Measles outbreak imported through the porous border in Moroto District, Uganda, March–July, 2024
Authors: Emmanuel Mfitundinda1*, Annet Namusisi1, Daniel Wenani1, Ruth Ayeerwot2, Emmanuel Korobe3, Druscillah Ssekandi4, Richard Migisha1, Benon Kwesiga1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Karamoja Regional Emergency Operations Centre, Moroto, Uganda, 3Moroto District Local Government, Moroto, Uganda, 4Uganda National Expanded Immunization Program, Ministry of Health, Kampala, Uganda Correspondence*: Tel: +256 777 166 851, Email: emmamfitundinda@uniph.go.ug
Summary
Background: On 26 June, 2024, Ministry of Health Uganda was notified of a measles outbreak in Moroto District. We investigated the outbreak to determine its magnitude, identify the source, identify risk factors for transmission, and recommend evidence-based control measures.
Methods: We defined a suspected case as onset of fever and maculopapular rash, plus ≥1 of: cough, coryza, or conjunctivitis in a resident of Moroto District from 15 March to 23 July, 2024. A confirmed case was a suspected case with a positive measles-specific IgM test. Cases were identified through review of health facility records and active case search within the health facilities. We calculated case fatality rate (CFR), and attack rates (AR) by sub-county and age group. We conducted an unmatched case-control study (1:2) and used logistic regression to identify risk factors. We estimated the vaccine effectiveness (VE) from adjusted odds ratio (aOR) associated with vaccination (VE=1-aOR) % and vaccination coverage (VC) from percentage of vaccinated controls.
Results: We identified 236 case-patients (218 suspected cases, and 13 confirmed cases). There were five deaths (CFR=2%) of suspected cases. The index case was a 10-month-old male who had travelled with the mother from the Western Turkana Region of Kenya, where a measles outbreak was ongoing. The overall Attack Rate (AR) was 19/10,000. Lotisan Sub-county (AR=50/10,000) and children <1 year (AR=194/10,000) were the most affected. Being vaccinated was 89% protective (aOR=0.11, 95%CI=0.03-0.4). Visiting a health facility 7–21 days before the onset of rash (aOR=3.8, 95%CI=1.3-11) and malnutrition (aOR=6.1, 95%CI=1.3-27) increased the odds of contracting measles. Estimated VC was 67% and VE was 89% (95%CI=60-97).
Conclusion: The outbreak was likely imported from Kenya, and was propagated by low vaccination coverage, nosocomial infections and malnutrition. Improved triage, mass vaccination campaigns for children aged 6–59 months and strengthened cross-border disease surveillance could prevent future similar outbreaks.
Introduction
Measles is a highly infectious viral vaccine preventable disease with a high burden in children <5 years of age. Without vaccination, >90 % of people would be infected by the age of 10 years with a symptomatic form of the disease (1). It is transmitted through respiratory droplets and by direct contact with infected nasal or throat secretions (1, 2). The incubation period of measles is 7–21 days. Measles presents with high-grade fever, maculopapular rash, cough, running nose and conjunctivitis. The maculopapular rash erupts 3–5 days after the onset of the fever, it starts from the face and spreads to the rest of the body. The Case Fatality Rate (CFR) of measles is 3-10% in developing countries. Complications of measles include pneumonia, diarrhea, otitis media and encephalitis in rare cases. Risk factors for severe disease include malnutrition, advanced HIV disease, age < 5 years and living in very crowded conditions (1).
The World Health Organization (WHO) recommends two doses of MCV with the first dose administered between 9 and 12 months of age and the second dose administered at the age of 15–18 months of age, the second dose should be at least one month apart from the first one(1). In Uganda, the coverage for MCV1 was suboptimal at 85% in 2022. The country introduced the second dose of MCV in 2022 but it’s coverage remains suboptimal at 44% in 2022 (5, 6). To achieve herd immunity and prevent outbreaks, the coverage should be at least >93% at a district level. As a result of this suboptimal MCV coverage, Uganda has experienced numerous measles outbreaks since 2018 as a result of the suboptimal coverage across the country (7,8, 9, 10, 11).
On June 26, 2024, the Ministry of Health (MoH) through the National Emergency Operations Centre received a notification of a measles outbreak in Moroto District, Karamoja Region, Uganda. Nine out of the13 suspected case-patients tested at the Uganda Virus Research Institute (UVRI) werepositive for measles-specific Immunoglobulin M (IgM) antibodies. We investigated to determine the scope, identify the source of the outbreak, assess risk factors for transmission, vaccine effectiveness, and vaccine coverage, and recommend evidence-based control and prevention measures.
Methods
Outbreak area
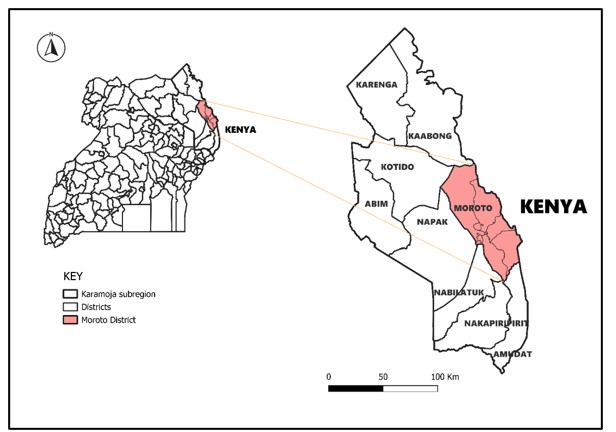
We conducted the investigation in Moroto District in Karamoja Region, North Eastern Uganda (Figure 1). This region is inhabited by the Karamojongs who are nomadic pastoralists in nature. The district neighbours the Turkana region of Kenya which is also occupied by nomadic pastoralists known as the Turkana people (10). Both people have intertwined cultures with a lot in common Moroto District has 18 health facilities and of them, 17 offer immunization services.
Case definition and finding
We defined a suspected case as onset of fever and maculopapular rash and one or more of the following symptoms: cough, runny nose or conjunctivitis in a resident of Moroto District from March 15, 2024 to July 23, 2024. A confirmed case was a suspected case with positive results for IgM measles-specific antibody test in a resident of Moroto District from March 15, 2024 to July 23, 2024.
We line-listed suspected measles cases by reviewing health facility records at Moroto RRH and St. Pius, Kidepo HC III. We found additional cases with the help of Health Facility Surveillance Focal Persons (HFSFP) who reviewed records at their health facilities where we couldn’t reach because of insecurity. We used standard case investigation forms to collect data on demographics, clinical characteristics, vaccination status, exposure history, treatment, and admission history of the case-patients.
Laboratory investigations
Samples of whole blood from 13 suspected case-patients were collected and sent to Uganda Virus Research Institute (UVRI) for Measles specific IgM testing.
Descriptive epidemiology
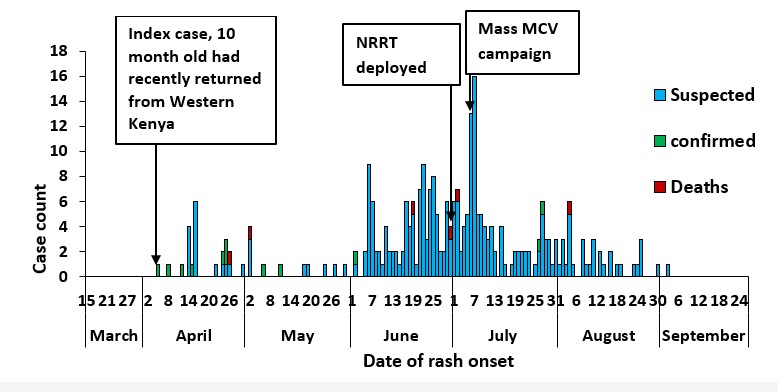
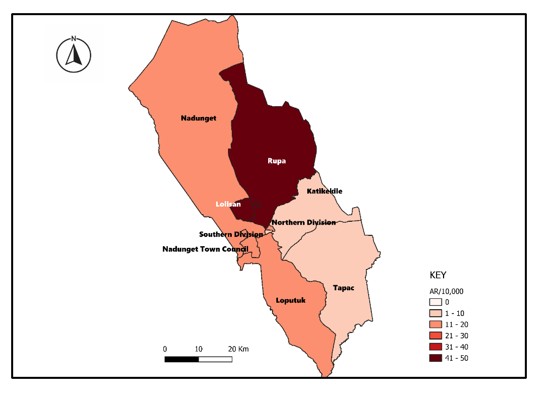
We constructed an epidemic curve to determine the distribution of measles cases over time. We computed Attack Rates (AR) by person, and place using projected populations from the Uganda Bureau of Statistics (UBOS) as the denominator and presented the results using tables. We described AR by place by depicting on maps using Quantum Geographic Information System (QGIS).
Hypothesis generation and case control study
We conducted 30 hypothesis generating interviews from suspected case-patients using the measles case investigation form. We asked the caretakers about the potential exposures that could have occurred within three weeks prior to the onset of symptoms. We also held interviews with the District Health Team (DHT) about the possible exposure factors and the source.
We conducted a case-control study to evaluate the generated hypotheses. We recruited 83 case patients. For each case, we selected two controls with no history of fever, rash and conjunctivitis from March 15 to July 23, 2024 with an alternative diagnosis on admission made by either a pediatrician or a medical officer, aged 6 months – 5 years and residents of Moroto District. We identified factors associated with measles transmission using logistic regression.
Vaccine coverage (VC) and vaccine effectiveness estimation (VE)
We estimated the VC using the percentage of controls with a history of measles vaccination in the case control study, assuming that the controls were representative of the general population. We calculated VE using the formula:
VE = 1- aOR
Where aOR is the odds ratio associated with having been vaccinated for at least one dose of measles vaccine, adjuster for risk factors that were significant during the univariate analysis, using conditional logistical regression.
Ethical considerations
The Ministry of Health of Uganda gave the directive and gave approval to investigate this outbreak. The Office of the Associate Director for Science at the US Centres for Disease Control and Prevention (CDC) Uganda determined that this research did not involve human subject research and that its primary intent was public health practice or disease control. Verbal informed consent was obtained from participants or, if the interviewee was a minor, guardians before the start of each interview.
Results
Descriptive epidemiology
We identified 290 (269 suspected cases, 15 confirmed cases and 6 deaths). The epidemic curve shows a propagated pattern with multiple peaks over the outbreak period (Figure 2). The index case was a 10-month-old from Kosiroi Village in Tapac Sub-county that is next to the Kenyan border of Western Turkana Region (Figure 3). He had received one dose of MCV. He had recently travelled from this region of Kenya alongside his mother. This region had an ongoing measles outbreak. Five deaths were recorded during this outbreak. All the deaths occurred at Moroto RRH and died of complications of severe pneumonia with underlying malnutrition. Three of the deaths were unvaccinated and two had unknown history of vaccination.
All cases presented with fever and generalized rash. The majority of the cases had running nose (71%), and red eyes (67%). Other symptoms were cough, diarrhea, generalized body weakness, poor feeding. 22% (52/236) of the cases had complications. The common complications during this outbreak were diarrhea (16%), diarrhea and pneumonia (3%), and pneumonia alone (2.5%).
The most affected age group was less than one year of age (194/10,000) followed by the 1-4 years age group (47/10,0000), and 5-15 years (2/10,000). The AR was similar among males (20/10,000) and females (18/10,000). The most affected Sub-counties were Lotisan (50/10,000) and Rupa (41/10,000). These were followed by Nandunget (17/10,000), Northern Division (14/10,000), Loputuk (13/10,000), Katikekile (9/10,000), Southern Division (7/10,000), and Tapac (1/10,000) sub-counties. The overall AR was 19/10,000.
Hypothesis generation and case control study findings
Of the 30 cases interviewed: 25 (83%) were not vaccinated; 19 (63%) had visited a health facility, eight (27%) were malnourished, 2 (7%) had a visitor from a neighboring district.
Interviews with the district health officer, and district surveillance focal person (DSFP) revealed that there was frequent movement across the Ugandan border with Kenya and they had been on high alert since the beginning of the year following information from their Kenyan counterparts about a measles outbreak that was ongoing in the Western Turkana Region.
Table 1: Factors associated with measles transmission during the outbreak in Moroto District, Uganda, March–July 2024
Moroto District, Uganda, March–July 2024
| Risk factor | Cases
n (%) |
Controls
n (%) |
Crude OR
(95% CI) |
aOR
(95%CI) |
| Vaccination | ||||
| Yes | 22 (50) | 111 (91) | 0.099 (0.04 – 0.26) | 0.11 (0.03–0.4) |
| No | 22 (50) | 11 (9) | Ref | Ref |
| Malnutrition | ||||
| Yes | 24 (29) | 24 (15) | 2.4 (1.3 – 4.6) | 6.1 (1.3 – 27) |
| No | 59 (71) | 142 (85) | Ref | Ref |
| Visiting a health facility | ||||
| Yes | 37 (45) | 14 (18) | 3.6 (1.7 – 7.7) | 3.8 (1.3 – 11) |
| No | 46 (55) | 63 (82) | Ref | Ref |
| Visitor from another district | ||||
| Yes | 11 (13) | 9 (5) | 2.7 (1.1 – 6.8) | 3.9 (0.3 – 53) |
| No | 72 (87) | 157 (95) | Ref | Ref |
| Vitamin A in the last 6 months | ||||
| Yes | 69 (83) | 153 (92) | 0.42 (0.19 – 0.95) | 0.5 (0.1–3.0) |
| No | 14 (17) | 13 (8) | Ref | Ref |
Vaccination (aOR=0.11, 95%CI=0.03–0.4), malnutrition (aOR=6.1, 95%CI=1.3–27), and visiting a health facility 7–21 days prior to onset of rash (aOR=3.8, 95%CI=1.3–11) were significantly associated with measles transmission (Table 1).
Vaccine coverage and vaccine effectiveness estimation findings
The estimated VE was 89% (95% CI= 60 – 97). The estimated VC, based on the percent of controls that had a history of being vaccinated against measles, was 91% among those ≥ 9 months of age and 67% overall for MCV1.
Discussion
Our investigation revealed that the outbreak was most likely introduced into the area from the Western part of Kenya; Turkana that neighbours the outbreak area and had been experiencing a large measles outbreak. Low measles vaccination coverage coupled with malnutrition and nosocomial spread propagated the outbreak. Rupa and Lotisan sub-counties were the most affected sub-counties.
This measles outbreak was likely introduced in Moroto through cross border importation from the Western Turkana Region that had been experiencing a measles outbreak since December 2023 (11). Both communities are nomadic pastoralists and there are frequent movements across the border for cultural and grazing reasons. Improving cross border information sharing at district and regional levels, and improved surveillance at border points can mitigate future spread of diseases by cross border movements (12).
The outbreak was further facilitated by mixing of measles and non-measles patients prior to the confirmation of the outbreak and the designation of an isolation unit at Moroto RRH. Nosocomial spread of measles has previously been found to propagate outbreaks in Uganda and elsewhere (8, 16, 17). The WHO recommends that individuals with rash and fever should not share common waiting areas at health facilities (15).
Malnutrition which was common in this outbreak area was associated with increased odds of measles infection. Studies in Afar District of North Eastern Ethiopia and Yemen found similar findings with malnutrition increasing the odds of measles disease(19, 20). This area had been experiencing an increase in acute food insecurity and malnutrition levels during the period of the outbreak (18).
In this study, history of measles vaccination was protective against measles disease. Measles vaccination is the recommended strategy for preventing measles outbreaks worldwide and subsequently achieving elimination. The WHO recommends two doses of MCV with the first dose administered at 9 months and the second dose at 15 – 18 months of age, and a VC of at least 80% for MCV2 (1). The estimated VE during this investigation for MCV1 was 89% which was higher than in a previous study of 85% (19), but lower than in another study in Uganda that found 95% VE but within the range of findings of systematic review of measles VE to be between 77%, IQR (62 – 91 %) . VE findings from the field vary and depend on the number of doses administered, vaccine handling and storage, cold chain failure and host factors such as malnutrition and HIV infection (20).
Study limitations
This investigation had some limitations. There was ongoing insecurity in the most affected communities of Lotisan and Rupa Sub-counties of the district during this outbreak (20). We could not access the insecure sub-counties for comprehensive case finding and investigations. This could have led to underestimation of the magnitude of the outbreak. Additionally, it is likely that we interviewed only severe cases who were more likely to seek care. Because of the insecurity, we enrolled hospital controls, this possibility likely introduced a misclassification bias. The bias was minimized by careful selection of the controls and only considering those without symptoms of measles and with a diagnosis other than measles made by either a pediatrician or a medical officer at the hospital.
Recommendations and public health actions
During the investigation, mass MCV campaign was conducted targeting children aged 6 months to 5 years in all the sub counties and divisions of Moroto district. Outreaches for vaccination were also extended to underserved and insecure areas with the support of the security forces in the district. Screening at all points of care for children was done and isolating suspected measles cases, an isolation and treatment wards were designated at Moroto RRH and St. Pius Kidepo HC III. We also participated in provision of relief food at the lowest administrative units coupled with screening for measles to prevent malnutrition and also avoid further spread of measles and reduce measles associated mortality.
To prevent and control future outbreaks, we recommended strengthening and supporting routine vaccination program; a policy shift in the national immunization schedule for the MCV1 to be administered at six months of age; integrating animal and human vaccination programs to improve on the vaccination coverage in this nomadic population and improved cross border information sharing at district level and enhancing cross border surveillance.
Conclusion
This measles outbreak was imported from the Western Turkana Region of Kenya to Moroto District, Karamoja Region through cross border movement by the nomadic people who live in both regions. The outbreak was propagated by interaction of cases with other children seeking care at different health facilities through nosocomial transmission. Malnutrition and low measles vaccination rates in the area further facilitated the outbreak.
Conflict of interest
The authors declared no conflict of interest
Author contribution
All authors contributed to the write-up and review of the bulletin. EM wrote the drafts of the bulletin and revised the bulletin for substantial intellectual content. DW, AN, DS, EK, RA, and RM participated in the investigation. RM, BK, and ARA were involved in the review of the bulletin for substantial intellectual content. RM participated in the supervision of field data collection and reviewed the draft bulletin for substantial intellectual content.
Acknowledgements
We acknowledge the support of the Moroto District local government and Karamoja Regional Emergency Operations Centre (EOC) who worked with us during this outbreak investigation and response for their cooperation. We thank the frontline health workers, whom we worked with during case finding, implementation of public health actions, and enrollment of controls for their time, support and cooperation. We also acknowledge the Ministry of Health through Uganda National Expanded Program for Immunization (UNEPI) for the logistical and technical support to the outbreak response especially the mass measles campaign.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO. Measles vaccines: WHO position paper, April 2017 – Recommendations. Vaccine. 2019 Jan 7;37(2):219–22.
- Measles [Internet]. [cited 2024 Jul 15]. Available from: https://www.who.int/news-room/fact-sheets/detail/measles
- Minta AA. Progress Toward Measles Elimination — Worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep [Internet]. 2023 [cited 2024 Jul 15];72. Available from: https://www.cdc.gov/mmwr/volumes/72/wr/mm7246a3.htm
- WHO U. WHO and UNICEF estimates of immunization coverage [Internet]. 2024 Jul. Available from: https://data.unicef.org/wp-content/uploads/cp/immunisation/uga.pdf
- Majwala RK, Nakiire L, Kadobera D, Ario AR, Kusiima J, Atuhairwe JA, et al. Measles outbreak propagated by children congregating at water collection points in Mayuge District, eastern Uganda, July – October, 2016. BMC Infect Dis. 2018 Aug 20;18(1):412.
- Biribawa C, Atuhairwe JA, Bulage L, Okethwangu DO, Kwesiga B, Ario AR, et al. Measles outbreak amplified in a pediatric ward: Lyantonde District, Uganda, August 2017. BMC Infect Dis. 2020 Jun 5;20(1):398.
- Walekhwa AW, Ntaro M, Kawungezi PC, Achangwa C, Muhindo R, Baguma E, et al. Measles outbreak in Western Uganda: a case-control study. BMC Infect Dis. 2021 Jun 22;21(1):596.
- Investigation of a Measles Outbreak in Semuto Subcounty, Nakaseke District, Uganda, June–August 2021 – UNIPH [Internet]. 2022 [cited 2024 Jul 15]. Available from: https://uniph.go.ug/investigation-of-a-measles-outbreak-in-semuto-subcounty-nakaseke-district-uganda-june-august-2021/
- WHO | Regional Office for Africa [Internet]. 2024 [cited 2024 Jul 15]. Weekly bulletins on outbreaks and other emergencies. Available from: https://www.afro.who.int/health-topics/disease-outbreaks/outbreaks-and-other-emergencies-updates
- Emerging and reemerging epidemic-prone diseases among settling nomadic pastoralists in Uganda. Acta Tropica. 2014 Sep 1;137:19–24.
- WHO Afro. OMS | Escritório Regional para a África. 2024 [cited 2024 Jul 16]. Outbreak and other Emergencies: Week 23: 3 – 9 June 2024. Available from: https://www.afro.who.int/countries/kenya/publication/outbreak-and-other-emergencies-week-23-3-9-june-2024
- Akinloluwa OO, Lokossou V, Okatubo G, Okunromade O, Nwitte-Eze O, Alabi S, et al. Towards a multi-lateral framework for cross-border surveillance and information sharing between Nigeria and neighbouring countries. BMJ Global Health. 2024 Mar 1;9(3):e013011.
- Nosocomial transmission of measles: An updated review. Vaccine. 2012 Jun 8;30(27):3996–4001.
- Farizo: Pediatric emergency room visits: a risk factor… – Google Scholar [Internet]. [cited 2024 Jul 19]. Available from: https://scholar.google.com/scholar_lookup?&title=Pediatric%20emergency%20room%20visits%3A%20a%20risk%20factor%20for%20acquiring%20measles&journal=Pediatrics&volume=87&issue=1&pages=74-79&publication_year=1991&author=Farizo%2CKM&author=Stehr-Green%2CPA&author=Simpson%2CDM&author=Markowitz%2CLE
- Biellik RJ, Clements CJ. Strategies for minimizing nosocomial measles transmission. Bull World Health Organ. 1997;75(4):367–75.
- Ayele WM. Malnutrition Precipitated Measles Outbreak in Gewane District, Afar Regional State, Northeastern Ethiopia, 2016 [Internet]. 2020 [cited 2024 Jul 19]. Available from: https://www.researchsquare.com/article/rs-32423/v1
- Nassar AAH, Al Amad MA, Qasim M, Dureab F. Risk factors for measles outbreak in Ataq and Habban districts, Shabwah governorate, Yemen, February to May 2018. BMC Infect Dis. 2021 Jun 10;21(1):551.
- Uganda – Karamoja, IPC Acute Food Insecurity and Acute Malnutrition Analysis, March 2024 – February 2025 (Issued 12 June 2024) – Uganda | ReliefWeb [Internet]. 2024 [cited 2024 Jul 19]. Available from: https://reliefweb.int/report/uganda/uganda-karamoja-ipc-acute-food-insecurity-and-acute-malnutrition-analysis-march-2024-february-2025-issued-12-june-2024
- Namulondo E, Ssemanda I, Komugisha M, Nuwamanya Y, Nsubuga EJ, Wako S, et al. Measles Outbreak in a Refugee Settlement, Kiryandongo District, Uganda, July– October 2023 [Internet]. 2024 [cited 2024 Jul 19]. Available from: https://www.researchsquare.com/article/rs-4497006/v1
- Oyel R. Nilepost News. 2024 [cited 2024 Jul 19]. Death toll in Moroto warrior attacks increases to 11. Available from: https://nilepost.co.ug/crime/206192/death-toll-in-moroto-warrior-attacks-increases-to-11


Comments are closed.