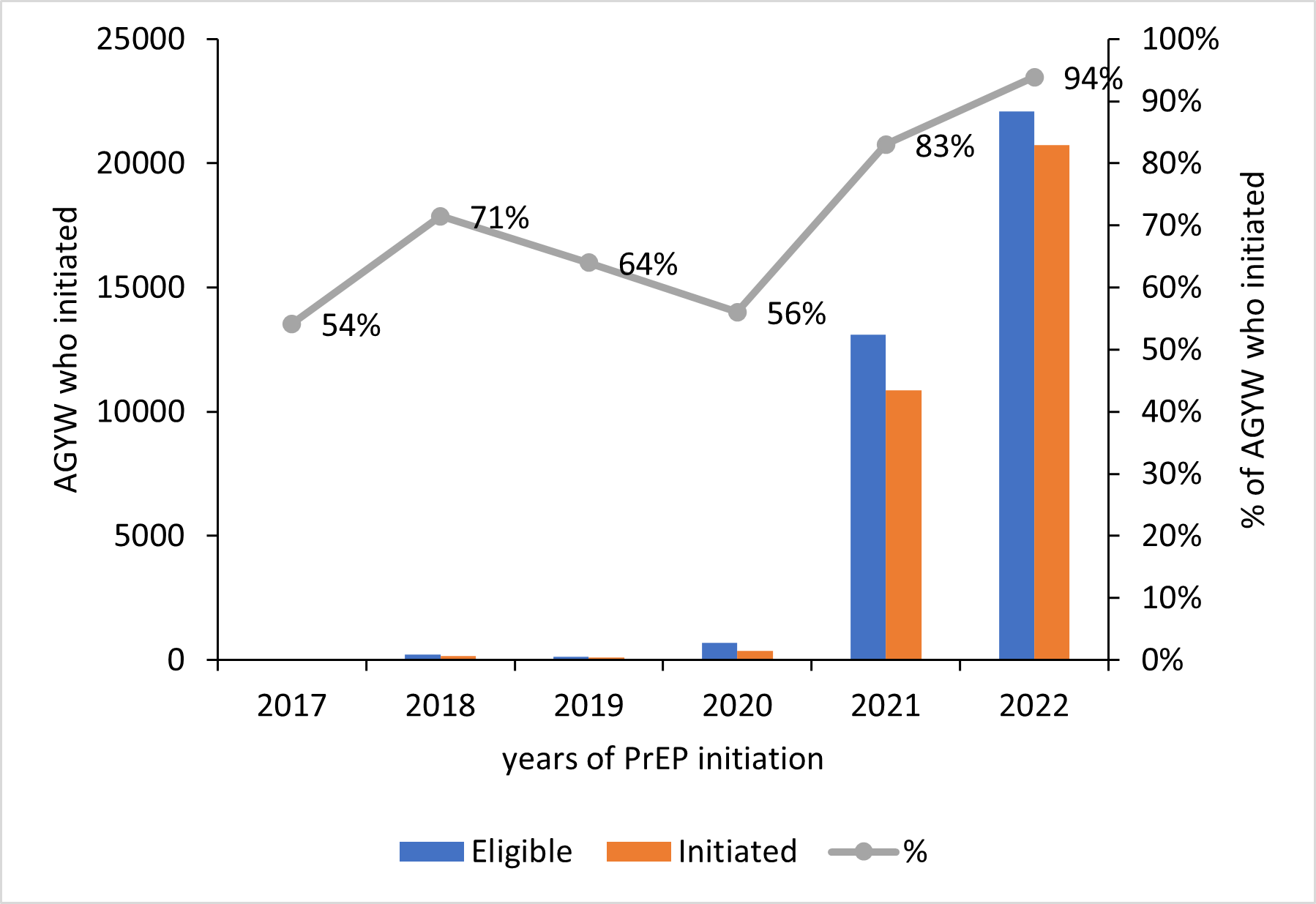
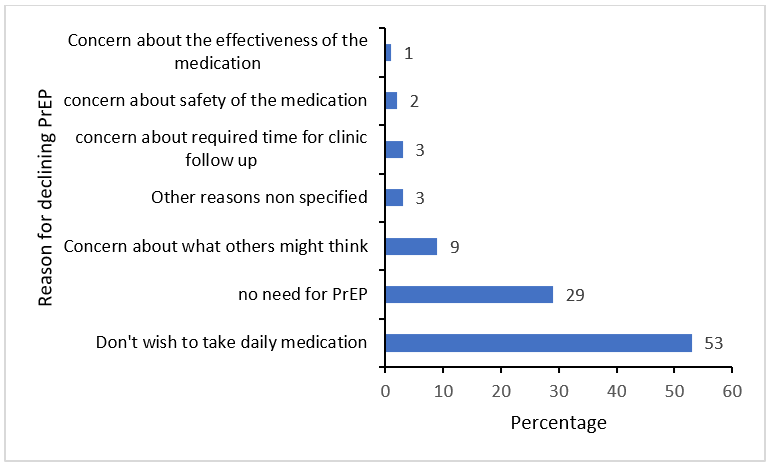
Results: A total of 64,363 observations of AGYW were obtained of which 63,608 (98.8%) AGYW were tested for HIV and 57,059 (89.7%) tested HIV-negative. Of the HIV-negative, 47,978 (84.1%) were screened for PrEP eligibility and 36,261 (75.6%) were eligible. Out of the eligible group, 32,258 (89.0%) initiated PrEP of which 19,379 (60.1%) were aged 20-24 years. The proportion who initiated PrEP increased from 54% in 2017 to 94% in 2022. More than half (53%) of the AGYW who never initiated PrEP attributed it to disliking daily medication. Being between 20-24 years (aPR:1.20; 95% CI: 1.02,1.29), having a casual sexual partner vs. single (aPR:1.20; 95% CI: 1.12-1.29), being tested through outreach (aOR:2.17 95% CI: 2.09-2.25) or at workplace (aPR:1.85; 95% CI: 1.68-2.03) vs. outpatient department were associated with increased likelihoods of initiating PrEP.
Conclusion: PrEP initiation was high among eligible AGYW. Dislike of daily medication was the main reason for declining PrEP, suggesting alternative PrEP regimens such as long acting cabotegravir and the dapivirine ring might result in greater PrEP initiation among eligible AGYW. In addition, reaching AGYW through outreaches or workplaces was associated with increased likelihood of PrEP initiation, suggesting strengthening of differentiated service delivery models that are adaptive to client needs and lessen access barriers.
Background
Despite progress towards ending HIV/AIDS as a public health threat in the last 20 years, there were still 1.5million new HIV infections globally in 2021 (1). The global HIV disease burden is disproportionately concentrated in Sub Saharan Africa (SSA); despite only containing one quarter of the world’s population(2). In 2017, SSA represented 65% of all new HIV infections (2).
Although Uganda has a generalized HIV epidemic, certain sub-populations, including Adolescent Girls and Young Women (AGYW) aged 15-24 years, continue to be at higher risk of HIV acquisition compared to the general population. In 2020, the prevalence of HIV among AGYW was 2.9% compared to 0.8% among adolescent boys and young men (ABYM)(3). Additionally, an estimated 54,000 new infections were recorded in Uganda during 2022, with approximately 37% occurring in young people aged 15-24 years of which nearly 75% happened to be AGYW (4, 5).
The high HIV risk in AGYW is attributed to a number of factors including but not limited to harmful cultural and gender norms, gender-based violence, poverty, high school drop- out rates, early marriages, and sexual intercourse with much older males (6). Furthermore, the COVID-19 pandemic is thought to have exacerbated the HIV risk for AGYW in Uganda due to the two years of school closure in the country, which happened to be the longest globally (7).
Changing the tide against HIV requires concerted efforts in large-scale implementation of effective HIV prevention interventions such as Pre- Exposure Prophylaxis (PrEP). Pre- Exposure Prophylaxis is an evidence-based HIV prevention intervention that reduces the risk of HIV acquisition by over 90% if used consistently and correctly (8). Oral PrEP is taken as a once daily combination pill of Tenofovir disoproxil fumarate and emtricitabine or Tenofovir disoproxil fumarate and Lamivudine (TDF + FTC or TDF + 3TC) as long as one is at substantial risk of HIV acquisition.
In Uganda, PrEP implementation started in July 2017 at six sites in four districts (9). By the end of 2022, PrEP was being provided at 587 sites in over 65 districts (10). At the time of rolling out PrEP implementation, the target population was men who have sex with men and female sex workers. Adolescent girls and young women were included to the target population for PrEP in the President’s Emergency Plan for AIDS Relief (PEPFAR) fiscal year October 2020–September 2021 (COP20).
Despite the scale-up of PrEP, initiation and continuation among AGYW has remained sub-optimal. According to unpublished PEPFAR Uganda Program data, 19,025 AGYW were initiated on PrEP in fiscal year 22 against a target of 70,196, representing only 27% of the target. Several barriers limit optimal PrEP use in AGYW including fear of side effects, intimate partner violence, low perceived risk, stigma associated with PrEP packaging, low family support, unfriendly and judgmental health workers, and inability to take daily pills among others (11).
According to studies conducted in Kenya, low and middle income countries, PrEP initiation among AGYW was dependent on a number of factors including but not limited to age, access to PrEP, knowledge about PrEP, one’s perception of their HIV risk, side effects, pill burden, support from peers, mode of delivery, doubts about PrEP efficacy, alcohol use, social support, social norms, fear of guardians reactions, and one’s attitude towards condoms use (12-15).
Although several periodic assessments have been done on PrEP initiation and continuation, little is known about PrEP initiation and its associated factors among AGYW (16, 17). Understanding the initiation of PrEP and its associated factors among AGYW is critical in guiding the design of tailored PrEP interventions and strategies. Additionally, it may help to high light regions that required inserted efforts to increase PrEP initiation among AGYW. We described PrEP initiation and its associated factors among AGYW in Uganda, 2017–2022.
Methods
Study setting
We considered PrEP data generated in the entire country. As of end of 2022, Uganda had approximately 6,937 health facilities, of which 587 provided PrEP (18, 19). According to the Uganda Bureau of Statistics Population Projection for 2022, the population of AGYW in Uganda was estimated at 4,808,700 (20).
Study design and data source
We analyzed PrEP data among high-risk AGYW aged 15-24 years reported through the PrEP tracker from 2017–2022. Adolescent girls and young women were added to the list of populations targeted for PrEP in Uganda in 2020. From 2017−2019, AGYW had access to PrEP but were not prioritized. The PrEP tracker is an electronic database that contains nationwide data for key and priority populations including high-risk AGYW. All health facilities that provide PrEP services are mandated to report data on a quarterly basis.
For AGYW to be initiated on PrEP, they must be eligible. Eligibility for PrEP includes one being HIV negative and is at substantial risk of acquiring HIV. Substantial risk of acquiring HIV includes the following: those with multiple sex partners of unknown HIV status, recurrent use of post exposure prophylaxis, and having at least one episode of a sexually transmitted infection monthly.
Pre-exposure prophylaxis data reported in the PrEP tracker include: total clients, total clients tested for HIV, total clients screened for PrEP eligibility and risk assessment, total clients eligible for PrEP, and total clients that Sero-converted.
Study variables, data collection, data management and analysis
Nationwide AGYW PrEP data was abstracted from the PrEP tracker. The data abstracted included: number of clients tested for HIV, total clients screened for PrEP eligibility, total clients eligible for PrEP and total clients initiated on PrEP, disaggregated by age (15-19, 20-24), from 2017–2022. We also obtained data on health facility and district/region.
The data was first downloaded in excel format and checked for completeness. The abstracted data was coded and imported into STATA SE version 14 for analysis. We summarized the data for the various PrEP cascade indicators (total AGYW, HIV testing, PrEP screening, PrEP eligibility, initiated on PrEP) as frequencies and proportions. Trends of PrEP initiation across the years were summarized as proportions and Mann-Kendal was used to determine significance of the trends. Choropleth maps were drawn using Quantum Geographic Information System (QGIS) to show the distribution of AGYW initiated on PrEP for the years 2017–2022.
We used modified poison regression to identify factors associated with PrEP initiation.
Ethical considerations
Since our study used routine surveillance data reported by health facilities in the PrEP tracker, we sort for permission from Monitoring and Evaluation Technical Support (METS). US Centres for Disease Control and Prevention (CDC) provided the non-research determination (NRD) for non-human subjects. In agreement with the International Guidelines for Ethical Review of Epidemiological Studies by the Council for International Organizations of Medical Sciences (1991) and the Office of the Associate Director for Science, US CDC/Uganda, it was determined that this activity was not human subject research and that its primary intent was public health practice or disease control activity (specifically, epidemic or endemic disease control activity). This activity was reviewed by the US CDC and was conducted consistent with applicable federal law and CDC policy. §§See, e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq. All experimental protocols were approved by the US CDC human subjects review board (The National Institute for Occupational Safety and Health Institutional Review Board) and the Uganda Ministry of Health and were performed in accordance with the Declaration of Helsinki
Results
pre-exposure prophylaxis cascade of adolescent girls and young women, Uganda, 2017–2022
Of the 64,363 AGYW aged 15-24, 63,608 (98.8%) were tested for HIV, of which 57,059 (89.7%) tested HIV negative. Of those that tested HIV-negative, 47,978 (84.1%) were screened for PrEP eligibility, of which 36,261 (75.6%) were eligible for PrEP. Of those eligible, 32,258 (89.0%) were initiated on PrEP over the six-year period (Figure 1).
Demographic characteristics of adolescent girls and young women initiated on pre-exposure prophylaxis in Uganda, 2017–2022
A total of 64,363 records of AGYW were abstracted and 32,258 initiated PrEP. Of those that initiated PrEP, 60% were aged 20-24 years, nearly three quarters (74.5%) were single, nearly half of them (49.8%) had primary education and over 80% of them were reached through outreach (Table 1).
Table 1: Baseline characteristics of adolescent girls and young women initiated on pre-exposure prophylaxis in Uganda, 2017–2022
| Characteristics | Frequency (n=32,258) | Percent |
| Age group | ||
| 15-19 | 12,879 | 40.0 |
| 20-24 | 19,379 | 60.0 |
| Marital status* | ||
| Single | 19,191 | 74.5 |
| Married | 5,178 | 20.1 |
| Divorced | 975 | 3.8 |
| Regular partner | 43 | 0.2 |
| Causal | 340 | 1.3 |
| Widowed | 23 | 0.1 |
| Educational level† | ||
| No formal education | 3,013 | 14.9 |
| Primary | 10,093 | 49.8 |
| Secondary | 6,766 | 33.4 |
| Tertiary | 391 | 1.4 |
| Nationality‡ | ||
| National | 22,883 | 99.8 |
| Foreigner | 3 | 0.01 |
| Refugee | 44 | 0.2 |
| Point of entry§ | ||
| OPD | 3,329 | 14.6 |
| ACASI | 28 | 0.1 |
| ART clinic | 76 | 0.3 |
| Homebased HTC | 39 | 0.2 |
| MCH | 383 | 1.7 |
| Outreach | 18,277 | 80.1 |
| PMTCT | 314 | 1.1 |
| Workplace | 323 | 1.4 |
| Others | 40 | 0.2 |
| Region¶ | ||
| Acholi | 2,045 | 6.3 |
| Ankole | 1,092 | 3.4 |
| Bugisu | 662 | 2.1 |
| Bukedi | 425 | 1.3 |
| Bunyoro | 1,369 | 4.3 |
| Busoga | 858 | 2.7 |
| Kampala | 7,517 | 23.3 |
| Karamoja | 0 | 0.0 |
| Kigezi | 299 | 0.9 |
| Lango | 5,398 | 16.8 |
| North Central | 5,302 | 16.5 |
| South Central | 6,204 | 19.25 |
| Teso | 28 | 0.1 |
| Tooro | 901 | 2.8 |
| West Nile | 133 | 0.4 |
*representing an n of 25,750, †representing an n=20,263, ‡ representing an n=22,930, § representing n=22,809, ¶representing n =32,233
Trend of adolescent girls and young women initiated on pre-exposure prophylaxis over the years in Uganda, 2017–2022
Overall, the proportion of AGYW who initiated PrEP across the years increased from 54% in 2017 to 94% in 2022 but the increase was not significant (p=0.13) (Figure 2).
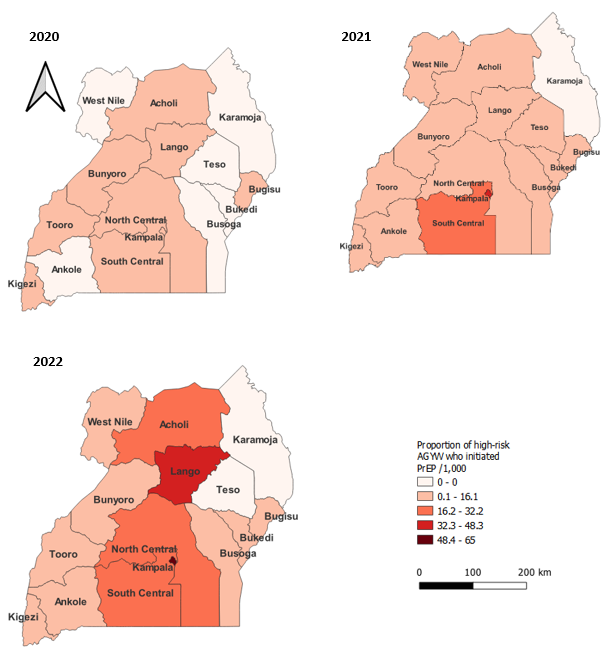
Distribution of proportion of adolescent girls and young women initiated on pre-exposure prophylaxis per region, Uganda, 2020–2022
Across the years, the proportion of AGYW initiated on PrEP per region increased as shown (Figure 4). In 2022, Kampala region had the highest proportion of high-risk AGYW initiated on PrEP (Figure 3).
Factors associated with pre-exposure prophylaxis Initiation among adolescent girls and young women, Uganda, 2017–2022
At bivariate analysis, age group, marital status, educational level, point of entry and region were associated with PrEP initiation (Table 3).
At multi-variate analysis, being aged 20-24 (aPR:1.04; 95% CI: 1.02-1.29), having a casual partner (aPR=1.20; 95% CI: 1.12, 1.29), being reached through outreach (aPR:2.17; 95% CI: 2.09-2.25) and work place (aPR:1.85; 95% CI: 1.68-2.03) were associated with an increased likelihood of PrEP initiation. On the other hand, having secondary education (aPR:0.92; 95% CI: 0.90-0.95), tertiary education (aPR:0.73; 95% CI: 0.67-0.79), accessing services at PMTCT (aPR:0.57 95% CI: 0.48-0.68) and being in a region other than Bugisu and Teso were associated with a reduced likelihood of initiating PrEP (Table 2).
Table 2: Factors associated with pre-exposure prophylaxis initiation among adolescent girls and young women, Uganda, 2017–2022
| Characteristic | PrEP
initiation |
PrEP initiation | Unadjusted PR (95% CI) | Adjusted PR (95% CI) |
| Yes (%) | No (%) | |||
| Age group | ||||
| 15-19 | 12,879 (40.0) | 13,263 (41.3) | 1 | 1 |
| 20-24 | 19,379 (60.1) | 18,842 (58.7) | 1.56 (1.03, 1.77) | 1.04 (1.02, 1.06) |
| Marital status | ||||
| Single | 19,191(74.5) | 18,093 (71.6) | 1 | 1 |
| Married | 5,178 (27.0) | 6,048 (23.9) | 0.97 (0.95, 0.99) | 0.99 (0.68, 1.10) |
| Divorced | 975 (3.8) | 757 (3.0) | 1.17 (1.13, 1.21) | 1.00 (0.96, 1.05) |
| Regular partner | 43 (0.2) | 158 (0.6) | 0.51 (0.40, 0.65) | 0.75 (0.61, 1.05) |
| Causal sexual partner | 340 (1.3) | 192 (0.8) | 1.23 (1.17, 1.30) | 1.20 (1.12, 1.29) |
| Widowed | 23 (0.1) | 20 (0.1) | 2.10 (0.85, 1.36) | 1.10 (0.86, 1.40) |
| Educational level | ||||
| No formal education | 3,013 (14.9) | 2,863 (16.6) | 1 | 1 |
| Primary | 10,093 (49.8) | 7,036 (40.8) | 1.14 (1.12, 1.17) | 0.98 (0.96, 1.01) |
| Secondary | 6,766 (33.4) | 6,641 (38.5) | 1.32 (1.00, 1.06) | 0.92 (0.90, 0.95) |
| Tertiary | 391 (1.9) | 710 (4.1) | 0.91 (0.85, 0.98) | 0.73 (0.67, 0.79) |
| Region | ||||
| Acholi | 2,045 (6.3) | 206 (0.7) | 1 | 1 |
| Ankole | 1,092 (3.4) | 2,449 (8.7) | 0.37 (0.36, 0.39) | 0.52 (0.96, 1.01) |
| Bugisu | 662 (2.1) | 83 (0.3) | 0.97 (0.94, 0.99) | 0.97 (0.93, 1.01) |
| Bukedi | 425 (1.3) | 427 (1.5) | 0.61 (0.57, 0.65) | 0.55 (0.50, 0.60) |
| Bunyoro | 1,369 (4.2) | 903 (3.2) | 0.78 (0.76, 0.81) | 0.72 (0.69, 0.75) |
| Busoga | 858 (2.7) | 1,206 (4.3) | 0.59 (0.56, 0.62) | 0.52 (0.46, 0.57) |
| Kampala | 7,517 (23.3) | 7,771 (27.6) | 0.73 (0.72, 0.74) | 0.67 (0.65, 0.68) |
| Kigezi | 299 (0.9) | 260 (0.9) | 0.61 (0.57, 0.66) | 0.59 (0.49, 0.72) |
| Lango | 5,398 (16.7) | 240 (0.9) | 1.04 (1.03, 1.05) | 0.94 (0.92, 0.96) |
| North Central | 5,302 (16.4) | 4,645 (16.5) | 0.73 (0.72, 0.74) | 0.81 (0.78, 0.84) |
| South Central | 6,204 (19.2) | 4,234 (15.1) | 0.75 (0.74, 0.76) | 0.72 (0.70, 0.74) |
| Teso | 28 (0.1) | 6 (0.02) | 0.92 (0.79, 1.06) | 0.61 (0.83, 1.09) |
| Tooro | 901 (2.8) | 3,058 (10.9) | 0.35 (0.34, 0.37) | 0.30 (0.28, 0.34) |
| West Nile | 133 (0.4) | 2,623 (9.3) | 0.07 (0.06, 0.08) | 0.06 (0.05, 0.08) |
| Point of entry | ||||
| OPD | 3,329 (14.6) | 11,009 (44.5) | 1 | 1 |
| ACASI | 28 (0.1) | 41 (0.2) | 1.36 (1.05, 1.77) | 1.38 (0.97, 1.96) |
| ART clinic | 76 (0.3) | 382 (1.5) | 0.82 (0.68, 0.99) | 0.61 (0.80, 1.38) |
| Home based HTC | 39 (0.2) | 225 (0.9) | 0.42 (0.31, 0.56) | 1.15 (0.71, 1.86) |
| MCH | 383 (1.7) | 1,307 (5.3) | 0.88 (0.81, 0.96) | 1.02 (0.91, 1.01) |
| Outreach | 18,277 (80.1) | 10,089 (40.8) | 1.92 (1.86, 0.96) | 2.17 (2.09, 2.25) |
| PMTCT | 314 (1.4) | 1,414 (5.7) | 0.70 (0.63, 0.77) | 0.57 (0.48, 0.68) |
| Workplace | 323 (1.4) | 232 (0.9) | 1.94 (1.83, 2.07) | 1.85 (1.68, 2.03) |
| Others | 40 (0.2) | 46 (0.2) | 1.65 (1.36, 2.00) | 1.59 (1.20, 2.10) |
*aPR=adjusted prevalence ratio, uPR: unadjusted prevalence ratio, ACASI: Audio-computer assisted self-interview, PMTCT: Prevention of Mother to Child Transmission of HIV, MCH: Maternal and Child Health.
Reasons for declining pre-exposure prophylaxis among adolescent girls and young women, Uganda, 2017–2022
Of the 4,003 AGYW who didn’t initiate PrEP, 656 (14.1%) reported reasons for declining PrEP. The main two reasons for declining PrEP were inability to take daily medication (53%) and no need for PrEP (29%) (Figure 4).
Discussion
In this study, we have described PrEP initiation and its associated factors among AGYW in Uganda from 2017–2022. Over the years PrEP initiation and the regions offering PrEP increased. More than half of the AGYW initiated on PrEP were aged 20-24 years. In addition, being aged 20-24 years, being reached through outreaches, and workplaces were associated with an increased likelihood of PrEP initiation. On the other hand, being reached through PMTCT, having secondary or tertiary education, and being in a region other than Bugisu or Teso was associated with a reduced likelihood of initiating PrEP. A few of the eligible AGYW declined PrEP.
HIV testing is a critical entry step into HIV prevention and treatment programs. HIV testing for AGYW was very high. This could be attributed to a favorable ministry of health policy that lowered consent age for HIV testing from 18 to 12 years(21). In addition, the increasing PEPFAR HIV testing targets over the years contributes to improved screening and testing(22).
Majority of the HIV negative AGYW were screened for PrEP eligibility. Although this may be high, it also presents missed opportunities in not screening a significant number of AGYW. The non-screened AGYW had been found eligible for HIV testing which implies that they had at least one factor putting them at risk of HIV acquisition. The proportion of AGYW eligible for PrEP was even lower. This could be attributed to the rigorous PrEP eligibility screening process which may screen out some clients. Overall, PrEP initiation was high. This could be attributed to good health education, counselling, and strong peer support systems. Similar findings were noted in a study conducted in both South Africa and Kenya where AGYW reported that receiving both clear and comprehensive information on PrEP enriched their knowledge on the same thus interesting them to initiate PrEP (23). In addition, AGYW in Kenya reported peer support helped to normalize PrEP use and reduced stigma as they influenced their understanding of PrEP and its initiation (13).
Over the years PrEP initiation increased. This could be attributed to improved health worker capacity to offer PrEP, increased number of sites offering PrEP, and the increasing PEPFAR PrEP targets year after year. The increased targets usually come with increased resources which translates into improved performance(22). The deep in 2019 and 2020 could be attributed to travel restrictions implemented by government to curtail the spread of COVID-19 and this could have been before the program adaptations to ensure un-interrupted service provision took effect(24).
The regions offering PrEP increased. Kampala has had the greatest number of PrEP initiations compared to all the other regions. This could be attributed to the fact that Kampala started implementing the PrEP program earlier than the other regions(25). This programmatic experience puts Kampala ahead of the rest. Karamoja region has not had any PrEP initiations. This is because, annual Spectrum Estimates have shown that Karamoja is a low HIV incidence region and therefore has never received PEPFAR PrEP targets.
More than half of the AGYW initiated on PrEP were aged 20-24 years. Similarly, being aged 20-24 years was associated with an increased likelihood of PrEP initiation. This could be due AGYW aged 20-24 being more independent and knowledgeable about PrEP (27). In addition, this could be attributed to the fact that those aged 15-19 years are not expected to be sexually active by society thus fear to initiate PrEP. This finding is similar to another study by Kayesu, Ivy, et al. where participants aged 15-19 years reported lack of interest in PrEP due to fearing being judged by people in their communities to be sexually active (15). In addition, similar findings were reported in a study conducted among PEPFAR supported countries where 64% of the AGYW who initiated PrEP were aged 20-24 years (28).
Being reached through outreaches and work places were associated with an increased likelihood of PrEP initiation. This may be attributed to the fact that taking PrEP to work places and outreaches makes access easier as one doesn’t require transport money. Work places present an opportunity of safe spaces for PrEP initiation since the AGYW are not in fear of meeting with relatives and community members unlike while at health facilities. Similar finding were reported that use of safe places protect AGYW from shying away from PrEP due to fear of meeting with relatives while at the health facility(23). In addition, availing PrEP at work places may come-in handy as a solution to the inconvenient schedules in securing PrEP for those in formal employment. In Malawi, participants reported that their interest in initiating PrEP was dependent on the ease of accessing it (29). In another study conducted in Kampala, it was reported that having to travel to distant areas and living far from health facilities hindered some participants from picking up their PrEP re-fills and it can’t be any different for initiation (15). Similarly, in a study done among female sex workers, 91.6% preferred having PrEP services provided through outreaches to health facilities(30).
Provision of PrEP within PMTCT was associated with a reduced likelihood of initiation. This could be attributed to fear (stigma) of being seen with the PrEP medication by relatives and friends. On the contrary, visiting PMTCT comes with continuous interaction with peers who are knowledgeable on PrEP. Some AGYW in Kenya noted that conversations held with knowledgeable and experienced peers influenced their understanding of PrEP resulting in initiation, not forgetting that peers are known for having greater influence over adolescents’ decisions (13).
Of the eligible AGYW, about a tenth declined PrEP. Of these, we found out that only 14% had reasons for declining PrEP initiation documented. More than half of those with reasons documented, reported that they would not wish to take daily medication and nearly a third reported that they didn’t need PrEP. Similar findings were reported in studies in Kenya where AGYW reported that the need to take a daily pill was a major inhibitor to PrEP initiation (12, 13). This finding builds a case for rolling out and scaling out newer long acting and discrete PrEP products like the PrEP Ring and long acting cabotegravir.
Study limitations
Some variables (continuity on PrEP and sero-conversion) had missing data and as a result, were dropped. In turn we were unable to determine how the optimal PrEP initiation translates into continuity in the program. Given the use of secondary data, we were not able to get detailed a understanding of the reasons for declining PrEP among AGYW.
Conclusion
PrEP initiation was high among eligible AGYW. Dislike of daily medication was the main reason for declining PrEP. Kampala had the greatest number of PrEP initiations compared to all the other regions. Being aged 20-24 years, having a casual partner, being reached through outreaches, and workplaces were associated with an increased likelihood of PrEP initiation.
Recommendations
Ministry of Health should expedite the introduction and scale up of alternative PrEP regimes such as long acting cabotegravir and the dapivirine ring as these might result in greater PrEP initiation among eligible AGYW. In addition, there is need to strengthen differentiated service delivery models that are adaptive to client needs and lessen access barriers. Ministry of Health needs to support heath facilities to develop strategies to increase PrEP screening and initiation among AGYW within the departments offering PrEP to reduce on the missed opportunities since majority of the screened AGYW were from the outreaches.
Conflict of interest
The authors declare that they have no conflict of interest.
Authors’ contributions
SW took the lead in conceptualizing the study idea, data analysis, writing, and editing the bulletin. IS, LB, BK, RM, EJN, HK, PM, and ARA were involved in the conceptualization of the study idea and the writing, editing, and reviewing of the bulletin. All authors read and approved the final bulletin.
Acknowledgements
The authors appreciate the Monitoring and Evaluation Technical Support, Makerere University School of Public Health for providing access to PrEP data that was used for this analysis.
Copyright and Licensing
All material in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
1.UNAIDS. THE PATH THAT ENDS AIDS, 2023 UNAIDS Global AIDS Update. https://unaidsorg/en. 2023.
2.Dwyer-Lindgren L, Cork MA, Sligar A, Steuben KM, Wilson KF, Provost NR, et al. Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature. 2019;570(7760):189-93.
3.UPHIA. UPHIA-Summary-Sheet-2020.pdf (columbia.edu) 2020.
4.UNAIDS. 2021 Factsheet – Facts on HIV and AIDS in Uganda 2021 (Based on Data ending 31st December 2020). https://uacgoug/media/attachments/2021/09/13/final-2021-hiv-aids-factsheetpdf. 2021.
5.Commission UA. Factsheet- Facts on HIV and AIDS in Uganda 2021 (Based on Date ending 31st December 2020). 2021.
6.UNAIDS. Women and HIV — A spotlight on adolescent girls and young women (unaids.org). 2019.
7.Mwine P, Kwesiga B, Migisha R, Cheptoris J, Kadobera D, Bulage L, et al. Sexual Gender-Based Violence among Adolescent Girls and Young Women 10-24 Years during COVID-19 Pandemic, Bukedi Region, Eastern Uganda.
8.McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet. 2016;387(10013):53-60.
9.Muwonge TR, Nsubuga R, Brown C, Nakyanzi A, Bagaya M, Bambia F, et al. Knowledge and barriers of PrEP delivery among diverse groups of potential PrEP users in Central Uganda. PloS one. 2020;15(10):e0241399.
10.Health Mo. Technical Guidance on Pre-Exposure Prophylaxis (PrEP) for Persons at Substantial Risk of HIV Infection in Uganda | MOH Knowledge Management Portal (health.go.ug). 2022.
11.Irungu E, Khoza N, Velloza J. Multi-level interventions to promote oral pre-exposure prophylaxis use among adolescent girls and young women: a review of recent research. Current HIV/AIDS Reports. 2021:1-10.
12.Sila J, Larsen AM, Kinuthia J, Owiti G, Abuna F, Kohler PK, et al. High awareness, yet low uptake, of pre-exposure prophylaxis among adolescent girls and young women within family planning clinics in Kenya. AIDS patient care and STDs. 2020;34(8):336-43.
13.Rogers ZH. “You are your own driver”: Factors Influencing the Decision to Initiate PrEP Among Adolescent Girls and Young Women within Routine Maternal Child Health and Family Planning Clinics in Western Kenya 2020.
14.Ekwunife OI, Ejie IL, Okelu V, Mita C, Durosinmi-Eti O, Powell A, et al. Interventions to increase the uptake and continuation of pre-exposure prophylaxis (PrEP) by adolescent girls and young women at high risk of HIV in low-income and middle-income countries: a scoping review. BMJ Global Health. 2022;7(12):e009474.
15.Kayesu I, Mayanja Y, Nakirijja C, Machira YW, Price M, Seeley J, et al. Uptake of and adherence to oral pre-exposure prophylaxis among adolescent girls and young women at high risk of HIV-infection in Kampala, Uganda: A qualitative study of experiences, facilitators and barriers. BMC women’s health. 2022;22(1):1-14.
16.Kayesu I, Mayanja Y, Nakirijja C, Machira YW, Price M, Seeley J, et al. Uptake of and adherence to oral pre-exposure prophylaxis among adolescent girls and young women at high risk of HIV-infection in Kampala, Uganda: A qualitative study of experiences, facilitators and barriers. 2022;22(1):1-14.
17.Mayanja Y, Kamacooko O, Lunkuse JF, Muturi‐Kioi V, Buzibye A, Omali D, et al. Oral pre‐exposure prophylaxis preference, uptake, adherence and continuation among adolescent girls and young women in Kampala, Uganda: a prospective cohort study. 2022;25(5):e25909.
18.Tracker P. PrEP Tracker. 2022.
19.Health Mo. Hospitals. https://wwwhealthgoug/hospitals/. 2023.
20.PEPFAR. Uganda Country Operational Plan (COP) 2022 Strategic Direction Summary. https://wwwprepwatchorg/wp-content/uploads/2022/11/Uganda-COP-2022pdf. 2022.
21.Health Mo. National HIV testing services policy and implementation guidelines. Ministry of Health of Uganda. 2016.
22.Jones A, Honermann B, Lankiewicz E, Sherwood J, Millett G. Current allocations and target apportionment for HIV testing and treatment services for marginalized populations: characterizing PEPFAR investment and strategy. Journal of the International AIDS Society. 2021;24:e25753.
23.Jackson-Gibson M, Ezema AU, Orero W, Were I, Ohiomoba RO, Mbullo PO, et al. Facilitators and barriers to HIV pre-exposure prophylaxis (PrEP) uptake through a community-based intervention strategy among adolescent girls and young women in Seme Sub-County, Kisumu, Kenya. BMC public health. 2021;21:1-13.
24.Sarki AM, Ezeh A, Stranges S. Uganda as a role model for pandemic containment in Africa. American Public Health Association; 2020. p. 1800-2.
25.Bosco Jr MJ, Tusiime JB, Mayega RW, Nalubega S. Uptake of oral-based HIV self-testing among Key Populations taking HIV pre-exposure prophylaxis in central Uganda. 2020.
26.Kamya C, Namugaya F, Opio C, Katamba P, Carnahan E, Katahoire A, et al. Coverage and Drivers to Reaching the Last Child With Vaccination in Urban Settings: A Mixed-Methods Study in Kampala, Uganda. Global Health: Science and Practice. 2022;10(4).
27.Lanham M, Ridgeway K, Mireku M, Nhamo D, Pillay D, Murire M, et al. Health care providers’ attitudes toward and experiences delivering oral PrEP to adolescent girls and young women in Kenya, South Africa, and Zimbabwe. BMC Health Services Research. 2021;21:1-12.
28.Patel P, Sato K, Bhandari N, Kanagasabai U, Schelar E, Cooney C, et al. From policy to practice: uptake of pre-exposure prophylaxis among adolescent girls and young women in United States President’s Emergency Plan for AIDS Relief-supported countries, 2017–2020. AIDS. 2022;36(1):S15-S26.
29.Maseko B, Hill LM, Phanga T, Bhushan N, Vansia D, Kamtsendero L, et al. Perceptions of and interest in HIV pre-exposure prophylaxis use among adolescent girls and young women in Lilongwe, Malawi. PLoS One. 2020;15(1):e0226062.
30.Martin VO, Tesha NA, Sunguya BF. Uptake of Oral HIV Pre-Exposure Prophylaxis (PrEP) and Associated Factors among Female Sex Workers in Tanga, Tanzania. Viruses. 2023;15(10):2125.


Comments are closed.