Improvement of Sample Receipt Turnaround Time for HIV Viral Load using a Continuous Quality Improvement Approach, Kigezi, Uganda, April-September 2023
Authors: Leah Naluwagga Baliruno*1, 2, Samuel Gidudu1, Harriet Nakigozi2, Sarah Elayeete1, Fredrick Nsubuga2, Alex Riolexus Ario1; Institutional affiliations: 1Uganda Public Health Fellowship Program-Laboratory Leadership Program, National Institute of Public Health, Kampala, Uganda; 2National Health Laboratories and Diagnostic Services, Ministry of Health, Kampala, Uganda; Correspondence*: Tel: 0702533694, Email: lnaluwagga@uniph.go.ug
Summary
Background: Uganda has an established national sample transport and referral network based on the hub-and-spoke model. All health facilities’ samples are expected to be received within 7 days at the Central Public Health Laboratory (CPHL). However, from October to December 2023, only 1(1%) of health facilities’ samples in Kigezi region were received within 7 days. We conducted a continuous quality improvement (CQI) project to reduce the sample receipt turnaround time.
Methods: A Continuous Quality Improvement (CQI) team was formed to coordinate the implementation of the CQI project, conducted stakeholder meetings, and used root-cause analysis techniques to identify the total control root causes and these were prioritized. Interventions included performance review meetings, improved coordination, communication, and timely data review. Progress was monitored using a quality indicator.
Results: Reasons for long sample receipt included poor coordination and communication. At baseline from April to May 2023, only 2 (2%) of spoke health facilities had samples received at CPHL and 52 (71 %) of spoke health facilities had samples received at CPHL in ≤7 days at end line.
Conclusion: Performance review meetings with hub coordinators, riders and spoke health facility staff as well as strengthening coordination and communication improved sample receipt turnaround time in Kigezi region.
Background
A specimen referral network is a coordinated system that allows a health facility or laboratory lacking the capacity to perform particular tests to safely send a patient’s specimen to another or higher-level laboratory with the capacity to perform the requested test(s) (1).
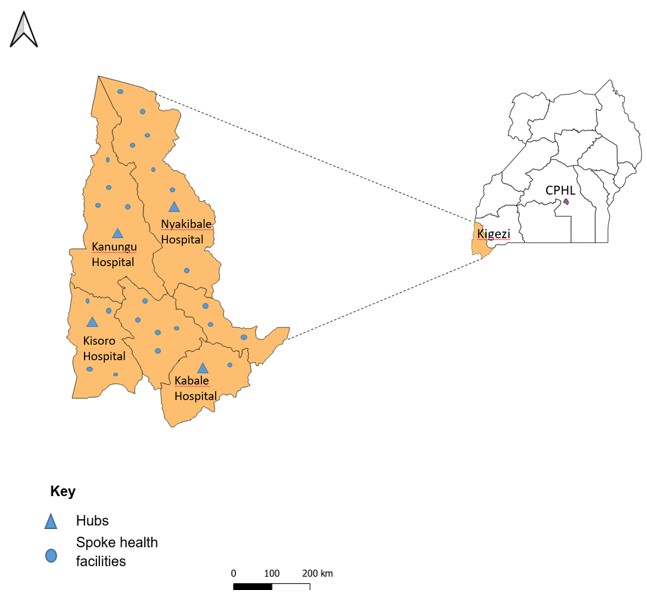
Uganda has a centralized specimen referral system in place. The hub-and-spoke model is where the “hub” is a central health facility that is identified to serve as a central specimen collection point for specimens coming from multiple referring sites, termed “spokes”. From the hub, the specimens are transported to the reference laboratory for testing (1). In Uganda, the hub-and-spoke model was initially established for the transport of Early Infant Diagnosis (EID) samples and has since expanded to transport other sample types including HIV Viral Load samples (4). The hub is accessible to a minimum of 15 health facilities within a radius of 40km maximum and drivers and courier bikers transport samples at least weekly to the hub and from the hub to the Central Public Health Laboratory, Ministry of Health Uganda (CPHL, MOH).
Central Public Health Laboratories, Ministry of Health routinely monitors the National Sample Transportation, Referral and Results Network (NRSTN) to improve its efficiency (5). However, there are still many challenges with some regions operating sub-optimally compared to others (6). High turnaround time in the NRSTN is a prevailing challenge. The NSTRN turnaround time (TAT) is broken down into 3 sections i.e. TAT sample collection to receipt at CPHL, TAT sample receipt at CPHL to sample results dispatch (testing laboratory), and TAT sample results dispatch to sample Results Download at the facility. The sample receipt starts from when samples are collected at the spoke health facility to when the samples are received at CPHL. From October- December 2022, Kigezi region had the lowest proportion of 1 (1%) of health facilities with samples received within 7 days. We identified the factors affecting VL sample receipt turnaround time in the Kigezi region and addressed the gaps using a continuous quality improvement approach.
Methods
Project implementation setting and design
We conducted this continuous quality improvement project in the Kigezi Region, South Western Uganda, from April to September 2023.
We considered Kigezi region because of its record of high turnaround time since October 2023, according to Ministry of Health – Central Public Health Laboratories, COP21 October 2022 – December 2022 Progress Report. We applied a four-stage problem-solving model used for improving a process or carrying out change (Plan-Do-Study-Act). Using this model, we focused on 3 fundamental questions: What are we trying to accomplish? How shall we know if a change is an improvement? And what changes should we make that can result in an improvement? We defined the aim of the quality improvement project by stating what we wanted to improve, how much improvement we wanted and by when (the timeline). The Quality improvement (QI) team defined their aim, identified measures, and changes to be made for improvement. We collected weekly data on the proportion of samples that had their samples received at CPHL, MOH within 7 days. We then conducted a final evaluation to ascertain whether there was an improvement in proportion of health facilities whose samples were received within 7 days.
Ethical considerations
This study reviewed by the US CDC and was conducted consistent with applicable federal law and the US CDC policy. We also obtained administrative clearance from the Central Public Health Laboratories, Ministry of Health before study start. All generated records were kept confidential and password protected.
Results
Baseline assessment findings
A total of 4 hubs served as central specimen points to 117 spoke health facilities. Only 2 (2%) of health facilities had their samples received at CPHL within 7 days. The majority 49 (42%) of health facilities were served by Kabale Hub with no health facility having their samples received at CPHL in ≤7 days (Table 1).
Table 1: Baseline assessment findings
| Hub | Total number of health facilities | Number of health facilities with samples received at CPHL within 7 days | Percentage |
| Kabale hub | 49 | 0 | 0 |
| Kanungu hub | 20 | 0 | 0 |
| Kisoro hub | 21 | 1 | 4.8 |
| Nyakyibale hub | 27 | 1 | 3.7 |
| Total | 117 | 2 | 2% |
Reasons for long sample receipt turnaround time in Kigezi, Uganda, April-September 2023
System factors, laboratory staff, ICT and hub rider related factors were identified as the broader causes for long sample receipt turnaround time. System factors included: wrong date written on collection form, workflow not aligned, not adhering to SOPs and writing forms before sample collection. Laboratory staff factors included; samples not ready for transportation, delayed sample packaging, and staff unavailability. ICT factors included; sub-optional sample tracking, outdated and not procuring new phones. Hub rider factors included: lack of adherence to transport schedule, adjustment of schedule, health facilities not ready on time, poor coordination and communication.
Poor coordination of the Hub riders and the spoke health facilities by the Hub coordinators as well as poor communication between Hub riders and the spoke health facilities were identified as contributory root causes within the team’s total control to influence change.
Effect of the intervention on the result receipt turnaround time
After the implementation of interventions, compared with only 2 (2%) at baseline, at the end line, 52 (71%) of health facilities in Kigezi region had their samples received at CPHL within 7 days (Table 2).
Table 2: Baseline and end-line assessment findings
| Baseline | End line | |||
| Hub | Total health facilities | Health facilities samples <7 days | Total health facilities | Health facilities samples <7 days |
| Kabale hub | 49 | 0 (0%) | 28 | 20 (71%) |
| Kanungu hub | 20 | 0 (0%) | 9 | 6 (67%) |
| Kisoro hub | 21 | 1 (5%) | 13 | 6 (46%) |
| Nyakyibale hub | 27 | 1 (4%) | 20 | 20 (100%) |
| Total | 117 | 2 (2%) | 70 | (52) 71% |
Discussion
Our study revealed a long sample receipt turnaround time at baseline. Poor coordination and communication were identified as the main root causes of long sample receipt turnaround time in Kigezi region. Performance review meetings, strengthening coordination, communication and timely review of data improved sample receipt turnaround time in the region leading to an increase in the percentage of health facilities that had their samples received at CPHL within 7 days.
Delay in sample pick up from the spoke health facilities was identified as one of the causes of delay in the study. This is in line with a study in South Africa, which showed that one of the most common issues that prolong pre-analytical TAT were delays in transport and sample collection from clinics to testing laboratories and changes in courier routes and pick-up times (7). Moreover, delay in sample transportation is one of the many causes of delayed pre-analytical TAT, which may be due to a lack of awareness of the consequences of delayed transportation on patients (8). This could also be attributed to several factors including delayed packaging at the spoke health facilities as shown by a study conducted in Bukedi region, Eastern Uganda, which also found that there were delays between the spoke health facility and hub caused by delayed packaging at spoke health facilities (9). In India, there was a long sample sorting time where the hub riders tended to wait for samples to pile up before transporting them (8).
During our study period, health facility staff including laboratory technologists, hub riders, and hub coordinators were laid off and this led to an increase in sample receipt turnaround time as a result of changes in Implementing Partners (IPs) for the Region. This is in line with other studies conducted which showed that short staffing of laboratory personnel has been noted to have a major impact on turnaround time. The throughput of the laboratory is related to many aspects of its workflow including sufficient staffing available to perform specific tasks (10). In a study conducted in India, it was found that failure to modify work schedules to coordinate available manpower, as well as a lack of manpower led to delayed turnaround time. The most impacted tests that require improvement are those for HIV viral load among other tests. Reducing delayed TAT skilled staff retention was among the many crucial strategies (11). Implementing partners also plays a pivotal role in terms of supporting laboratories to effectively manage and deliver quality services, this includes facilitating the hub coordinators and hub riders (6), therefore a transition of implementing partners in the region is likely to affect service delivery.
There was poor coordination and communication between hub riders and staff at spoke health facilities in our study, leading to a long sample receipt time. When staff at spoke health facilities were absent or not yet ready to prepare samples they would not communicate with hub riders. Hub riders would therefore adjust their schedule to their convenience without communicating with the health facilities or their supervisors leading to poor coordination. This was in line with a study conducted in Bukedi region which showed that there was poor communication and hub riders and staff and staff at the spoke health facilities leading to the delay of samples at the spoke health facilities, hence leading to increased turnaround time between the spoke and hub (9).
We had performance and quality management review meetings which are essential to the medical laboratory quality management system and a major opportunity for laboratory management and leadership to reaffirm its commitment to the management system and to continually improve its effectiveness. Performance review meetings are ISO 1589:2012 requirement in which is improvement of a key indicator such as turnaround time is paramount (12). In line with this, a study conducted in Bukedi region showed that the implementing partner supported the districts to hold quarterly performance review meetings to identify challenges and share learnings. This helped to reduce the turnaround time between spoke health facilities and the hub (9).
In our study, the hub coordinators were tasked to ensure the hub riders called the staff at the health facilities to improve communication and coordination. The laboratory managers were also encouraged to ensure the staff responsible for preparing the referral samples called the hub riders to ensure better coordination. Similarly, in a study in Bukedi district, cohesive coordination between the health workers and hub riders significantly improved turnaround time (9). Furthermore, a previous study in India, indicated that timely communication between healthcare workers and laboratory professionals is vital in ensuring mutual understanding and collaboration after the samples have been collected and delivered at the laboratory (13).
A weekly review of sample receipt turnaround on a WhatsApp forum was carried out during the study period. This enabled the key stakeholders to get timely information and therefore enable timely action. This is in line with a study in South Africa where it was found that adding weekly TAT component analysis at the laboratory level further identifies problematic testing weeks and possible causes of prolonged TAT. Weekly assessment of TAT and TAT components not only identified problematic testing laboratories or days with TAT challenge but also enabled the identification of individual outlier samples that can be investigated to assess causes of TAT delays (7). It has also been recommended that weekly monitoring of TAT identifies poor performance more accurately than aggregate reporting, thereby focusing on the identification of poorly performing laboratories that need immediate intervention (8). There is a need for periodic monitoring of delayed TAT and the reasons for elevated TAT and put improvement plans into place (7).
Study limitations
Only data entered into the Laboratory Information Management System (LIMS) was used for our study because the monitoring of TAT using the sample tracking system was limited. This was due to the stock-out of sample tracking barcodes. Strengthening the sample tracking system could provide valuable additional date and time values to allow for a more comprehensive TAT review.
Conclusion
Sample receipt turnaround time in Kigezi region improved through cohesive coordination between the health workers and hub riders. There should be continuous strengthening of coordination and coordination between health workers and hub riders.
Conflict of interest
The authors declare that they have no conflict of interest.
Authors Contribution
LNB, HN, FN and SG conceived and designed the analysis. LNB, HN, FN, and SG collected the data. LNB, HN, FN and SG contributed to the data analysis. LNB, HN, FN and SG performed analysis. LNB, HN, FN, SG, and SE wrote the bulletin. LNB, HN, FN, SE, and AA wrote and reviewed the bulletin to ensure scientific integrity.
Acknowledgements
We acknowledge the Uganda Public Health Fellowship Program, Central Public Health Laboratories Ministry of Health (CPHL) Uganda, Makerere University School of Public Health and Baylor Uganda for support and oversight of this project. We also acknowledge the US Centers for Disease Control and Prevention Uganda for implementation support. We also thank Kigezi Regional stakeholders for the implementation and coordination of this project.
Copyright and licensing
All materials in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Fonjungo PN, Alemnji GA, Kebede Y, Opio A, Mwangi C, Spira TJ, et al. Combatting Global Infectious Diseases : A Network Effect of Specimen Referral Systems. 2017;64.
- Dama E, Nikiema A, Nichols K, Bicaba BW, Porgho S, Tarnagda Z, et al. Designing and Piloting a Specimen Transport System. 2020;18.
- Gebregergs GB, Sinishaw MA, Shiferaw MB. Evaluation of the postal service for referral of specimen of drug resistance tuberculosis in Amhara region , Ethiopia ; mixed method. 2021;21(2).
- Kiyaga C, Sendagire H, Joseph E, Mcconnell I, Grosz J, Narayan V, et al. Uganda ’ s New National Laboratory Sample Transport System : A Successful Model for Improving Access to Diagnostic Services for Early Infant HIV Diagnosis and Other Programs. 2013;8(11):1–7.
- CPHL/MOH. MINISTRY OF HEALTH MINISTRY OF HEALTH – CENTRAL PUBLIC HEALTH LABORATORIES (MOH – CPHL) COP21 October 2022 – December 2022 PROGRESS REPORT. 2022;(October 2022):1–70.
- Ministry of Health U. Guidelines for the Uganda National Health Laboratory Hub and Sample Transport Network. 2017;(September).
- Coetzee L-M, Naseem C, Glencross DK. Weekly laboratory turn-around time identifies poor performance masked by aggregated reporting Authors: Afr J Lab Med. 2010;1–8.
- Prasad P, Kumar R, Kumar S, Sinha P. Monitoring and Root Cause Analysis of Clinical Biochemistry Turnaround Time at a Tertiary Care. 2023;15(6):1–7.
- Mangeni R. Reducing Viral load Turn around for sample transportation between Spoke Health facility and Laboratory Hub : A case study of Bukedi region , Eastern Uganda Program Goals , Scope and Design. 2023;
- Erika Deaton-Mohney MT(ASCP), CPP; Sharon Ehrmeyer, PhD MC, Farnsworth, PhD, DABCC; Theresa Kunzler, MS, MT(ASCP); Frederick Strathmann, PhD D&, Monica Thomas, MPA C. Overcoming Lab Staffing Shortages. 2023.
- Kobusingye JO, Limenyande MJ-M, Mayinja H, Erika Deaton-Mohney MT(ASCP), CPP; Sharon Ehrmeyer, PhD MC, Farnsworth, PhD, DABCC; Theresa Kunzler, MS, MT(ASCP); Frederick Strathmann, PhD D&, Monica Thomas, MPA C, et al. Turnaround Time: An Efficacy Measure for Medical Laboratories. Cureus. 2022;5(9).
- Theodorou D, Giannelos P. Medical laboratory quality systems-A management review. Int J Health Care Qual Assur. 2015;28(3):267–73.
- Kobusingye JO, Limenyande MJ-M, Mayinja H. Impact of turnaround time in delivery of Covid-19 results and surveillance: a case of points of entry, Uganda. J Interv Epidemiol Public Heal. 2022;5.


Comments are closed.