Methanol poisoning caused by adulteration of alcohol at production stage in a factory in North Western Uganda, August 2022
Authors: Robert Zavuga*1, Thomas Kiggundu1, Mackline Ninsiima1, Peter Chris Kawungezi1, Lawrence Oonyu1, Brian Agaba1, Richard Migisha1, Doreen Gonahasa1, Daniel Kadobera1, Benon Kwesiga1, Lilian Bulage1, Freda Loy Aceng2, Joshua Kayiwa2, Peter Edward Okello1, Issa Makumbi2, Alex Riolexus Ario1,2 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda, National Institute of Public Health, Kampala, Uganda, 2Ministry of Health, Kampala, Uganda *Correspondence: Email: rzavuga@musph.ac.ug, Tel:+256772655723
Summary Background: Methanol is a toxic industrial solvent which, when ingested can cause vision loss, severe illness, and death. In August 2022, the Ugandan Ministry of Health was notified of a cluster of sudden deaths in Arua City and Madi-Okollo District in persons who had consumed gin (Gin X) produced from a local manufacturer (Manufacturer A). We investigated the outbreak to determine the scope of the problem, identify the risk factors for the sudden deaths, and recommend control and prevention measures. Methods: We defined a suspected case as acute onset of blurred vision with abdominal pain, general body weakness, headache, or profuse sweating in a resident of Arua City or Madi-Okollo districts from 16–26 August 2022. A retrospective cohort study was carried out among the cases to identify risk factors for death. In collaboration with Uganda Police Force and the Uganda National Bureau of Standards, we collected samples of Gin X from manufacturer A for methanol toxicology analysis at the Government Analytical Laboratory in Kampala. Autopsies were carried out on all deceased case-patients. Results: We identified 48 cases (47 males and 1 female); 18 (38%) died. The median age of cases was 32 years (IQR 26-46). Compared with cases who consumed one 200ml bottle or less of Gin X, the risk of dying was 4 times (RR=4.1, 95% CI: 0.49-34, p=0.19) higher (non-significant) among those who drank 2 bottles, and 10 times (RR=10.7, 95% CI: 1.5-75, p=0.02) higher among those who drank ≥3 bottles. The mean methanol content among the five samples which were collected from manufacturer A was 594,424 mg/L (range 259,263- 809,193 mg/L), higher than the maximum recommended limit of 50mg/L. Eight autopsies all showed liver inflammation oedema, gastrointestinal bleeding, and pulmonary oedema which is consistent with methanol poisoning. We found out that manufacturer A was not licensed to produce gins but rather fruit wines only. Conclusion: This outbreak was caused by consumption of Gin X manufactured by manufacturer A which was adulterated with methanol at the production stage. We recommend strict enforcement of the laws that govern alcohol production and distribution.
Background
Methanol is a toxic industrial organic solvent which is used as a cleansing solution, pesticide, and an alternative bio-fuel [1, 2]. It is also sometimes mixed with ethanol in alcoholic beverages either by mistake or intentionally as a cheap substitute for ethanol. Methanol poisoning is an important public health problem because of its severe consequences. The maximum safe limit of methanol in drinking alcohol is 50mg/L [3]. Once ingested, it undergoes enzymatic oxidation and is converted to highly toxic formic acid which can lead to metabolic acidosis, neurotoxicity, optic nerve damage and death [4]. Symptoms usually appear 12-24 hours after ingestion but can be delayed if ethanol is ingested simultaneously [5].
Unregulated and unrecorded alcohol productions are responsible for most methanol poisoning outbreaks due to adulteration of alcoholic beverages. Low income countries are disproportionately affected due to poor capacity to regulate and monitor the sale of the unrecorded alcoholic beverages [6]. Delays in notification of the health system to respond to outbreaks, poor health seeking behavior of the victims, and unavailability of adequate resources to treat methanol toxicity can lead to severity of symptoms and high case fatality rates [7].
On 18th August 2022, the Uganda Ministry of Health (MoH) through the Public Health Emergency Operations Centre (PHEOC) received a report about a cluster of deaths in Arua City. This incident reportedly occurred after multiple persons consumed alcohol which was packed in plastic bottles from a local alcohol manufacturer. The victims presented with headache, backache, restlessness, difficulty in breathing, and loss of consciousness before they died. The same incident was also reported in the neighboring district of Madi-Okollo after consumption of the same beverage. We investigated the outbreak to determine the scope of the problem, cause of sudden deaths, identify the risk factors for the sudden deaths in these clusters, and recommend control and prevention measures.
Methods
Outbreak area
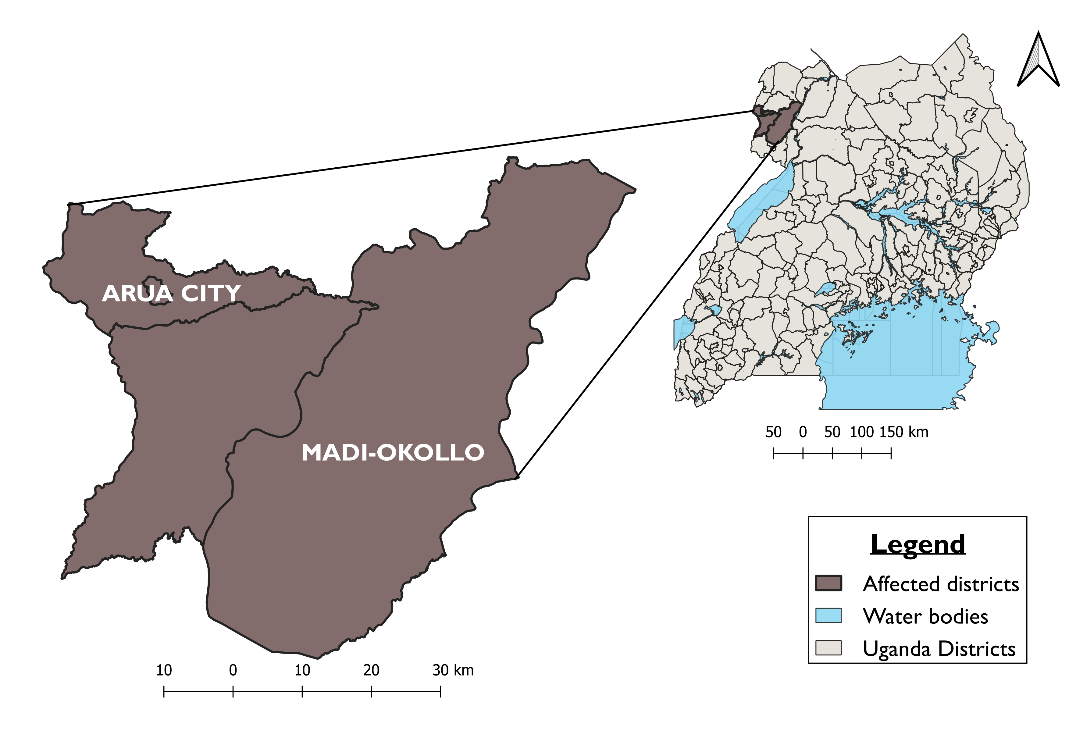
The investigation was conducted in Arua City and Madi-Okollo District which are both located in North Western Uganda (Figure 1). This region is bordered by Democratic Republic of Congo in the west and South Sudan in the North. It is served by Arua Regional Referral Hospital (ARRH), which is the main referral treatment facility.
Case definition and finding
We defined a suspected case as; onset of blurred vision or abdominal pain with any of the following: general body weakness, headache, dizziness, profuse sweating, or loss of vision in a resident of Arua City or Madi-Okollo District from 16 to 26 August 2022.
We reviewed medical records from ARRH and other health facilities where the cases sought care from for the month of August 2022. With the help of community health workers who are also referred to as village health team members we conducted community case-finding in Arua City and Madi-Okollo District in the affected sub counties. We interviewed survivors and next-of-kin of the deceased to develop a line list of the suspected cases. We also conducted key informant interviews with the local community leaders to investigate the occurrence of similar cases in the communities.
Descriptive epidemiology
We analyzed the line list data to characterize case-patients by their clinical presentations. We used attack rates to describe the distribution of cases by age and place of residence. The attack rates were calculated using population data from the Uganda National Bureau of Statistics (UBOS) population projections for Arua City and Madi-Okollo District.
Laboratory and post-mortem investigations
In collaboration with the Uganda Police Force and the Uganda National Bureau of Standards (UNBS) – the body responsible for licensing and certification of products in Uganda, eight samples of the suspected gin were collected and submitted to the Government Analytical Laboratory (GAL) in Kampala for toxicological analysis. Additionally, police carried out eight autopsies on the deceased from ARRH.
Case management
We identified data on how the survivors and deceased were managed through visiting the heath facilities where they sought treatment, reviewing their medical records, and the type of treatment they received.
Trace-back investigations and environmental assessment
We interviewed survivors, next of kin of the deceased, the owners of the factory, owners of bars and shops that were selling alcohol to identify the source of the implicated gin X, and the point at which and why it might have been adulterated.
Hypothesis generation interviews
We used a structured questionnaire to interview survivors and next of kin of the deceased on the case-patients’ alcohol exposures two days prior to their onset of symptoms.
Retrospective cohort study
The initial investigation showed that all cases had consumed gin X from 16 to 26 August 2022, suggesting that gin X was implicated. We then conducted a retrospective cohort study and enrolled all cases in the two most affected sub-counties in Arua City and Madi-Okollo District to determine the risk of death after consuming gin X. We used a structured questionnaire to interview all cases. The questionnaire inquired whether they drunk gin X between 16 to 26 August 2022, the exposure dates, place where they drunk gin X from, and the quantity of gin X taken.
Ethical considerations
This outbreak investigation was in response to a public health emergency and was therefore determined to be non-research. The MoH gave a directive to investigate this outbreak and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and that its primary intent was for public health practice or disease control.
The authors sought permission to conduct the investigation from District Health authorities of Arua City and Madi-Okollo District. Permission was also sought from the administrators of the health facilities to access data about patients who had been admitted and those that had died. The authors sought verbal informed consent from the respondents who were survivors, next of kin of the deceased, local leaders, and police detectives. They were all informed that their participation was voluntary and their refusal would not attract any negative consequences. Data which was collected did not contain individual personal identifiers as a way of ensuring confidentiality.
Results
Descriptive epidemiology
A total of 48 suspected cases (47 male) were line listed, including 30 in Arua City (AR=8/100,000) and 18 in Madi-Okollo District (AR=10/100,000). The outbreak affected the 25-34-year age group (AR=27/100,000) more than other age groups (Table 1). Eighteen deaths were reported (case-fatality rate: 38%), including 12 in Arua City and 6 in Madi-Okollo District. The median age of cases was 32 years (IQR 26-46). Cases presented with blurred vision (79%), abdominal pain (77%), headache (70%), dizziness (69%), and other symptoms (Table 2).
Table 1: Attack rates and case fatality rate of methanol poisoning by age group, sex, and district among 48 cases of methanol poisoning during an outbreak in Arua City and Madi-Okollo District, Uganda, August 2022
| Characteristic | Population* | Total cases | Total deaths | Case fatality rate (%) | Attack rate per 100,000 people |
| Total | 255,889 | 48 | 18 | 38 | 19 |
| Age (years) | |||||
| 18-24 | 88,119 | 6 | 0 | 0 | 7 |
| 25-34 | 70,149 | 19 | 6 | 32 | 27 |
| 35-44 | 40,431 | 9 | 4 | 44 | 22 |
| ≥45 | 57,280 | 14 | 8 | 57 | 24 |
| Sex | |||||
| Male | 122,827 | 47 | 18 | 38 | 38 |
| Female | 133,062 | 1 | 0 | 0 | 1 |
| District | |||||
| Arua City | 172,945 | 30 | 12 | 40 | 17 |
| Madi-Okollo | 82,944 | 18 | 6 | 33 | 22 |
*Projected 2022 population based on the 2014 census
Table 2: Distribution of clinical signs and symptoms among 48 cases of methanol poisoning during an outbreak in Arua City and Madi-Okollo District, Uganda, August 2022
| Symptom | n | (%) |
| Blurred vision | 38 | 79 |
| Abdominal Pain | 37 | 77 |
| Headache | 34 | 70 |
| Dizziness | 33 | 69 |
| Profuse Sweating | 24 | 50 |
| Difficulty in breathing | 22 | 46 |
| Staggering movements | 20 | 42 |
| Chest pain | 20 | 42 |
| Shivering | 16 | 33 |
| Loss of vision | 15 | 31 |
| Fever | 14 | 29 |
| Loss of consciousness | 12 | 25 |
| Vomiting | 12 | 25 |
| Diarrhea | 7 | 14 |
| Confusion | 6 | 13 |
| Nausea | 2 | 4 |
| Others | 5 | 10 |
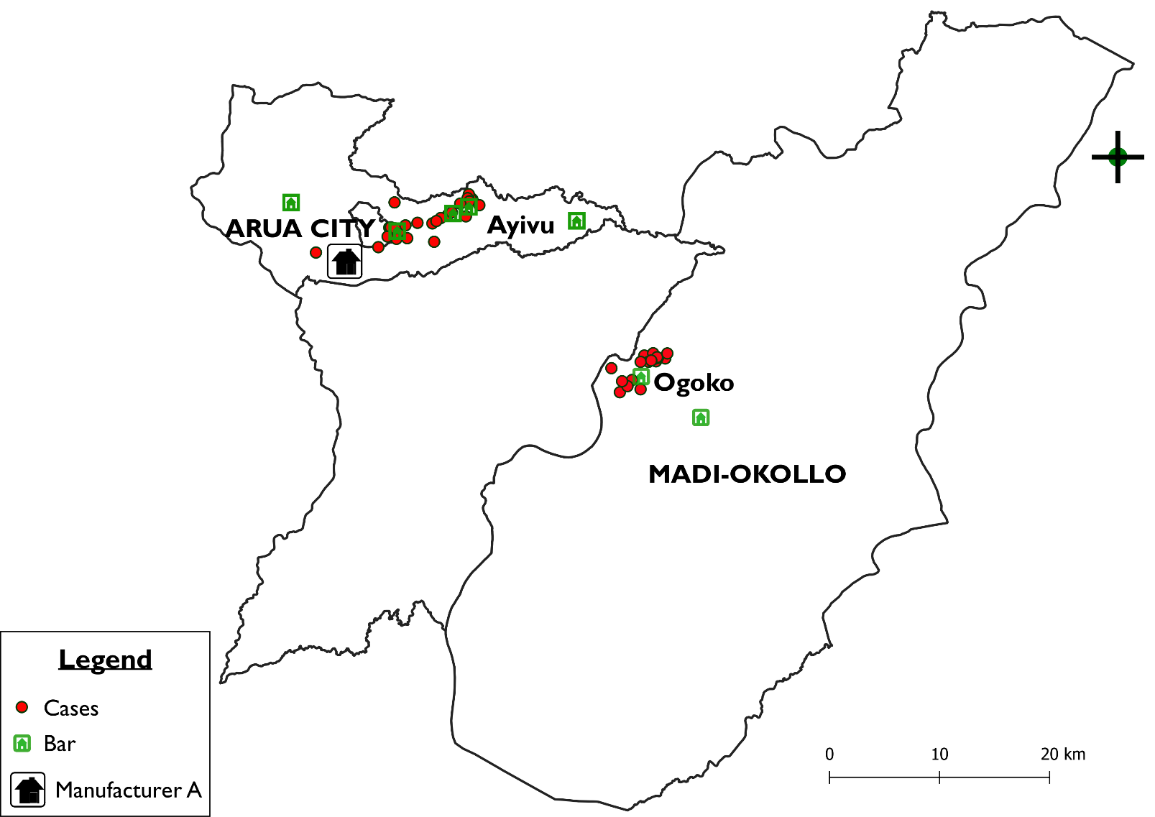
Cases were clustered around the bars which also acted as main distributors of gin X (Figure 2). This outbreak only affected one sub-county in each district. That is, Ayivu division in Arua City (AR=7/100,000) and Ogoko subcounty in Madi-Okollo District (AR=13/100,000).
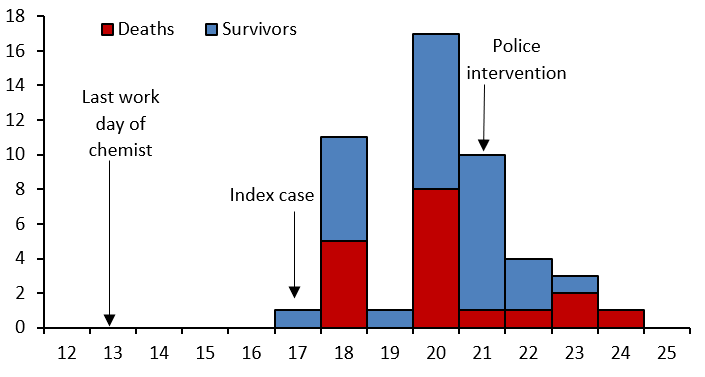
The index case first developed symptoms on 17 August and the last on 24 August 2022. The epidemic curve suggests a point source exposure lasting for 7 days (Figure 3). The number of cases reduced after police intervention on 21 August, 2022. This was done through closure of manufacturer A, seizure, and destruction of stock of the main distributors.
Case management
All cases consumed gin X from 17 to 23 August 2022 before the onset of symptoms. The average time between the last ingestion of alcohol and onset of symptoms was 13 hours (SD±6) and the mean time between onset of symptoms and death was 20 hours (SD±16).
Among the 18 deaths, 14 (78%) occurred in the community without accessing any health facility while the rest died in health facilities. Fourteen survivors (11 from Madi-Okollo District and 3 from Arua City) were referred to ARRH for treatment. The rest of the survivors were managed at home. The average duration of stay in the hospital for those who were admitted was two days. Despite having a diagnosis of methanol poisoning, none of the case-patients who were admitted in ARRH received intravenous ethanol, which is the recommended treatment.
Laboratory and autopsy investigation results
According to the UNBS report, among the eight samples picked from manufacturer A, five contained excessive concentrations of methanol above the maximum recommended limit of 50mg/L. Their mean methanol content was 594,424 mg/L (range 259,263-809,193 mg/L) [8]. All the eight autopsies that were conducted revealed liver inflammation, gastrointestinal bleeding and pulmonary oedema, all of which are consistent with methanol poisoning.
Trace-back investigation findings
After interviewing the cases, four bars which were the possible source of the implicated gin X were identified, that is, three in Arua City and one in Madi-Okollo District. These bars also acted as the main distributors of gin X in the region. Interviews with the bar owners reveled that they all got their supply of gin X from Manufacturer A located in Arua City.
Manufacturer A was a small-scale alcohol-producing company run in a home setting with production capacity of less than 1,000 liters per day. It had been in existence since 2001 and was fully licensed by UNBS to produce pineapple wine prior to this outbreak. Manufacturer A did not have an established storage, inventory, and warehouse management system. The bottles did not have serial numbers and the production batches lacked batch numbers.
In April 2022, manufacturer A started engaging in production of gin X and hired a chemist for this role. Production went on illegally without licensing from UNBS from April until August 2022.
At the beginning of August 2022, a disagreement ensued between the chemist and the proprietor of manufacture A which was concerning about the high cost of buying raw materials. It was alleged that the chemist would buy raw materials cheaply and then quote a higher figure to the proprietor. Despite this disagreement, the chemist continued to work until his last day of 13 August 2022. After the 13 August 2022 production, the chemist did not return back for work and all his known phone contacts were unreachable. Four days later, the index case appeared.
Retrospective cohort study findings
The risk of death increased significantly with increasing number of gin X bottles consumed (Table 3).
Table 3: Dose-response relationship among cases after consumption gin X in Arua City and Madi-Okollo District, Uganda during a methanol poisoning outbreak, August 2020
| Gin X quantity consumed | Alive n (%) | Dead n (%) | RR | 95% CI | p-value | |
| ≤ 1 bottle | 14 (46.7) | 1 (5.6) | Ref. | |||
| 2 bottles | 8 (26.6) | 3 (16.7) | 4.1 | (0.49 – 34.26) | 0.19 | |
| 3 bottles | 3 (10.0) | 6 (33.3) | 10 | (1.42 – 70.22) | 0.02* | |
| > 3 bottles | 2 (6.7) | 5 (27.8) | 10.7 | (1.52 – 75.35) | 0.02* | |
| Not specified | 3(10.0) | 3(16.6) | 7.5 | (0.96-58.59) | 0.06 | |
1 bottle (200ml size) contains 200mls of gin X
Discussion
This was a methanol poisoning outbreak following adulteration of illicit alcohol at production stage from manufacture A. Almost entirely only males were affected. Four out of ten people died after consumption of the gin X. The risk of death increased with increasing quantity of gin X consumed. This investigation highlights the need for enhanced food poisoning community-based surveillance and public awareness about the dangers of illicit alcohol.
The adulterated alcohol was traced back to manufacturer A, which was illegally producing the gin. Unrecorded and unregulated alcohol has been linked to several methanol poisoning outbreaks [9, 10]. The proportion of unregulated alcohol as a percentage of total alcohol is high among low income countries with an estimated value of 42 percent in Uganda [11]. Unregulated alcohol production possess a health security threat because its produced without regulatory and market oversight and hence increasing the risk of safety, poor quality, and chances of adulteration [9].
During this investigation, tracing back the exact batch where the poisonous alcohol gin X was drawn from was difficult because of poor store keeping practices of manufacturer A. The packaging of gin X lacked serial numbers which made it difficult in identifying the possible points of adulteration along the supply chain beyond the production stage. This improper documentation is contradictory to best practices of labelling and coding alcoholic beverages[12]. In future, proper labeling and coding of alcoholic batches by manufactures could allow efficient trace-back.
Males were the only ones who were entirely affected by this outbreak. This is in line with other Ugandan studies which show a huge gender disparity in regard to alcohol consumption where men consume alcohol more than women [13, 14]. It is not surprising that the methanol alcohol poisoning outbreak affected more men than women.
This outbreak caused 18 deaths with a Case Fatality Rate (CFR) of 38 percent. This is high compared to what has been reported in some African studies. Retrospective studies done in Libya (2013) and Kenya (May and July 2014) indicate that among 1,000 patients who were poisoned in Libya, 101 died corresponding to CFR of 10% while among the 341 and 126 cases in Kenya, 100 and 26 people died corresponding to 29% and 21% CFR respectively[15]. The deaths in our study were likely associated with not seeking proper health care as many cases didn’t go to health facilities and died at home. Wu X et al, 2022 note that early diagnosis and timely medical care are essential in reducing mobidity and motality of methanol poisoning [7].
Although methanol is present in most alcoholic drinks and poses no harm at low levels, excesses above 50g/L can be lethal [3]. As with other toxic agents, methanol toxicity is dose dependent. There was a significant increased risk of death with increasing dose of methanol consumed. This is in agreement with findings from a systematic review which was done in 2017 and concluded that the concentration of biological exposure indices and clinical symptoms for methanol exposure have a dose response relationship[16].
Study limitations
We were unable to confirm presence of methanol in blood of case-patients since at the time of the investigation most survivors had already been discharged from hospital or were recovering. The blood samples which were earlier collected by police, were not properly stored and were submitted late to the GAL. This could not permit analysis. However, the patients’ clinical presentations, epidemiologic data, laboratory toxicological findings, and post mortem results were all consistent with methanol poisoning.
Conclusion
We concluded that this outbreak was caused by consumption of gin X which was adulterated with high concentration of methanol at the production stage from manufacturer A. There could have been a possibility that this adulteration was intentional following the disagreement between the chemist and the proprietor. We recommend the enforcement of the laws that govern alcohol production and distribution in Uganda. The UNBS could carry out regular impromptu checks for methanol even on other previously certified alcoholic brands.
Public health actions taken
Immediately after the outbreak was detected the Ministry of Health instructed the investigation. With support from the Uganda Police Force and the UNBS, the implicated manufacturer was closed and stopped production on 21 August 2022. Two employees of manufacturer A and one of the main dealers of gin X in Arua city were apprehended on 21 August 2022 and prosecuted in courts of law. The chemist and the proprietor went on the run and were believed to have fled the country by the time of this investigation.
Stocks gin X were withdrawn from the major distributors and destroyed. Community sensitization was carried out with support from Arua City and Madi-Okollo District authorities on radio talk shows and community gatherings. Community event-based surveillance was strengthened where members of the community were encouraged to report any suspicious alcohol related symptoms and deaths to the local health authorities.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgements
The authors thank the staff of the Public Health Fellowship Program for the technical support and guidance offered during this study.
The authors also extend their appreciation to the Ministry of Internal Affairs, particularly the Government Analytical Laboratory for the laboratory investigations, the Uganda Police Force for availing the Post Mortem results, and providing access to suspects, and providing security the factory tour.
We also appreciate the Uganda Prisons for the assistance offered to us while interviewing the suspects. Furthermore, the authors extend their appreciation to Arua City and Madi-Okollo local council and health authorities for the support offered during investigation.
Lastly the team also appreciates the administration of Arua Regional Referral hospital, Arua Regional Emergency Operations center, and the West Nile Regional WHO office for the support they offered during investigation.
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Joshi DR, Adhikari N: An overview on common organic solvents and their toxicity. J Pharm Res Int 2019, 28(3):1-18.
- Ott J, Gronemann V, Pontzen F, Fiedler E, Grossmann G, Kersebohm DB, Weiss G, Witte C: Methanol. Ullmann’s encyclopedia of industrial chemistry 2000.
- Paine A, Davan AD: Defining a tolerable concentration of methanol in alcoholic drinks. Human & experimental toxicology 2001, 20(11):563-568.
- Ashurst JV, Nappe TM: Methanol toxicity. 2018.
- Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA: American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. Journal of toxicology Clinical toxicology 2002, 40(4):415-446.
- Ssebunnya J, Kituyi C, Nabanoba J, Nakku J, Bhana A, Kigozi F: Social acceptance of alcohol use in Uganda. BMC psychiatry 2020, 20(1):1-7.
- Wu X, Gu M, Wang W, Zhang H, Tang Z: Case Report: Early Recognition, Treatment, and Occupational Safety Protection are Crucial for Methanol Toxicity. Frontiers in Medicine 2022, 9.
- UNBS: Uganda National Bureau of Standards (UNBS); Statement on Adulterated Gin (City5) and Death of Consumers in Arua City and Neighbouring Districts. In.; 2022.
- Manning L, Kowalska A: Illicit Alcohol: Public Health Risk of Methanol Poisoning and Policy Mitigation Strategies. Foods (Basel, Switzerland) 2021, 10(7).
- Rehm J, Kailasapillai S, Larsen E, Rehm MX, Samokhvalov AV, Shield KD, Roerecke M, Lachenmeier DW: A systematic review of the epidemiology of unrecorded alcohol consumption and the chemical composition of unrecorded alcohol. Addiction (Abingdon, England) 2014, 109(6):880-893.
- Probst C, Manthey J: Unrecorded alcohol use: a global modelling study based on nominal group assessments and survey data. 2018, 113(7):1231-1241.
- Vukatana K, Sevrani K, Hoxha E: Wine Traceability: A Data Model and Prototype in Albanian Context. Foods (Basel, Switzerland) 2016, 5(1):11.
- Kabwama SN, Ndyanabangi S, Mutungi G, Wesonga R, Bahendeka SK, Guwatudde D: Alcohol use among adults in Uganda: findings from the countrywide non-communicable diseases risk factor cross-sectional survey. Global health action 2016, 9:31302.
- Wagman JA, Nabukalu D: Prevalence and correlates of men’s and women’s alcohol use in agrarian, trading and fishing communities in Rakai, Uganda. 2020, 15(10):e0240796.
- Rostrup M, Edwards JK, Abukalish M, Ezzabi M, Some D, Ritter H, Menge T, Abdelrahman A, Rootwelt R, Janssens B: The methanol poisoning outbreaks in Libya 2013 and Kenya 2014. PloS one 2016, 11(3):e0152676.
- Moon C-S: Estimations of the lethal and exposure doses for representative methanol symptoms in humans. Annals of Occupational and Environmental Medicine 2017, 29(1):44.


Comments are closed.