Increasing cases of Multi-drug Resistant Tuberculosis associated with poor adherence to first-line anti- tuberculosis treatment: West Nile Region, 2013-2017
Denis Okethwangu1, Doreen Birungi1, Benon Kwesiga1, Alex R. Ario1; Affiliation: 1Uganda Public Health Fellowship Program
Summary
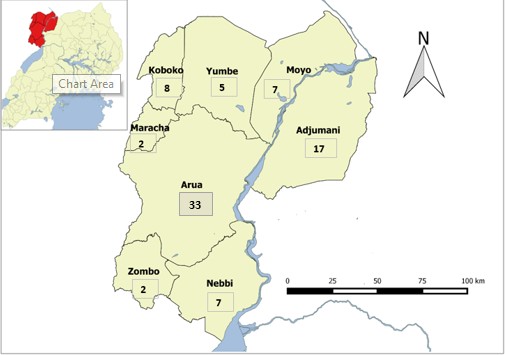
Multidrug resistant tuberculosis (MDR-TB) is infection with strains of Mycobacterium tuberculosis resistant to isoniazid and rifampicin. Compared to drug-susceptible tuberculosis, treatment of MDR-TB is a lengthy and expensive undertaking, and has a lower cure rate. It has been estimated that treatment of drug resistant tuberculosis takes up over 50% of the budget of national TB control programs. In July 2017, Medical Teams International (a Non-Governmental Organization) reported high cases of MDR-TB in Arua District with some among refugees. We set out to determine the scope of MDR-TB in West Nile Region. In Arua District specifically, we identified risk factors for MDR-TB and assessed capacity of health facilities and communities to prevent MDR-TB spread. Between 2013 and 2017, we identified 85 MDR-TB cases in West Nile of which 33 were from Arua District. 73% (62/85) were males while 19% (16/85) were refugees. In Arua, a case-control study among MDR-TB case-persons and TB patients (as controls) revealed that poor adherence to first line anti-TB drug regimen and positive HIV status were associated with the develop- ment of MDR-TB. We also found that infection prevention and control practices at the Hospital and in the community present a big risk for transmission of MDR-TB cases. We recommended adequate isolation of MDR-TB cases, emphasis on TB drug adherence and use of masks.
Introduction
The emergence of multidrug resistant tuberculosis (MDR-TB) has attracted global concern. Treatment of MDR-TB is a lengthy and expensive undertaking, yet with only about 55% cure rate (1). MDR-TB is caused by Mycobacterium tuberculosis strains that are resistant to isoniazid and rifampicin. It may be acquired through inappropriate TB treatment or transmitted from person to person. A person with TB who does not adhere to first-line anti-TB treatment is at risk of MDR-TB. Additionally, MDR-TB infected persons may transmit the drug-resistant strain to uninfected persons through droplets. High risk groups for the development of MDR-TB include HIV-infected persons and patients exposed to TB treatment (2). Refugees may also be at risk for MDR-TB through crowded living conditions and poor medical supplies (3). Medical Teams International, an organization that works with refugees in Uganda, reported 14 confirmed cases of MDR-TB in Arua District, particularly among refugees. We set out to determine the scope of MDR-TB in West Nile, identify risk factors for development of MDR-TB in Arua District and assess the capacity of health facilities and the community to prevent development/spread of MDR-TB.
Methods
We defined a suspected MDR-TB case as a TB case who had been on first-line anti-TB treatment for at least 2 months. We defined a confirmed MDR-TB case as resistance to at least rifampicin and isoniazid confirmed by Gene-Xpert or molecular Drug Susceptibility Test (DST).
We abstracted data from the TB initiation center at Arua Regional Referral Hospital (ARRH). We identified records of all MDR-TB patients resident in Arua District from 2013 to 2017 and conducted descriptive epidemiology. We generated and tested hypotheses using a case-control study.
The ratio of cases to controls was 1:3. Controls were defined as TB cases on treatment for at least 2 months and had a negative Gene- Xpert result for resistance to rifampicin. We used structured questionnaires to assess the capacity of health facilities to diagnose and manage TB. Through observation, we assessed infection control and prevention practices in health facilities and community.
Results
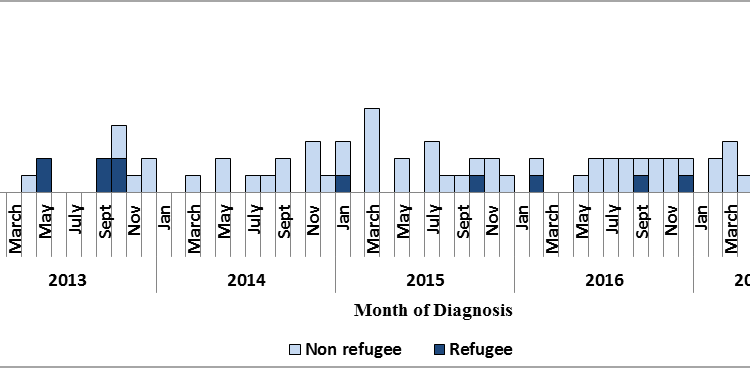
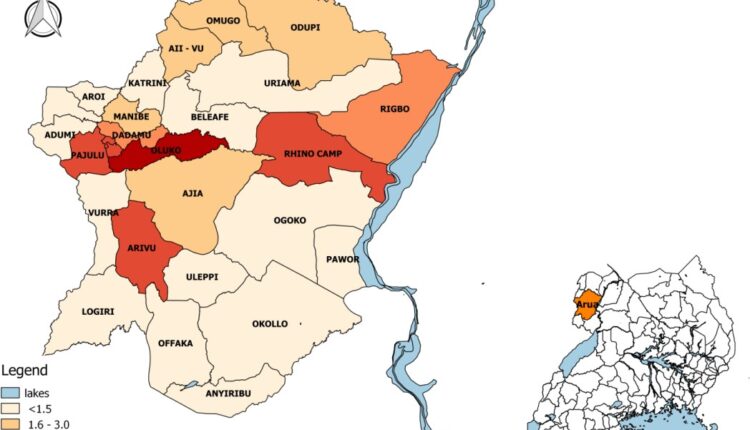
Between 2013 and 2017, we identified 85 MDR-TB cases in West Nile of whom 33 were from Arua. 73% (62/85) were males while 19% (16/85) were refuges (Figure 1). Among Arua case-persons, we found that poor adherence to first-line TB treatment (OR-14.3 [95% CI: 4.6-44.7]) and positive HIV status (OR-2.4 [95% CI: 1.1-5.5]) were significantly associated with development of MDR-TB. Oluko sub-county had the highest proportion of MDR-TB cases (Figure 3). All health facilities assessed reported having stock-outs of essential anti-TB commodities while 89% (8/9) of facilities sampled were accredited to provide TB services and had a laboratory, 56% had at least one laboratory staff. Infection control and prevention practices in health facilities and community were poor. At Arua Regional Referral Hospital (ARRH), 11 MDR-TB inpatients exceeded the initial carrying capacity of 4. Therefore MDR-TB patients were transferred to the drug-susceptible TB ward increasing likelihood of spread of infection.
Discussion
The association of poor adherence to first-line anti-TB drugs is consistent with findings found in other studies. Van der Werf et al. (2012) demonstrated that patients who had had an inappropriate treatment had a 27-fold risk of developing MDR-TB (4). Similar studies were reported in Bangladesh and India (5,6). Studies have also provided evidence for the association of HIV infection and development and MDR-TB. A systematic review found that a positive HIV status is associated with primary MDR-TB (7). Contrary to results from a survey conducted in India among Tibetan refugees (8), we found that being a refugee was not associated with development of MDR-TB. Frequent stock- outs of essential TB commodities negatively impact on adherence to anti-TB treatment.
Conclusion
There has been a high proportion of MDR-TB cases among TB cases in West Nile, Uganda since 2013. We recommended that the Ministry of Health ensures timely provision of adequate anti-TB commodities; intensifies directly observed therapy in health facilities and in communities; trains community healthcare workers in the basic management of TB cases; and expands the MDR-TB Ward at ARRH.
References
- Cain KP, Marano N, Kamene M, Sitienei J, Mukherjee S, Galev A, et al. The Movement of Multidrug-Resistant Tuberculosis across Borders in East Africa Needs a Regional and Global Solution. PLOS Med. 2015 Feb 24;12(2):e1001791.
- Berhan A, Berhan Y, Yizengaw D. A Meta-Analysis of Drug Resistant Tuberculosis in Sub-Saharan Africa: How Strongly Associated with Previ- ous Treatment and HIV Co-Infection? Ethiop J Health Sci. 2013 Nov;23 (3):271–82.
- European Centre for Disease Prevention and Multidrug resistant tuberculosis in migrants, multicountry cluster – 13 April 2017. Stockholm: ECDC; 2017.
- Van der Werf MJ, Langendam MW, Huitric E, Manissero Multidrug resistance after inappropriate tuberculosis treatment: a meta-analysis. Eur Respir J. 2012 Jun;39(6):1511–9.
- Isaakidis P, Das M, Kumar AMV, Peskett C, Khetarpal M, Bamne A, et Alarming Levels of Drug-Resistant Tuberculosis in HIV-Infected Pa- tients in Metropolitan Mumbai, India. PLOS ONE. 2014 Oct 21;9 (10):e110461.
- Ullah I, Javaid A, Tahir Z, Ullah O, Shah AA, Hasan F, et al. Pattern of Drug Resistance and Risk Factors Associated with Development of Drug Resistant Mycobacterium tuberculosis in Pakistan. PLOS ONE. 2016 Jan 25;11(1):e0147529.
- Suchindran S, Brouwer ES, Van Rie A. Is HIV Infection a Risk Factor for Multi-Drug Resistant Tuberculosis? A Systematic PLoS ONE [Internet]. 2009 May 15;4(5). Available from: http://
www.ncbi.nlm.nih.gov/pmc/articles/PMC2680616/
8. Salvo F, Dorjee K, Dierberg K, Cronin W, Sadutshang TD, Migliori GB, et Survey of tuberculosis drug resistance among Tibetan refugees in India. Int J Tuberc Lung Dis. 2014 Jun 1;18(6):655–62.


Comments are closed.