Increase access to safe drinking water in Kampala slums to prevent future occurrence of cholera and other diarrheal disease outbreaks in the city
Author: Daniel Eurien1; Affiliation: 1Uganda Public Health Fellowship Program, Kampala, Uganda
Executive Summary
Kampala Capital City Authority (KCCA) with the Ministry of Health (MoH) battled a severe cholera outbreak from January to February 2019 that resulted in 3 deaths and affected 50 people in the five city divisions. The immediate response by KCCA and MoH was swift, and was instrumental in containing the outbreak. However, it is important that policymakers prioritize provision of safe water and improve sanitation coverage urgently to prevent future out-breaks in Kampala slums especially with the looming rain season. This brief examines the epidemiology of the recent cholera outbreak in Kampala and provides recommendations to policymakers and implementers on what needs to be done to prevent future similar cholera outbreaks in Kampala. The author suggests that the most recent outbreak should re-echo the need for the local government authorities to fully enforce the Public Health Act to prevent recurrent faecal contamination of water sources that are the root cause of the persistent cholera out-breaks in Kampala.
Introduction
Uganda is categorized by the World Health Organization (WHO) among the 51 “cholera endemic” countries; classified as those re-porting confirmed cholera cases detected during the last 3 years with evidence of local transmission (1).
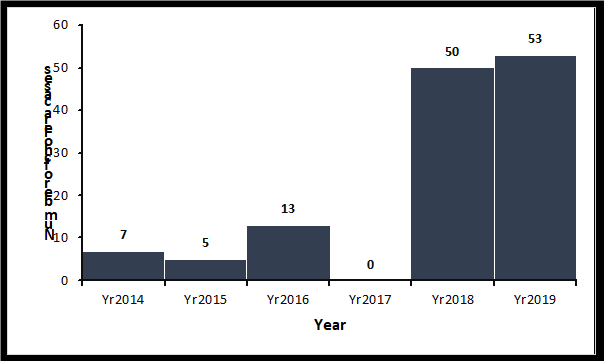
Kampala city slums along with districts bordering Democratic Republic of Congo (DRC) and Karamoja region to the north east are the three cholera hotspots in Uganda(2). Cholera cases have been reported in Kampala city over the last six years with exception of 2017. (Figure 1). Kampala city, like most cities in developing countries, is experiencing rapid urbanization leading to an increase in population, and rapid development of periurban (informal) settlements. More than 60% of the city’s population with low incomes reside in these settlements which have the lowest basic service levels (sanitation, water supply, solid waste collection, and storm water disposal) (3) ,(4). Most slums in Kampala are densely populated and situated in low-lying areas, making them susceptible to frequent flooding during heavy rains. Additionally, pit latrines are the dominant sanitary facilities used in these slums, resulting in constant risk of faecal contamination of shallow ground water, which is used as a drinking water source by a large number of slum dwellers (4,5). Even though construction of pit latrines along drainage channels and release of sewage into open drainages is a public nuisance according to the Uganda Public Health Act 2000, this has not deterred the practice especially in slum dwellings (6). This therefore, puts the slum dwellers at constant risk of cholera outbreaks whenever flooding occurs.
Cholera is an infectious disease with a short incubation period of a few hours to 5 days and has a high epidemic potential. It is transmitted through consumption of food, or water contaminated with cholera bacteria (7). It commonly presents with profuse painless watery diarrhea and vomiting and when untreated, about 5% of the cases die of severe dehydration (7).
In this policy brief, we examine the source of the recent cholera outbreak, mode of transmission, and recommend evidence-based interventions.
Approaches and Results
To be able to identify as many cases as possible, we used two strategies i.e. health facility and community case finding. The team visited health facilities and reviewed out patient, in-patient and laboratory records to identify current or previous patients that fulfilled the case definition. Patients who had been seen at a health facility and discharged were followed up and assessed. With the help of Village Health Teams (VHTs), the team also visited affected villages to identify more cases. We conducted a case control study matched by age using a ratio of 1 case: 5 controls. A case was any person with onset of profuse, painless acute watery diarrhea in a Kampala City resident (≥2 years) from 28 December 2018 to 11 February 2019. Controls were persons from the same village who never had any symptoms resembling cholera from December 28th 2018 to 11th February 2019. We assessed potential risk factors such as: source of drinking water, handling of water from collection to storage, water treatment practices and travel history to a place with cholera outbreak. We conducted an environmental assessment, and tested water samples from randomly selected households and water sources using culture and PCR to identify V. cholera.
We identified 50 people were affected, with 3 (6.0%) deaths. All age groups were affected; with age group 5-14 years being the most affected with attack rate (AR) (8.2/100,000). Cases were clustered in Sembule village, Lubaga Division which was the epicenter of this outbreak. We found that people who drank water from well X were 21 times more likely to develop cholera compared to those who took water from other sources (ORM-H=21, 95% CI: 4.6–93). We also found that there was a 67% protective effect among residents who took water from the public token tap (ORM-H=0.33, 95% CI: 0.13–0.86) and those who boiled water before drinking had an 85% protective effect against cholera (ORM-H =0.15, 95% CI: 0.036-0.59). Of the 45 stool samples tested, 22 were con-firmed positive for V. cholerae O1, serotype Inaba; a bacterium responsible for causing cholera outbreaks. The epidemic curve showed serious point-source outbreaks preceded by rains.
Sembule village had a token-operated water tap, which had broken down one month prior to the outbreak, and residents resorted to drink water from the open well. Environmental assessment showed that residents emptied their faeces into the drainage channel that was connected to the open well. Water from a container in one of 8 households tested positive for V. cholerae; water from open well had coliform counts 900MPN/100ml.
Sembule village water systems
Sembule village, like most slums in Kampala is located in a swamp. The main sources of drinking water were: public token tap, private water tap and open well water. Residents accessed water from public token pipe at Uganda Shillings 38 per 20-liter jerry can. Sembule village had six public token taps; each token tap serving 20 house-holds. It also had four open wells; two of which were free to the community. Meanwhile, a 20-liter jerry cost Uganda Shillings 300 for other two wells. Sembule village also had households with private taps that charged residents Uganda shillings 500 for a 20-liter jerry. We established that 87% (20/23) of cases accessed water from one public stand pipe. However, the tap broke down in December 2018; therefore, residents fetched water from other cheaper sources including from the free open wells. We observed that well X (implicated well) was in close proximity with a drainage channel that drained fecal matter from the latrines (Figure 2). The drainage channel flooded submerging the open well X. Community members waited for storm water to recede before collecting water. We found evidence of fecal matter released into the drainage channel from one of the pit latrines constructed along the drainage channel. We also observed that most of the community pit latrines were constructed along the drainage channel.
Conclusions
This outbreak was caused by drinking contaminated water from implicated well X. Break down of token tap forced members of the most affected households to resort to the cheaper alternative source of water that turned out to be heavily contaminated with faeces. We recommended emergency chlorination of drinking water, fixing the broken public tap, closure of well X, sensitization about the danger of drinking water from well X, and improving latrines so they are not discharged into the drainage channel.
Policy implications
Cholera outbreaks will continue occurring in Kampala slums if; coverage of safe water is not increased through increasing the number of cheap public token taps, Public Health Act is not fully enforced to ensure that all households have pit latrines and ensuring that no household discharges feces into the drainage channels.
Policy recommendations
Kampala Capital City Authority (KCCA) and National Water and Sewerage Corporation should increase access to affordable portable water in slum dwellings by increasing the number of public token taps. These water tokens should be accessible to every household to avoid exploitation by a few people in possession of water tokens. KCCA should ensure full enforcement of the Public Health Act for every landlord to provide sanitary facilities and ensure that feces are not released to the drainage channels during rainy days.
References
1.Ang GY, Yu CY, Balqis K, Elina HT, Azura H, Hani MH, et al. Molecular Evidence of Cholera Outbreak Caused by a Toxigenic Vibrio cholerae O1 El Tor Variant Strain in Kelantan, Malaysia. Journal of Clinical Microbiology. 2010 Nov 1;48(11):3963–9.
2.Bwire G, Malimbo M, Maskery B, Kim YE, Mogasale V, Levin A. The Burden of Cholera in Uganda. PLoS Negl Trop Dis [Internet]. 2013 Dec 5 [cited 2019 Jan 14];7(12). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3855006/
3.2014 National Census Main Report.pdf [Internet]. [cited 2019 Jan 21]. Available from: http://www.ubos.org/onlinefiles/uploads/ubos/NPHC/2014%20National%20Census%20Main%20Report.pdf
4.Kulabako RN, Nalubega M, Wozei E, Thunvik R. Envi-ronmental health practices, constraints and possible interventions in periurban settlements in developing countries – a review of Kampala, Uganda. Internation-al Journal of Environmental Health Research. 2010 Aug 1;20(4):231–57.
5. Katukiza AY, Ronteltap M, Oleja A, Niwagaba CB, Kansiime F, Lens PNL. Selection of sustainable sanitation technologies for urban slums–a case of Bwaise III in Kampala, Uganda. Sci Total Environ. 2010 Dec 1;409(1):52–62
6.Public health act Chapter_281.pdf [Internet]. [cited 2019 Feb 12]. Available from: https://www.kcca.go.ug/uDocs/public%20health%20act%20Chapter_281.pdf
7.World Health Organisation cholera fact sheet [Internet]. [cited 2019 Jan 14]. Available from: https://


Comments are closed.