Measles outbreak Investigation in Terego District, Uganda, May- June, 2024.
Authors: Annet Mary Namusisi1*, Yasiini Nuwamanya1, Richard Migisha1, Rita Atugonza2, Ampaire Immaculate2, Fred Nsubuga2, Benon Kwesiga1, Alex Riolexus Ario1. Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Uganda National Expanded Program on Immunization, Ministry of Health Uganda, Kampala, Uganda; Correspondence*: Tel: +256785859760, Email: annetnamusisi@uniph.go.ug
Summary
Background: The Ministry of Health (MoH) received a notification of a measles outbreak in Terego District, Uganda, on April 30, 2024. We investigated to determine the scope of the outbreak, assess risk factors for transmission, Vaccine effectiveness (VE), Vaccine coverage (VC), and recommend evidence-based control and prevention measures.
Methods: We defined a suspected case of measles as onset of fever and maculopapular rash, plus ≥1 of the following; cough, runny nose (coryza) conjunctivitis (red eyes) in a resident of Terego District from February 1, 2024 to June 1, 2024. A confirmed case was defined as a suspected case that tested positive for IgM measles-specific antibody test. We identified case-patients in health facility registers and active case searched to update the line-list using our case definitions. We conducted a 1:1 unmatched case-control study and used logistic regression to identify exposures associated with measles infection. We estimated vaccine coverage and effectiveness in the district.
Results: We identified 136 case-patients (132 suspected case-patients and 4 confirmed case-patients and no deaths). The index case had returned from Ediophe HCIII in Arua City where she was co-caretaking a relative’s child that had been admitted on ward with measles-like symptoms. The median age was 4.1 years (IQR: 1.5-9) and 0-6 months age group was the most affected with AR (220/100,000). Females were more affected (AR=64/100,000) compared to males (AR=42/100,000). Vaccination was 60% protective against measles (aOR=0.4, 95% CI=0.2,0.8). Visiting any health facility (aOR=4.4, 95%CI=1.4,14), attending a public gathering (aOR=4.9, 95%CI=2.01, 12), and visiting a place of worship (aOR=19, 95%CI=1.8, 206) were associated with acquisition of measles disease. VE was 60% (95% CI=20-80) and VC was 71%.
Conclusions: The measles outbreak in Terego District was imported from Arua City and facilitated by suboptimal vaccine effectiveness, low vaccine coverage in the affected sub counties, nosocomial spread in health facilities, and community gatherings. The district should take deliberate measures to improve routine immunization coverage to strengthen herd immunity thereby mitigating risk of future measles outbreaks.
Background
Measles is a highly contagious disease caused by the measles virus. The disease is spread from person to person through inhalation of infected respiratory droplets, within an incubation period of 7-21 days (1). Due to its high infectivity rate, where one infected individual averagely transmits the disease to 12 to 18 individuals in a susceptible population, it has been associated with several outbreaks globally (2).
Since 2018, measles has been one of the leading causes of morbidity and mortality among the vaccine preventable diseases in children <5 years (3). In 2022, there was a global rise in measles case-patients by 18% and measles deaths by 43% compared to 2021, approximating to 9 million case-patients and 136,000 deaths. The rise was due to disruptions in the healthcare systems from 2020 to 2021 following the COVID-19 pandemic. The disruptions resulted into many children missing out on their routine immunization, especially during the lock down when immunization services were suspended (7). During the same period, the vaccination coverage for measles-containing vaccine (MCV 1) was 81% and 71% for MCV2 (4). In 2022, Africa contributed halfway to the burden of measles case-patients in the world, with Sub-Saharan Africa exhibiting the highest number approximating to 17,500 measles case-patients (5). In Uganda, measles is the most reported outbreak(6).
Furthermore, it is important to note that immunization is the most effective way to reduce measles infections and transmission. Despite availability of measles vaccines, given in 2 doses in Uganda, the country is still faced with increasing numbers of measles outbreaks each year, often affecting children under 5 years of age (8) . In January 2024, the country faced 8 measles outbreaks in 8 districts including Terego (9). On April 30, 2024, Ministry of Health received a notification about a measles outbreak in Terego District, through the Public Health Emergency Operations Centre (PHEOC). This occurred after four out of seven samples tested from the Uganda Virus Research Institute (UVRI) turned positive for Measles specific IgM antibodies. We investigated to determine the scope of the measles outbreak, assess risk factors for transmission, vaccine coverage, and effectiveness, and recommend evidence-based control and prevention measures.
Methods
Outbreak setting
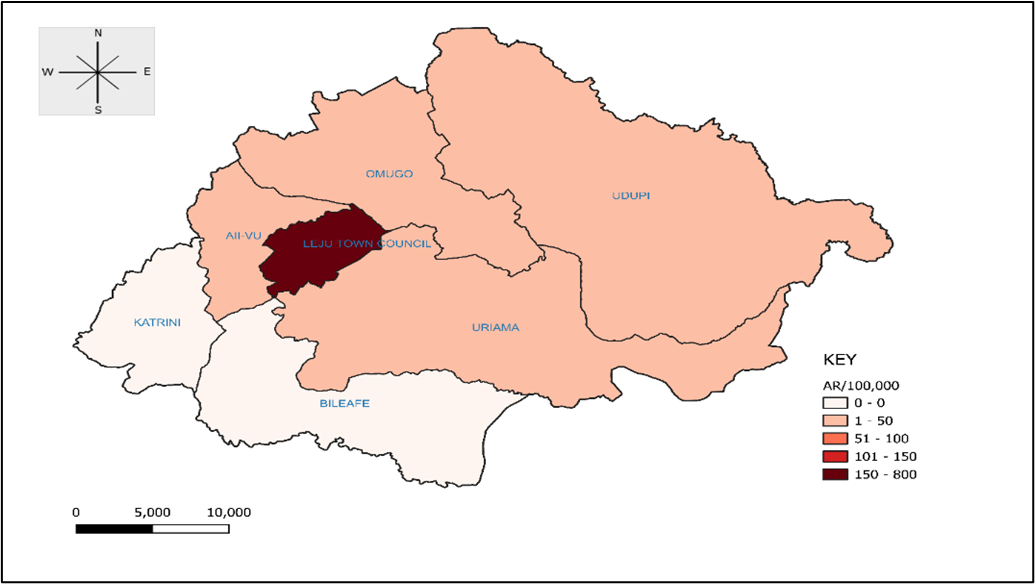
Terego is a new rural district in West Nile part of northern Uganda, established in 2020. It has a population of 394,319 people, which consists of natives and refugees from 2 refugee settlements. The district comprises of seven sub-counties (SC): Aii-Vu, Bileafe, Katrini, Odupi, Omugo, Uriama, Leju Town council and 39 parishes, with its headquarters in Leju town council (10). The measles outbreak occurred in 5 sub-counties; Aii-Vu, Omugo, Udupi, Uriama and Leju Town council.
Case definition and finding
We defined a suspected case of measles as onset of fever and maculopapular rash, with one or more of the following: cough, runny nose (Coryza) or conjunctivitis (red eyes) in a resident of Terego District from February 1, 2024 to June 1,2024. A confirmed case was a suspected case that has been confirmed positive for IgM measles-specific antibody test.
We reviewed patient records to identify measles case-patients that visited health facilities in Terego District since February, 2024, and updated the line list. Leju Town council had the highest number of case-patients compared to the other sub-counties, and we selected it for active case search. We actively searched for additional case-patients at Obofia HCII and communities in Leju Town council, with the help of the Health Assistants (HAs) and Village Health Teams (VHTs). Obofia HCII is the major health facility serving people from far and wide in Leju Town council. We interviewed case-patients using a standard Case Investigation Form (CIF) to obtain information on demographic characteristics, clinical features, vaccination and social history. Vaccination history was assessed by vaccination card availability and recall of the parent with demonstration of knowledge on site of vaccination.
Descriptive epidemiology
We described the line-listed case-patients by place, person, and time. Person characteristics included sex and age. We used 2024 population projections from the Uganda Bureau of Statistics (UBOS) to obtain the mid-year population for the different age groups for Terego District to calculate the attack rates by age and subcounty. Using the Quantum Geographic Information System (QGIS) software, we constructed choropleth maps to display attack rates by place. We summarized distribution of case-patients by time of skin rash onset using an epidemiological curve.
Laboratory investigations
Whole blood was collected from 7 suspected case-patients for measles IgM antibody testing.
Environmental assessment
We observed the turn up for vaccination at Obofia HCII and movement of people outside Terego District and from neighboring districts and countries like Democratic Republic of Congo. We interviewed caretakers, health care workers at the HCII, and the Local Council V chairperson to obtain information regarding people’s perceptions about measles and measles vaccinations, and possible causes of the measles outbreak in the district. We observed for control measures instituted by the caretakers with children suffering from measles during home interviews.
Hypothesis generation
We conducted 30 hypothesis generating interviews using a measles case investigation form. Case-patients or their caretakers were interviewed on a number of potential risk factors that occurred within three weeks prior to symptom onset, such as: visiting a health facility, travelling outside Terego, being vaccinated, close proximity to someone with a rash during church service and playing away from home.
Case control study
We conducted a 1:1 unmatched case-control study to evaluate the possible risk factors that emerged during hypothesis generation. The study focused at Leju Town council since it had the highest attack rate for measles compared to the other six sub counties. A control was defined as a person residing in Terego district with no history of fever or rash from February 1, 2024 to June 1, 2024. Controls were obtained from neighborhood (who had not had a measles case before) to ensure both case-patients and controls had comparable exposures. An interviewer-administered questionnaire was used to obtain information on demographics, clinical characteristics, and other risk factors to measles disease. We used logistic regression to identify factors associated with measles transmission.
Vaccine Effectiveness (VE)
We estimated vaccine effectiveness for measles vaccine using the formula VE=1-aOR where aOR were the protective odds (adjusted OR from logistic regression) of having been vaccinated at least once with MR vaccine.
Vaccine Coverage (VC)
We estimated vaccine coverage using the proportion of eligible vaccinated respondents among the control group.
Ethical considerations
This outbreak investigation was conducted in response to a public health emergency by the National Rapid Response Team. The Ministry of Health (MoH) gave permission to investigate this outbreak. In addition, a non-research determination clearance from the US Centers for Disease Prevention and Control (US CDC) was sought. The investigation was approved by US CDC and conducted in accordance to the applicable US federal laws. § §See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
We sought permission to conduct the investigation from District health authorities of Terego District. Since the investigation presented no more than minimal risk of harm and involved no procedures for which written consent is normally required, we sought verbal informed consent or assent for interviews, from the respondents. We ensured privacy during all interviews and case-patients information was kept confidential throughout the investigation period and beyond.
Results
Descriptive epidemiology
Overall, 136 case-patients (AR=53/100,000) were identified including 4 confirmed case-patients and no deaths. The median age was 4.1 years (IQR=1.5-9). Case-patients with age group 0-6 months were the most affected (AR=220/100,000 case-patients) followed by 1-4 years (AR=110/100,000). Females were more affected (AR=64/100,000) than males (AR=42/100,000). Among the seven sub-counties, Leju Town Council was the most affected (AR=793/100,000), followed by Omugo (AR= 18/100,000), Uriama (AR=8/100,000), Udupi and Aii-Vu each (AR= 2/100,000). Two sub-counties; Bileafe and Katrini did not register any measles case-patients (Figure 3).
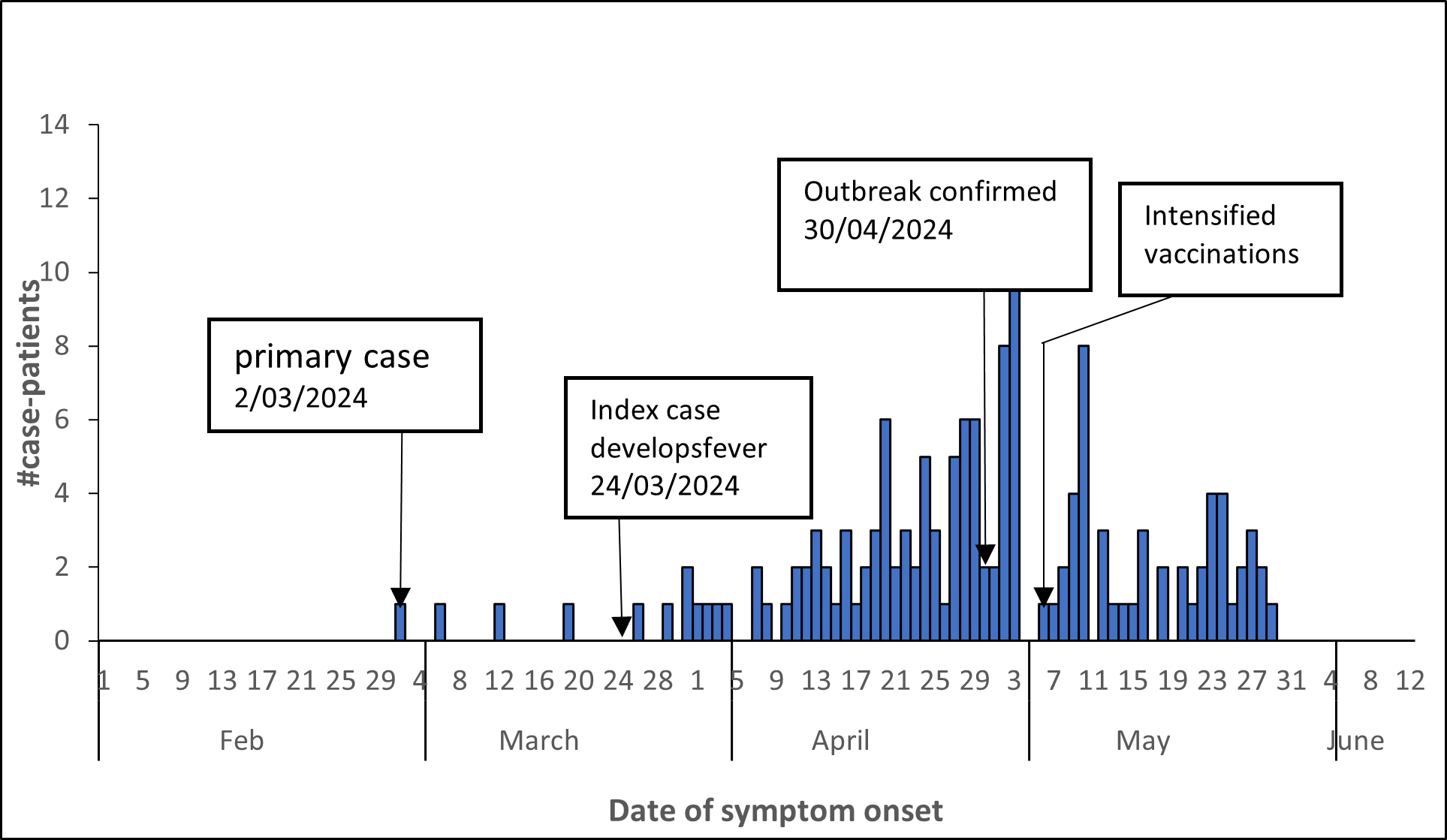
Measles transmission occurred rapidly from one person to another. The primary case was a 5 months old male, AB from Leju TC who developed skin rash on March 2, 2024. He had no history of travel outside Terego District or household contact with a case or transmission to any member of the household. In this outbreak, the index case was a 36-year-old woman, BB from Osua village, Leju T/C who developed symptoms on March 24, 2024. A week prior to symptom onset, she reported visiting Ediophe HCIII in Arua City where she accompanied her relative on the ward who was taking care of her sick child and stayed over for 6 days. The sick child had been admitted with measles-like symptoms including fever and rash, and BB reports that there were several other children with similar signs and symptoms on the ward. On April 17, 2024 samples from 7 people were taken off and sent to UVRI, 4 of which including the one for the index case tested positive for IgM antibodies. On April 30, 2024 Ministry of Health (MoH) declared an outbreak for measles in Terego District. Several suspected case-patients were line listed thereafter and from May 06, 2024 supplementary immunization campaigns were intensified. There were no new reported case-patients since May 29, 2024 (Figure 2).
Environmental assessment findings
Many mothers deliver from government health facilities in the nearby sub counties and leave their children’s immunization cards there. These cards are kept by the health workers to avoid being misplaced by the mothers. As a result, mothers are not aware of the next vaccination appointments and hence do not return back to Obofia HCII for their children’s vaccinations. We also observed that sick children (with measles) were not isolated at home and instead lived normally with the rest of the family members, thereby further spreading the measles infection in the household. Interviews with the LCV revealed that people in the communities were not aware of MR2 vaccine presence and their children were vaccinated only with MR1.
Hypothesis generation findings
Potential risk factors to measles transmission were: Being in close proximity to someone with a rash during church service, not vaccinated against measles, and playing away from home (Table 1). We therefore designed a case-control study to test the hypotheses.
Table 1: Potential exposures associated with measles outbreak in Terego District, Uganda, February-June 2024
| Potential risk factors | Case-patients (%) |
| Close proximity to someone with a rash during church service | 30 (100) |
| Not vaccinated against measles | 26 (87) |
| Playing away from home | 26 (87) |
| Visiting a health facility within 3 weeks prior to symptom onset | 22 (73) |
| Travelling outside Terego within 3 weeks prior to symptom onset | 21 (70) |
Factors associated with measles transmission in Terego District, February-June 2024
At multivariable analysis, vaccinated individuals were 60% less likely to develop measles compared to the unvaccinated (aOR= 0.4; 95% CI=0.2,0.8). The odds of developing measles disease among individuals who visited a health facility since February prior to the outbreak were 4.4 times the odds in those who did not visit. (aOR = 4.4; 95% CI=1.4,14). The odds of developing measles disease in those who attended a public gathering were 4.9 times the odds in those who did not attend a public gathering (aOR = 4.9, 95% CI=2.01,12). The odds of developing measles disease in individuals who attended a place of worship were 19 times the odds in those who did not visit any place of worship (Table 2).
Table 2: Risk factors for measles outbreak investigation in Terego District, Uganda, February-June 2024
| Risk factor | Number (%exposed) | cOR
(95% CI) |
aOR
(95% CI) |
|
| Case-patients n (%) | Controls n (%) | |||
| Vaccinated against measles | 27(34) | 57(71) | 0.2 (0.1-0.4) | 0.4 (0.2-0.8) |
| Attending a public gathering | 59 (74) | 17(21) | 10 (5.01-22) | 4.9 (2.01-12) |
| Current school attendance | 17(71) | 12(86) | 0.4 (0.04-2.7) | |
| Received a visitor from Arua City | 12(15) | 4(5.0) | 3.4 (0.95-15) | 3.5 (0.7-18) |
| Received a visitor from South Sudan | 6(7.5) | 1(1.3) | 6.4 (0.7-298) | |
| Sharing a water source | 59 (74) | 41(51) | 2.7 (1.4-5.2) | 1.1 (0.5-2.6) |
| Visiting a place of worship | 79(99) | 69(86) | 13 (1.6-100) | 19 (1.8-206) |
| Visiting any health facility | 32 (40) | 6(7.5) | 8.2 (3.2-21) | 4.4 (1.4-14) |
cOR refers to crude Odds Ratio
aOR refers to adjusted Odds Ratio
Measles Vaccine effectiveness
From the case-control analysis, 34% (27/80) of case-patients compared to 71% (57/80) 0f control-persons had received the measles vaccine at least once and this was 60% protective against measles disease (0.4 (0.2-0.8)). Therefore, the vaccine effectiveness was estimated at 60%.
Measles vaccination coverage
Approximately 71% (57/80) control-persons had received at least one dose of measles vaccine. The vaccine coverage was estimated at 71%.
Discussion
Our investigation revealed an imported measles outbreak from Arua City, propagated by attending a public gathering, visiting a place of worship and visiting any health facility prior to the outbreak period. On the other hand, vaccination with measles-rubella (MR) vaccine was found to offer protection against acquisition of the disease among residents in Terego District.
The index case was from Leju TC and may have transmitted to many people there. The most affected age group was 0-6 months followed by 1-4 years and 7-11months, with 15+ years the least affected. This is because children 0-6 months have lower immunity compared to older age groups and largely depend on herd immunity from the vaccinated population. However, if the community has a low vaccination coverage, the population that are not eligible for vaccination are prone to getting the infections. Important to note that vaccination in Uganda is focused on children 9 months and above, since its known that the children 0-5 months are protected by maternal antibodies that continue to wane off as they mature, hence they largely depend on herd immunity from older children (11). The vaccine effectiveness was 60% in this investigation and the vaccine coverage was 71%. The coverage is lower than WHO recommended minimum target of 95%, which is required for herd immunity.
Children vaccinated against measles disease were 60% less likely to develop measles compared to the unvaccinated. Our findings are similar to those by Gressick et al, where MMR vaccinations offered substantial protection against measles disease(3). Immunization is the most effective way to reduce measles infections and transmission and measles vaccination was estimated to avert 57 million deaths globally, from 2000-2022 (12, 13).
Individuals who visited a health facility for health care services other than measles disease management since February 2024 were more likely to develop measles disease compared to those who did not go to any health facility in the same period. Measles is a highly contagious disease and will be highly spread from close contact in confined spaces with infected patients. Our findings coincide with other studies which show that healthcare settings are hot spots for measles transmission due to nosocomial spread of infectious agents to susceptible individuals in hospitals (14, 15). Attending a public gathering, and visiting a place of worship were associated with developing measles disease. People who attended a public gathering such as market, funeral, party were more likely to develop measles disease compared to their counterparts who did not. Similarly, people who went for prayers at places of worship were more likely to get measles disease compared to their counterparts who did not. Our findings are consistent with findings for a study in China and Uganda where high-density population propagated the spread of measles disease (6, 16). This is because during public gatherings and congregation, there is increased close contact between healthy and diseased people, hence easy transmission of the measles virus.
Study limitations
We used the control population from Leju Town council to calculate the vaccine coverage of the entire district since this was the most affected subcounty. However, this coverage may not be representative of the overall vaccine coverage in the district.
Conclusion
This was an imported outbreak from Arua City, propagated by low vaccination coverage, high density gatherings, and visiting hospital settings. The most affected age group was 0-6 months.
Public health actions
The District Task Force was activated on May 1, 2024 to respond to the outbreak.
We intensified measles surveillance through active case search at health facilities and communities. We sensitized political leaders and enhanced social mobilization and risk communication. The district health workforce intensified routine measles vaccination. A mass measles vaccination campaign was conducted targeting all children aged 6-59 months, in June 2024.
Recommendations
Routine measles vaccination targeting children from 6 months instead of 9 months, would increase herd immunity in the population.
Enhancing static measles vaccinations and outreaches by carrying out door to door vaccination outreaches would ensure no child is left behind.
Intensifying health education on child vaccinations during antenatal care services would increase maternal knowledge about vaccination.
Designating isolation facilities for sub-counties that have only HCIIs to enable isolation of patients with infectious diseases like measles would limit disease transmission during any gatherings.
Conflict of interests
The authors declare that they have no conflict of interests.
Authors’ contributions
AMN, YN, designed the study and contributed to the data collection and analysis. AMN led the writing of the bulletin. AMN, YN, RM participated in bulletin writing and review to ensure scientific integrity and intellectual content. All the authors contributed to the final draft of the bulletin.
Acknowledgements
We appreciate the management of Terego District Local Government and Obofia HCII for their stewardship, and the community for their participation in this investigation. We also thank the Ministry of Health through Uganda National Expanded Program for Immunization (UNEPI) for their technical support. We are grateful to Global Alliance for Vaccines and Immunization (GAVI) and the US CDC for funding this investigation.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Husada D, Kusdwijono, Puspitasari D, Kartina L, Basuki PS, Ismoedijanto. An evaluation of the clinical features of measles virus infection for diagnosis in children within a limited resources setting. BMC Pediatrics. 2020;20(1):5.
- Parums DV. A Review of the Resurgence of Measles, a Vaccine-Preventable Disease, as Current Concerns Contrast with Past Hopes for Measles Elimination. Medical science monitor : international medical journal of experimental and clinical research. 2024;30:e944436.
- Organisation. WH. Disease outbreak news. 28 April 2023.
- (CDC) CfDC. Global Measles Vaccination. 2024 JULY 15, 2024.
- Nchasi G, Paul IK, Sospeter SB, Mallya MR, Ruaichi J, Malunga J. Measles outbreak in sub-Saharan Africa amidst COVID-19: A rising concern, efforts, challenges, and future recommendations. Annals of medicine and surgery (2012). 2022;81:104264.
- Nsubuga EJ, Morukileng J, Namayanja J, Kadobera D, Nsubuga F, Kyamwine IB, et al. Measles outbreak in Semuto Subcounty, Nakaseke District, Uganda, June-August 2021. IJID regions. 2022;5:44-50.
- Hussein SZ, Mardia N, Amirah M, Hashim R, Abu Bakar SH. Knowledge and Practice of Parents Towards Measles, Mumps and Rubella Vaccination. The Malaysian journal of medical sciences : MJMS. 2022;29(3):90-8.
- Organization WH. Measles. 12 July 2024.
- (IFRC) IFoRCaRCS. UGA: Epidemic – 01-2024 – Measles Outbreak.
- GmbH GCG. SFD Report Terego District Uganda. 2021 2021.
- Fleurette M. Domai KAA, Su Myat Han, Ana Ria Sayo, Janine S. Ramirez, Raphael Nepomuceno et al. Measles outbreak in the Philippines: epidemiological and clinical characteristics of hospitalized children, 2016-2019. THE LANCET Regional Health. 2022;19.
- WHO. Measles Fact sheet. 2024.
- Organisation WH. measles fact sheet. 2023 2023.
- Sultana Habibullah JA, M. Shakeel Aamir Mullick. Case-control Study for Measles Outbreak in a Tertiary Care Hospital. 2014.
- Biribawa C, Atuhairwe JA, Bulage L, Okethwangu DO, Kwesiga B, Ario AR, et al. Measles outbreak amplified in a pediatric ward: Lyantonde District, Uganda, August 2017. BMC infectious diseases. 2020;20(1):398.
- Qin S, Ding Y, Yan R, He H. Measles in Zhejiang, China, 2004-2017: Population Density and Proportion of Floating Populations Effects on Measles Epidemic. Health Security. 2019;17(3):193-9.


Comments are closed.