Investigation of an Outbreak of Acute Haemorrhagic Conjunctivitis at School X in Kampala City, March 2024
Authors: Dorothy Aanyu1*, Tracy Rutogire1, Benon Kwesigwa1, Richard Migisha1, Alex Ndyabakira2, Sarah Karen Zalwango2, Daniel Ayen Okello2, Lilian Bulage1, Alex Riolexus Ario1 : Institution affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda National Institute of Public Health, Kampala, Uganda; 2 Kampala Capital City Authority, Kampala, Uganda : Correspondence*: Tel: +256774009185, Email: daanyu@uniph.go.ug
Summary
Background: On March 11, 2024, Kampala Capital City Authority received an alert of increase in the number acute haemorrhagic conjunctivitis (AHC) cases at an infant School X in Kampala City. We investigated the outbreak to determine the scope, identify factors associated with its spread, and recommend control and prevention measures.
Methods: We defined a case as redness of one or both eyes and any of the following: tearing, swelling, itching, discharge in a pupil or staff of school X from March 5-31, 2024. We identified cases by reviewing health records at the school. We calculated attack rates (AR) by ages, sex, class, and dormitory using staff and pupils of the infant school as source population. We also conducted staff interviews and an environmental assessment. We conducted an unmatched case-control study. We defined a control as a pupil or staff of school X who had not had AHC from March 05 to March 31, 2024. We identified factors associated with the spread of AHC in the school using logistic regression.
Results: We found 175 cases, 167 of whom were pupils and 8 were staff. The mean age for case-patients was 11.4 years (range 5–45 years). Attack rates (%) were similar in females and males (10 vs 8.4). Pupils in the boarding section were more affected than day scholars (AR:23) with residents of Alpha dormitory more affected than other dormitories (AR:50). Pupils in P4-P7 were the most affected compared to lower class groups (AR:17). We found that being a boarding scholar (aOR=10, 95%CI: 2.1-51) increased the odds of AHC. Persons who washed their hands at arrival back at the dormitory/home (aOR= 0.38, 95%CI: 0.16-0.91) and pupils in classes P4-P7 (aOR= 0.34 95%CI: 0.14-0.77) were protected against AHC. We observed that most dormitories were congested with pupils sleeping in triple decker beds, some adjacent beds had no space separating them. Hand washing facilities were also not well distributed.
Conclusion: The outbreak was likely facilitated by dormitory congestion and poor hand hygiene practices. Boarding scholars were most affected; regular hand washing and attending upper classes were protective. Education and awareness of good hand hygiene measures could mitigate the risk of similar outbreaks in the future.
Background
Conjunctivitis, commonly known as “AHC” or “pink eye”, is an inflammation of the conjunctiva, the transparent membrane that lines the eyelid and eyeball. It can be caused by a bacterial or viral infection, allergies or can be toxin- induced. Viral conjunctivitis followed by bacterial conjunctivitis is the most common cause of contagious conjunctivitis, while allergic and toxin-induced conjunctivitis are non-contagious (1).
Diagnosis of AHC is usually made on the basis of clinical presentation and patient history. A mucopurulent discharge is often associated with bacterial AHC while watery discharge has been more consistent with viral conjunctivitis (4). The common pathogens for bacterial conjunctivitis are Staphylococcus species followed by Streptococcus pneumoniae and Haemophilus influenzae. Bacterial conjunctivitis is more common in children than in adults (3).
Viral conjunctivitis accounts for up to 75% of acute conjunctivitis cases. Adenoviruses followed by Enteroviruses and Coxsackieviruses are the most commonly isolated causative agent of acute haemorrhagic conjunctivitis (AHC). AHC is characterized by inflammation, reddening and swelling of the conjunctiva, itching, increased tear production, feeling like a foreign body is in the eye, crusting of eyelids or lashes, and discharge (5). The incubation time is 1-3 days from the exposure to the infection. Common complications include photophobia, blurred vision, and severe headaches. It spreads from person to person through contaminated hands and through sharing contaminated personal items such as clothing, towels, and accessories like sunglasses and eye makeup (4,6).
On March 11, 2024 Kampala Capital City Emergency Operations Centre received an alert from school X in Kampala City. It stated that several learners were ill with AHC and requested for help in managing the outbreak. We investigated to determine the scope of the outbreak, identify factors associated with its spread, and to recommend control and prevention measures.
Methods
Outbreak area
This outbreak occurred at school X in Kampala City. School X is a mixed day and boarding nursery and primary school with approximately 1,800 learners, 700 of whom were in the boarding section. The school also had 148 staff consisting of teachers, matrons, medical, and security personnel.
At the time of the outbreak notification, Kampala City was experiencing an outbreak of AHC, and more than 1,000 cases had been reported in prisons and communities all over the city. No school had reported any cases to local authorities at the time.
Case definition and finding
We defined a suspected case as redness of one or both eyes and any of the following: tearing, swelling, itching, discharge in a pupil or staff of school X from March 5-31, 2024. A confirmed case was suspected case with a positive result on bacterial culture in ocular swab specimens from a pupil or staff of school X from March 05- 31, 2024. To find cases, we reviewed records from the school sick bay. For each case-patient line listed, we conducted follow-up interviews with the school nurse and child on presentation of symptoms, treatment, and possible linkage. We then created a line list of all cases meeting the case definition capturing variables such as dates of symptom onset, demographic characteristics, and symptoms.
Descriptive epidemiology
We described the cases by age, class group, dormitory of residence and section of study (day or boarding) and calculated attack rates for each to determine the scope of the outbreak. To describe the outbreak in terms of time, we constructed an epi-curve.
Laboratory investigations
To identify the causative pathogen, we collected ocular swabs for microbiological evaluation from six AHC case-patients that had not initiated antimicrobial therapy. Laboratory testing was carried out at Central Public Health Laboratories (CPHL).
Environmental assessment
To identify factors that could have been be associated with the introduction and spread AHC into School X we assessed the set-up of the dormitory facilities, play area, classrooms and handwashing facilities in School X.
Hypothesis generation interviews
In order to identify risk factors for AHC, we conducted 50 hypothesis generating interviews. We interviewed case-patients about potential risk factors for AHC transmission occurring three days before onset of symptoms. These included history and nature of contact with a symptomatic case, handwashing measure, and contact with a person from outside the school.
Case-control study
To evaluate the exposures that emerged during hypothesis generation, we conducted an unmatched case-control study comparing exposures of 175 cases to an equal number of randomly selected controls. We defined a control as a pupil or staff of School X with no history of AHC from March 05 to March 31, 2024. We administered an electronic questionnaire to both cases and controls to assess exposure and outcomes of interest. For the reported hand hygiene practices, all responses falling at “sometimes” or “never” were considered non-performers of the practice and were assigned a “no” response, while those responses at “always” or “most of the time” were performers of the practices and were assigned “yes” response. We identified risk factors for transmission using logistic regression.
Ethical considerations
This investigation was in response to a public health emergency and was therefore determined to be non-research by the office of the Center for Global Health, US Center for Disease Control and Prevention. Kampala Capital City Authority (KCCA) gave permission to investigate this outbreak. Permission to conduct the investigation was obtained from the school X administration and assent was also obtained from the underage respondents. All child case-patient interviews were conducted with a staff member present. In collaboration with KCCA, we linked school X medical team to a consultant ophthalmologist to guide them on appropriate case management for the affected case-patients.
Results
Descriptive epidemiology
We identified 175 suspected cases in this outbreak, 167 of whom were pupils and 8 were staff. There were no confirmed cases nor fatalities. The average age of case-patients was 11.4 years (SD=5.1, range, 5–45 years). Both sexes were similarly affected, attack rate (AR) of 10% in females vs 8.4% in males (Table 1). By class group, pupils in P4-P7 were the most affected with AR of 17%. Pupils in the boarding section were more affected than day scholars (AR 23% vs 0.37%). All five dormitories registered cases but pupils residing in boys dormitory Alpha were most affected (AR: 50%) followed by pupils in girl’s dormitory Omega (AR:33%).
Table 1: Attack rates by pupil characteristics at school X, during an outbreak of acute haemorrhagic conjunctivitis, Kampala City, March 2024 (n=175)
| Variable | Category | Cases | Population | Attack rate (%) |
| Sex | Female | 99 | 975 | 10 |
| Male | 76 | 909 | 8.4 | |
| Level | Pre-primary | 2 | 438 | 0.5 |
| P1-P3 | 23 | 622 | 3.7 | |
| P4-P7 | 142 | 824 | 17 | |
| Staff | 8 | 148 | 5.4 | |
| Section | Boarding | 165 | 708 | 23 |
| Day | 2 | 1176 | 0.34 | |
| Dormitories | Alpha | 33 | 66 | 50 |
| Omega | 65 | 193 | 34 | |
| Delta | 29 | 134 | 22 | |
| Beta | 33 | 231 | 14 | |
| Gamma | 5 | 84 | 6.0 | |
| Teachers quarters | 8 | 148 | 5.4 |
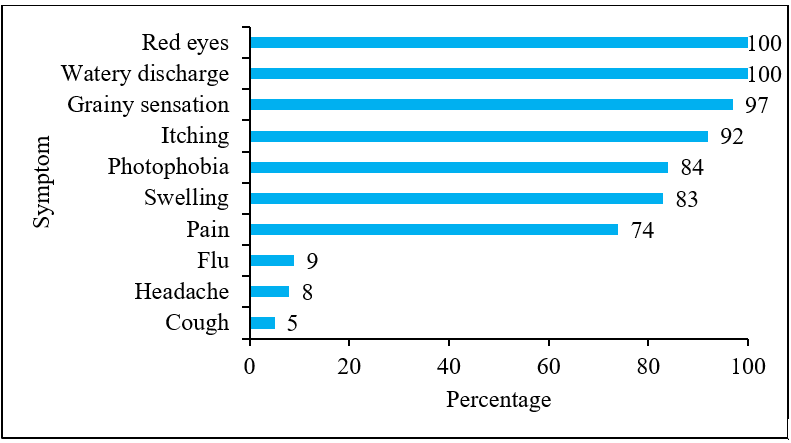
All case-patients had red eyes (100%) and a watery eye discharge (Figure 1). Other common eye symptoms were grainy sensation (97%), itching (92%) photophobia (84%), swelling (83%), and pain (74%). Some case-patients also experienced non eye symptoms like flu (9%), headache (8%), and cough (5%).
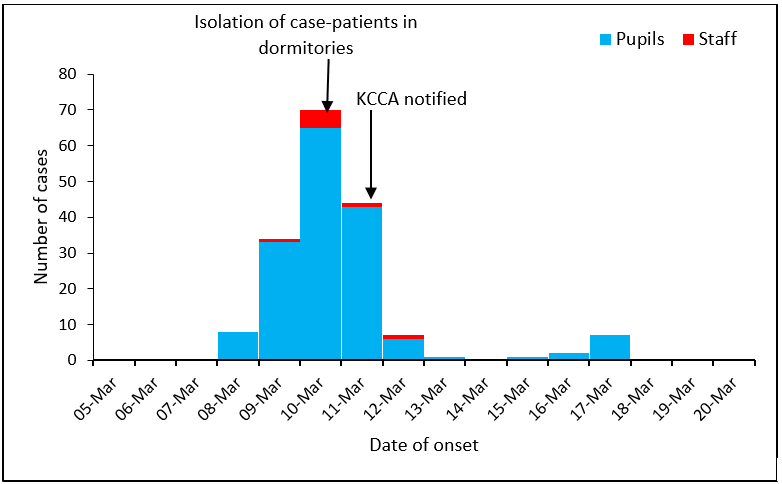
The epidemic curve suggested a propagated outbreak (Figure 2). Eight pupils at the school X. developed irritating eye symptoms on March 08, 2024. They were all male and all resided from the same dormitory. Two days later on March 10, more than 70 new cases were registered forming the first generation of cases. On March 11, 2024 KCCA Emergency Operations Centre was notified of the outbreak at the school. A second generation of cases started on March 15, rising to a small peak on March 17 and thereafter no new cases were recorded at school X.
Laboratory investigation
No organisms were observed after gram staining. No bacterial growth was observed when the swabs were subjected to culture and sensitivity testing.
Environmental assessment
Screening: At the time of the investigation, all visitors were screened at the main school entrance and one with symptoms of AHC was not allowed to access the school. We found that there was generally regulated movement of persons to and from either the classes or dormitories.
Classrooms: The school had four classrooms for each class/level and there were 50 pupils in each stream. In the classrooms, pupils sat in pairs assigned by the class teacher. The school had an open area where the children would play from during the breaktime. There were no toys or playground equipment.
Dormitories: All the dormitories were within the school perimeter except boys dormitory Alpha. Alpha was outside the school wall, about 100 meters away. The school thus employed a private security firm to guard the dormitory in the evenings and weekends. All the other dormitories did not have guards assigned.
We observed that most of the dormitories were congested. Pupils slept in triple bunk beds with half a meter separation in between. Beds were lined up to the wall and some adjacent beds had no space separating them. The pupils used their own towels and toiletries, but sometimes shared soap with others. Personal hygiene practices like bathing and brushing happened in a public bathing area. The matrons personally took more care of the younger children, ensuring they had bathed and brushed their teeth well enough and older children were randomly inspected as they exited the dormitories to go to class for the day. We found out that in the early days of the outbreak, there was mixing of AHC case-patients and other non-ill pupils in the dormitories. The matrons reported that due to congested settings, it was hard to enforce isolation in the dormitories. But from March 10, 2024 they had come up with a strategy to reduce interaction between case-patients and their non-ill counterparts by enforcing an earlier bedtime for the case-patients.
Handwashing: Handwashing stations were placed at major school entrances and at class room blocks. The stations were pedal step activated and the contained a mild soap mixture. Dormitories did not have handwashing stations at the entrance.
We interviewed cases and controls on their hygiene practices. All reported washing their faces every morning. All practiced handwashing with soap and water before and after meals and after using the toilet.
Hypothesis generation findings
Our hypothesis generation interviews revealed that 92% had contact with a symptomatic case-patient, 63% washed their hands regularly, 2% shared personal items such as towels and handkerchiefs with a case-patient. Based on the descriptive epidemiology and hypothesis generation findings, we thus hypothesized that close contact with a case and poor hand hygiene practices were the potential exposures for this outbreak.
Case-control study
We enrolled 175 controls for the case-control study. In our bivariate analysis, contact will an ill person, being a boarding scholar, class group and handwashing were associated with AHC. We did not find statistically significant association between sex and age with AHC (Table 2). At the multivariate analysis stage, being a boarding scholar (aOR=10, 95%CI:2.1-51) increased the odds of AHC. Persons who washed their hands at arrival back at the dormitory/home (aOR=0.38, 95%CI:0.16-0.91) and pupils in classes P4-P7 (aOR=0.34 95%CI:0.14-0.77) were protected against AHC.
Table 2: Factors associated with acute haemorrhagic conjunctivitis at School X, Kampala City, March 2024
| Category | Cases n(%) | Controls n (%) | COR (95%CI) | aOR (95%CI) |
| Contact with ill person | ||||
| No | 9 (5) | 22 (13) | Ref | |
| Yes | 166 (95) | 153 (87) | 2.7 (1.2-5.9) | 1.7 (0.7-4.5) |
| How they interact | ||||
| Share a decker | 12 (7.2) | 3 (2) | Ref | |
| Play together | 120 (72) | 143 (93) | 4.7 (1.31-17) | |
| Share personal items | 4 (2.4) | 0 (0) |
0.4 (0.017-9.3) |
|
| Share stationary | 14 (8.4) | 0 (0) | 0.12 (0.006-2.6) | |
| Others | 16 (10) | 7 (5) | 1.8 (0.37-8.2) | |
| Sex | ||||
| Female | 99 (57) | 106 (60) | Ref | |
| Male | 76 (43) | 69 (40) | 1.18 (0.77-1.8) | |
| Section | ||||
| Day | 2 (1) | 17 (10) | ref | |
| Boarding | 165 (99) | 151 (90) | 9.3 (2.12-41) | 10 (2.1-51) |
| Class group | ||||
| Pre-P3 | 25 (15) | 13 (8) | ref | |
| P4-P7 | 142 (85) | 155 (92) | 0.48 (0.24-0.97) | 0.34 (0.14-0.77) |
| Age group | ||||
| 0-10 | 70 (40) | 70 (40) | Ref | |
| 11-15 | 97 (55) | 102 (58) | 0.95 (0.62-1.5) | |
| >15 | 8 (5) | 3 (2) | 2.7 (0.68-10) | |
| Handwashing after school | ||||
| No | 22 (13) | 10 (6) | Ref | |
| Yes | 153 (87) | 165 (94) | 0.42 (0.19-0.92) | 0.38 (0.16-0.91) |
Discussion
We investigated an outbreak of AHC at School X in Kampala City. We identified 175 suspected cases of AHC, there were no confirmed cases and no fatalities. Pupils in boarding section and residents of boys dormitory Alpha were most affected. We found that being a boarding scholar was significantly associated with AHC. We also found that pupils in classes P4-P7 and those who reportedly washed their hands at arrival back at the dormitory/ home were protected against AHC.
Our study findings showed that pupils in boarding section were most affected than day scholars and we found that being a boarding scholar was significantly associated with AHC infection. This could be because the first case-patients fell ill on March 08, 2024 which was the first day of a long weekend (International women’s day weekend). The day scholars were thus not at the school during the start of the outbreak. By the end of the weekend the school had implemented initial control measures including exempting symptomatic pupils from attending class and thus reducing the possible interaction and infection of the day scholars. Furthermore, the dormitories were congested with learners sleeping on triple decker beds lined up to the wall and some adjacent beds had no space separating them, contrary to the public health school building recommendations set out by KCCA (7).
Being in classes P4-P7 and hand washing at arrival back at the dormitory/ home were protective against AHC. A study on the protective effect of hand hygiene found that children in higher age groups such as those in P4-P7 were protected against infections (8). Hand washing is one of the recommended ways by several health protection and promotion agencies so as to limit the risk of infection with AHC (5,9,10). In this case, handwashing at arrival back to the dormitory or home for day scholars broke the person to person transmission of AHC.
Study limitations
Due to logistical limitations, i.e., absence of molecular testing capacity, we failed to identify the causative pathogen in this outbreak. However, the case symptom presentation was consistent with AHC. The commonest eye symptoms in this outbreak were red eyes, watery discharge, grainy sensation, itching, photophobia, swelling, and pain which are typical symptoms used for the clinical diagnosis of AHC (11).
Conclusion
The outbreak at School X affected both pupils and staff members. Its spread was likely facilitated by dormitory congestion and poor hand hygiene practices. Education and awareness of good hand hygiene measures would prevent such outbreaks in future in the similar settings. We also recommended routine surveillance for AHC to help identify patterns and detect outbreaks earlier, which may help curb transmission in congregate settings such as schools.
Given that AHC can be spread by contact with fomites contaminated with the virus, we recommended disinfection of dormitories and classes and regular washing of personal items used by the case-patients.
Public health actions
We intensified early case finding by the matrons by teaching them the common symptoms to look out for and emphasized the temporary isolation for all case-patients at all dormitories. We held health education sessions educating learners on the signs and symptoms, transmission, and preventive measures for AHC. We also encouraged learners to practice good personal hygiene. We consulted with a senior ophthalmologist in Kampala City to guide on the management of the case-patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Author contribution
All authors contributed to the write-up and review of the bulletin. DA wrote the drafts of the manuscript and revised the paper for substantial intellectual content. TR and AN participated in the investigation of AHC at the School X. BK and RM supervised the investigation and reviewed the bulletin for substantial intellectual content. SKZ and DAO were involved in the review of the paper for substantial intellectual content. LB, and ARA reviewed the draft bulletin for substantial intellectual content.
Acknowledgements
The authors thank the staff of the Uganda Public Health Fellowship Program for the technical support and guidance offered during this study. The authors also extend their appreciation to the Kampala Capital City Authority and the administration of the School X for notifying the outbreak. This facilitated the notification of other schools in the metropolitan area and enabled the City to implement preventive and response measures to other places of congregate settings such as these. Finally, we thank the US-CDC for supporting the activities of the Uganda Public Health Fellowship Program.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- AHC (Pink Eye) | Disease Outbreak Control Division [Internet]. [cited 2024 Apr 11]. Available from: https://health.hawaii.gov/docd/disease_listing/AHC-pink-eye/
- Akçay E, Çarhan A, Hondur G, Tufan ZK, Duru N, Kılıç S, et al. Molecular identification of viral agents associated with acute AHC: a prospective controlled study. Braz J Infect Dis. 2017 Jul 1;21(4):391–5.
- Epling J. Bacterial AHC. BMJ Clin Evid. 2012 Feb 20; 2012:0704.
- CDC. Centers for Disease Control and Prevention. 2019 [cited 2024 Apr 11]. Pink Eye Symptoms. Available from: https://www.cdc.gov/AHC/about/symptoms.html
- CDC. Centers for Disease Control and Prevention. 2019 [cited 2024 Apr 30]. Help to Prevent the Spread of Pink Eye. Available from: https://www.cdc.gov/AHC/about/prevention.html
- Snapshot [Internet]. [cited 2024 Apr 11]. Available from: https://health.hawaii.gov/docd/disease_listing/AHC-pink-eye/
- PUBLIC HEALTH (SCHOOL BUILDINGS) RULES.pdf [Internet]. [cited 2024 Jun 1]. Available from: https://www.kcca.go.ug/media/docs/PUBLIC%20HEALTH%20(SCHOOL%20BUILDINGS)%20RULES.PDF
- Hand Hygiene Frequency by Age Group and Healthcare Worker Status. | Download Scientific Diagram [Internet]. [cited 2024 May 8]. Available from: https://www.researchgate.net/figure/Hand-Hygiene-Frequency-by-Age-Group-and-Healthcare-Worker-Status_tbl1_352674333
- IPAC_Fall2017_Katz_Vearncombe_Deeves.pdf [Internet]. [cited 2024 Apr 30]. Available from: https://ipac-canada.org/photos/custom/CJIC/IPAC_Fall2017_Katz_Vearncombe_Deeves.pdf
- American Academy of Ophthalmology [Internet]. 2012 [cited 2024 Apr 30]. Infection Prevention in Eye Care Services and Operating Areas and Operating Rooms – 2012. Available from: https://www.aao.org/education/clinical-statement/infection-prevention-in-eye-care-services-operatin
- Solano D, Fu L, Czyz CN. Viral AHC. In: StatPearls [Internet] [Internet]. StatPearls Publishing; 2023 [cited 2024 Jun 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470271/


Comments are closed.