Laboratory response to an acute conjunctivitis outbreak, Uganda Prisons Luzira, Kampala, Uganda March, 2024
Authors: 1,2Wilfred Opeli, 1,3Anne Martha Nankya, 4Alisen Ayitewala, 2Moses Kisakye, 5Emma Amalai, 5Javis Tumwesige, 6Bryn Odaga, 7Richard Walwema, 1,8Esther Nabatta, 1,9Ronald Samuel Lugwana, 1,4Ritah Namusoosa, 1,3Tracy Rutogire, 1,10Winnie Agwang, 1Hannington Katumba, 1Charity Mutesi, 1Emmanuel Mfitunda, 1Owens Joyce Kobusingye, 1Daniel Wenani, 1Loryndah Olive Namakula, 1Emmanuel Okiror Okello, 1Janet Lubega Kobusinge, 1Getrude Abbo, 1Annet Mary Namusisi, 1Briget Ainembabazi 1Patrick Kwizera, 1Joshua Kayiwa, 1Milton Wetaka, 3Stephen Balinandi, 3John Kayiwa, 3Rebecca Nakidde, 3Ibrahim Mugerwa, 3Grace Najjuka, 3Isaac Ssewanyana, 3Atek Kagirita, 3Susan Nabadda, 1Samuel Gidudu and 1Alex Riolexus Ario Institutional affiliations 1Uganda National Institute of Public Health, Ministry of Health, Kampala, 2Uganda Prisons Services, Kampala, Uganda, 3Uganda Virus Research Institute, Ministry of Health, Entebbe, Wakiso, 4National Health Laboratory and Diagnostics Services, Ministry of Health, Kampala, Uganda, 5Kampala Capital City Authority, Kampala, Uganda, 6Kampala Metropolitan Area Public Health Emergency Operations Centre, Kampala, Uganda, 7Infectious Disease Institute of Uganda, Kampala, Uganda, 8National Animal Disease Diagnostics and Epidemiology Center, MAAIF, Entebbe, Wakiso, 9Mengo Hospital, Kampala, Uganda, 10Baylor College of Medicine Children’s Foundation, Kampala, Uganda, Correspondence: Tel: +256773229025, Email: wopeli@uniph.go.ug
Summary
Background: In March 2024, Kampala Capital City Authority (KCCA) and Ministry of Health Uganda (MOH) reported a suspected outbreak of conjunctivitis (red eye) in Uganda Prisons, Luzira. On March 12, 2024, the Ministry of Health (MOH) deployed a multi-disciplinary team to support the Uganda Prisons Service (UPS) respond to the conjunctivitis outbreak. The Laboratory Leadership Track supported the UPS in coordinating laboratory activities; mentor staff, monitoring sample collection, referral, tracking and receipt of results. We suggested recommendations to strengthen laboratory systems for any future outbreak responses.
Methods: We had meetings with prisons’ management. We assessed capacity of UPS laboratories in Luzira to conduct the outbreak investigation and conducted mentorships, coordinated the collection tracking of samples, referral and relay of test results for timely public intervention and patient management.
Results: The Luzira laboratory testing capacity was identified to be at 43%, below the 80% WHO target. The prisons laboratory team collected and referred a total of 116 eye swab samples from 56 suspected cases. The turnaround time (TAT) from sample collection to pick up and result dispatch was within 1 and 7 days respectively for samples referred. Sample results from Uganda Virus Research Institute (UVRI)
identified enterovirus C as the causative agent for the conjunctivitis outbreak in UPS Luzira.
Conclusion: The UPS laboratory and response team ably responded to the conjunctivitis outbreak. Stakeholders were identified and engaged in coordinating laboratory activities from sample collection to receipt of results. However, a need to build laboratory testing capacity for any future outbreak response is recommended.
Background
Conjunctivitis is an infection characterized by a red eye with any or all of the following symptoms; swelling, itching, tearing, irritation and sticky discharge of the eyes whose lids may be stuck together by a mucopurulent exudate on awakening (1). The cause of conjunctivitis infection can either be bacteria, viruses, fungal or an allergic reaction.
Conjunctivitis in a closed setting like prisons is declared when there is a rapid increase in cases especially when they are clustered by time and location and if there is evidence of transmission from person to person (5). The Uganda Prison Services on the 7th of March 2024 notified the Kampala Capital City Authority (KCCA) of a possible outbreak of conjunctivitis (red eye infection) in Kampala Remand prisons with 314 suspects registered. On the 12th of March, 2024, the MOH deployed a multi-disciplinary team of national rapid responders (laboratory leaders and field epidemiologists) to support UPS response to the conjunctivitis outbreak. The source of the infection for Luzira prisons was reported to be Makindye police station, with the initial index case originating from Nabutiti zone, Kansanga, Makindye division. In addition to prisons, schools in Nakawa and Rubaga divisions of Kampala district also registered suspected cases of conjunctivitis.
We identified key stakeholders and partners to offer technical and logistical support to the conjunctivitis outbreak response. We also sought to assess and build the capacity of the Uganda Prisons laboratories in Luzira in coordinating the conjunctivitis outbreak response by mentoring laboratory staff monitoring on sample collection, referral, transportation, receipt at referral testing laboratory and time of return of results to the referring laboratory. We suggested recommendations for future laboratory interventions during an outbreak response based on their findings.
Methods
The Outbreak occurred at the four prison units under the Kampala Extra Region (KER), namely: Murchison Bay, Kampala Remand, Luzira Upper and Luzira Women prisons. The KER is one of 16 Regional Prisons in the Uganda Prisons Service located approximately 6 km east of Kampala Capital City Centre with a population of 8,098 inmates and 13,897 staff, family, and neighboring community. KER has 5 health facilities with laboratories; Murchison Bay Hospital, Luzira staff clinic HC IV, Kampala Remand Prison HC III, Luzira Upper Maximum Prison HCIII and Luzira Women Prison HC III.
We identified partners and stakeholders in this response that would support the laboratory outbreak response investigation. We defined their roles and responsibilities according to the needs found at the prison laboratory.
We assessed the capacity of Luzira prison laboratories to coordinate laboratory response activities using the WHO laboratory assessment tool, 2012.
Luzira staff clinic HCIV was the sample collection hub and national sample transport system was used to refer samples to the testing laboratories. Together with partners, we mobilized sample collection materials. Two or three samples were collected from each suspected case depending on sample adequacy and tests to be performed. Samples were collected and transported to the National Microbiology Reference Laboratory (NMRL) at the National Health Laboratory and Diagnostic Services (NHLDS) for testing.
This investigation was in response to the conjunctivitis outbreak in Uganda Prisons. The office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not a human subject research and its primary intent was for disease control. Permission was obtained from the Uganda Prisons authorities to access the facilities and inmates. Verbal consent was sought from all participants and their identities kept private by use of codes and no personal identifiers. Participation was voluntary and without coercion and no penalties imposed for refusal.
Result
Partners and stakeholders identified to participate in the laboratory response
We identified two reference laboratories (Uganda National Health Laboratory and Diagnostic Services and Uganda Virus Research Institute) which were charged with transportation and testing of samples collected from the outbreak response area. Other partners include the Luzira prisons clinical and surveillance team and National Medical Stores. Stakeholders identified included Baylor College of Medicine – Uganda and Infectious Disease Institute that supported the outbreak response with development of conjunctivitis outbreak response guidelines, logistical and technical support.
Laboratory capacity assessment and capacity building
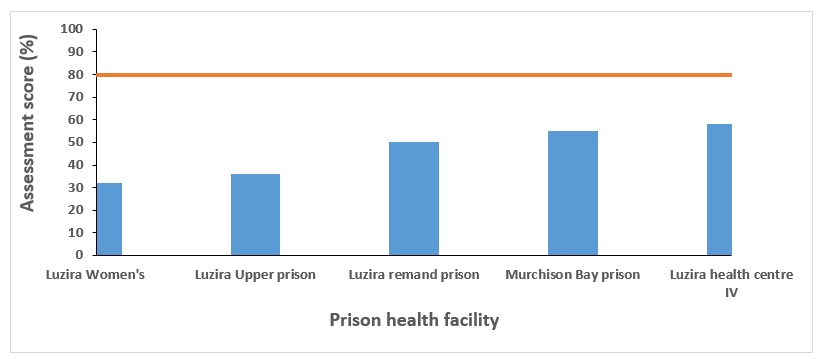
The Uganda prison Luzira laboratory’s capacity to respond to the red eye outbreak was at an average of 43% which is below the recommended 80 (Figure 1).
All key functions assessed were below the required 80% target.. Scores below 50% required immediate interventions; sample management, response management, data management, lab surveillance, supply availability, bio-risk management and testing capacity (Figure 2).
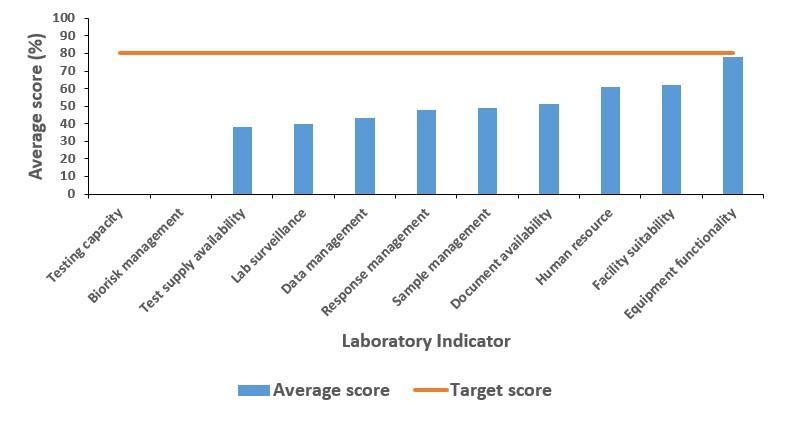
Based on the assessment results, we facilitated the development of sample and logistics trackers, and carried out staff mentorship on sample collection, packaging and transportation, laboratory data and logistics management. Twelve laboratory personnel and 1 ophthalmic officer were mentored.
Sample collection, transportation, and testing
As of 26th, March 2024, 116 samples were collected from 59 suspected cases. All samples collected were transported within 24 hours after collection to the NHLDS and UVRI reference laboratories.
Enterovirus C nucleic acid was confirmed present in four patients with red eyes in Murchison Bay (3) and Kampala Remand prisons (1).
Discussion
This investigation of conjunctivitis in a Uganda prisons highlighted and provided critical insights into laboratory capacity for infectious disease outbreak preparedness and response in a closed setting. The investigation found the UPS Luzira laboratory capacity at 43% which is below the 80% WHO recommendation indicating a low capacity to adequately respond to the conjunctivitis outbreak.
Laboratory infrastructure, supply shortages and the lack of bio-safety/biosecurity measures were some of the major challenges identified during the outbreak response. Given that the institution has adequate laboratory staffing, it’s essential that the facilities are supplied and equipped so as to be able to provide baseline investigations such as gram staining for screening purposes. There is also need to put in place biosafety/biosecurity measures for infection, prevention and control purposes.
It is important to maintain a proper laboratory data management system for effective infectious disease surveillance. This not only helps in the monitoring of disease trends and patterns but also helps in early case detection and follow-up. Though the prisons health system was able to detect the conjunctivitis outbreak early, there was poor record keeping and documentation of suspected cases.
There was generally a lack of a preparedness and response plan aimed at addressing any eventual infectious disease outbreak. A functional system designed to forecast and respond to a public health emergency ensures resource availability, active surveillance, data management, adequate supplies, equipment functionality, testing capacity and a well oriented laboratory work force for any eventual outbreaks in peace time.
The laboratory capacity at Luzira prisons to conduct screening tests like Gram staining technique was limited and lacked a basic microbiology section to perform culture tests.
Study limitations
The findings of this conjunctivitis outbreak response cannot be generalized to the other up country prisons units and national situation given its limited coverage area, environmental and short intervention period.
Conclusions
The laboratory response team assessed the capacity of the Luzira prisons laboratory to respond to the conjunctivitis outbreak and with the support of reference laboratory’s identified Enterococcus type C virus as the causative agent which helped inform public health interventions.
Recommendations
We recommend that the Prisons Health authority develop of a laboratory outbreak response plan and carry out regular training of laboratory staff in outbreak response preparation and response, biosafety and bio-risk management.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgements
We are grateful to the administration of Uganda Prisons Service for allowing us carry out this intervention. We also thank Baylor Uganda and Infectious Disease Institute for their technical and logistical support and Centers for Disease Control and Prevention – Uganda, Makerere University School of Public Health and Uganda National Institute of Public Health for the financial and technical Support.
Copy right and license
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Azari AA, Arabi A. Conjunctivitis: a systematic review. Journal of ophthalmic & vision research. 2020;15(3):372.
- Yeu E, Hauswirth S. A review of the differential diagnosis of acute infectious conjunctivitis: implications for treatment and management. Clinical Ophthalmology. 2020:805-13.
- Kowalski RP, Nayyar SV, Romanowski EG, Shanks RM, Mammen A, Dhaliwal DK, et al. The prevalence of bacteria, fungi, viruses, and acanthamoeba from 3,004 cases of keratitis, endophthalmitis, and conjunctivitis. Eye & contact lens. 2020;46(5):265-8.
- Johnson D, Liu D, Simel D. Does this patient with acute infectious conjunctivitis have a bacterial infection?: The rational clinical examination systematic review. JAMA. 2022;327(22):2231-7.
- Kaur G, Seitzman GD, Lietman TM, McLeod SD, Porco TC, Doan T, et al. Keeping an eye on pink eye: a global conjunctivitis outbreak expert survey. International Health. 2022;14(5):542-4.


Comments are closed.