How prepared are we for cross-border outbreaks: Lessons Learned from an imported Cholera Outbreak using 7-1-7 approach, Elegu border point, Uganda, January 2024
Authors: Innocent Ssemanda¹*, Brian Kibwika1, Ritah Namusoosa1, Susan Waako1, Benon Kwesiga¹, Lilian Bulage1, Alex Ario1, Richard Migisha1; Institutional affiliations: ¹Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; Correspondence*:Tel: 0777531618, Email: issemanda@uniph.go.ug
Summary
Background: Cholera remains a major public health threat in Uganda, particularly in border districts that face recurrent outbreaks due to cross-border population movement. A 7-1-7 is a timeliness metric for outbreak detection, notification, and response which can be used to assess system performance. We investigated an imported cholera outbreak in Elegu Town, a border point between Uganda and South Sudan, in January 2024, highlighting the country’s preparedness and challenges in managing cross-border disease outbreaks using the 7-1-7 metric.
Methods: We defined a suspected case as the onset of acute watery diarrhea in an asylum seeker at the Elegu border point from January to February 2024. A confirmed case was a suspected case in which Vibrio cholerae was isolated in the stool by culture or PCR. We actively searched for cases and collected data on person characteristics, symptoms, and outbreak timeliness. We used semi-structured interviews to elicit insights from district health officials on the enabling factors and bottlenecks during the response. We used the 7-1-7 metric was used to assess detection, notification, and response timeliness.
Results: Thirteen members of the same refugee family from South Sudan were diagnosed with cholera within 6 hours of arrival at the Elegu border, with 4 (31%) confirmed cases. Of the cases, 9 (69%) were female, and 7 (54%) were below eighteen years. The authorities detected, notified, and responded to the outbreak within the 7-1-7 timelines, with no significant bottlenecks identified. The outbreak was detected and notified within one day and by the fifth day, a full response was mounted. The prompt response was attributed to the recent experience with Ebola and COVID-19, the availability of a functional emergency operations center, and the presence of trained surveillance frontline health workers.
Conclusion: The imported cholera outbreak at Elegu demonstrates Uganda’s preparedness in managing cross-border disease outbreaks. Achieving the 7-1-7 targets highlights the country’s capacity to detect, notify, and respond to such events. Continued investment in local-level disease detection, communication, and national-level resource mobilization will be crucial to sustaining an effective outbreak management strategy.
Introduction
Cholera remains a global public health threat, causing between 1.3 million to 4.0 million cases, and 21,000 and 143,000 deaths worldwide every year [1, 2]. For More than 50 years after its resurgence in Africa, cholera is still a major public health problem, characterized by a large disease burden, frequent outbreaks, and high case fatalities [3]. Between 2010 and 2020, 25 African countries reported 484,450 suspected cholera cases and 999 cholera outbreaks to the World Health Organization (WHO)[4]. From the late 1990s through the first decade of the twenty-first century, sub-Saharan Africa has reported more cholera deaths than any other region. Between 2007 and 2011, the annual Case-Fatality Ratios (CFRs) for cholera in sub-Saharan Africa ranged from2.22% to 2.95% [5-7]. This highlights the continued public health burden posed by cholera across sub-Saharan Africa, even in the face of advancements in scientific understanding and treatment of the disease.
In Uganda, epidemics of cholera have occurred regularly since the disease first appeared in 1971 and the disease has nearly become endemic, with cases reported every year since 2000 [8]. While many parts of the country have not experienced any outbreak of the disease, the border districts have had recurrent outbreaks in the last two decades [8, 9]. The Ministry of Health has instituted preventive and control measures that include the promotion of access to safe water, sanitation, and hygiene; health education and community mobilization; disease surveillance; and case management. However, cholera cases continue to be reported annually. Between 2011 and 2015, Uganda reported over 9,000 cases of cholera in 18 border districts, with an annual average of 60-182 deaths [9, 10]. In border districts, there is a greater chance of importation of cholera due to frequent travel by the community across borders and also the influx of asylum seekers during conflicts in the neighboring countries [11]. Cholera poses a significant threat to regions with vulnerable populations, such as refugees, fishing communities, and large urban slum settlements [9, 11].
Rapid detection, reporting, and response to an infectious disease outbreak are critical to prevent localized health events from emerging as pandemic threats. Rapid detection depends on effective disease surveillance systems leveraging data from multiple sources [12-14]. Timeliness is a key criterion for evaluating any disease surveillance system. How fast a system can detect a threat is critical for ensuring optimal performance [12, 13]. Since the West Africa Ebola epidemic of 2014–16, several frameworks have been developed to measure readiness capacity. Uganda has adopted a new global target of 7-1-7 whereby every suspected outbreak is identified within 7 days of emergence, reported to public health authorities with the initiation of investigation and response efforts within 1 day, and effectively responded to within 7 days [13, 15, 16]. With clear targets for each milestone, these metrics can inform real-time performance gaps by surfacing bottlenecks where targets are not being met. Building on the International Health Regulations (2005) and WHO’s “triple billion targets” methodology, 7-1-7 metrics simplify performance evaluation, provide a blueprint for outbreak communication, and drive performance improvement [17].
On January 21, 2024, the Ugandan Ministry of Health was alerted of 13 suspected cholera case-patients at the refugee reception center at the Elegu border town, in Amuru District, bordering Adjumani District. The patients presented with profuse vomiting and acute watery diarrhea. Eighty percent (4/5) of the stool samples from the patients tested positive for Vibrio cholerae by both rapid diagnostic test (RDT) and polymerase chain reaction (PCR). We investigated an imported cholera outbreak in Elegu Town, a border point between Uganda and South Sudan, in January 2024, highlighting the country’s preparedness and challenges while exploring enabling factors and bottlenecks in managing cross-border disease outbreaks using the 7-1-7 metric.
Methods
Study setting
The outbreak was reported at Elegu border Town which is located in Amuru District, Acholi Sub-region at the international border with Nimule Town, South Sudan approximately 105 north of Gulu City by road. Elegu Town has a population of 17,000 people. In 2016, this same area was affected by a cholera outbreak, with 44 (99%) of the cases being refugees from South Sudan [18]. In 2021, the Ministry of Health launched an emergency operations center in Arua to combat public health emergencies including outbreaks in the West Nile region.
Field investigation
We defined suspected case as the onset of acute watery diarrhea in an asylum seeker at Elegu Town from January 16, 2024, to February 5, 2024. A confirmed case was a suspected case in which Vibrio cholerae has been isolated in the stool by culture or PCR.
Using the case definition, we actively searched for cases in three of the biggest health facilities and reception center communities at the border town. In the health facilities, we reviewed records and interviewed health workers, patients, and caretakers to obtain any information relating to potential cases of cholera. At the refugee reception and collection center, we interviewed new asylum seekers and refugee community leaders regarding the possibility of them having signs and symptoms of cholera.
7-1-7 assessment
The cholera outbreak was managed by a combined team of members from the Adjumani District, Arua emergency operations center, and Elegu port health authorities. 7-1-7 has been proposed as a target for outbreak detection, notification, and early response, whereby every suspected outbreak is detected within 7 days of emergence and reported to public health authorities within 1 day of detection, and seven early response actions are completed within 7 days from reporting to public health authorities, indicating timely initiation of response [13]. We evaluated the team’s readiness to respond to public health emergencies using the 7-1-7 metric and assessment tool. We assessed the response timeliness, from the initial detection to the completion of the outbreak response activities. This start-to-end evaluation gauged the speed with which the district detected the outbreak, notified the Ministry of Health, and implemented the response measures. To gain insights into the response process, we interviewed the district officials who led the outbreak response efforts to understand the enabling factors and bottlenecks in the response.
Data analysis
We performed a descriptive analysis of the person characteristics of the cases, presenting numerical findings as frequencies and percentages. For the qualitative data from the interviews conducted, we employed content analysis, which enabled a systematic exploration of the participants’ perspectives and experiences. Two independent coders conducted a meticulous initial coding process, analyzing the text line by line and prioritizing inter-coder reliability. Any discrepancies were resolved through discussion and consensus. Following this, the codes were systematically organized into overarching categories, and the iterative process led to the emergence of the main themes. These themes were then reviewed, refined, and validated by revisiting the raw data to ensure accuracy.
Ethical considerations
We conducted this study in response to a public health emergency and as such it was determined to be non-research. The MoH authorized this study and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. §§See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
We obtained permission to investigate from the Adjumani District health authorities and the Nyumanzi refugee settlement authorities. We obtained verbal consent from all the respondents aged ≥18 years since were under isolation. For those aged <18 years, we obtained consent from the parents and assent from the respondents. Participants were assured that their participation was voluntary and that there would be no negative consequences for declining participation in the investigation. Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, which were inaccessible to anyone outside the investigation team
Results
Person characteristics of case-patients: Imported cholera outbreak at Elegu, Uganda-South Sudan Border, January 2024
We investigated a case of a cholera outbreak among 13 asylum seekers who belonged to the same family of 14. Originally from Khartoum, Sudan, they sought refuge in the town of Ruweng at the border between Sudan and South Sudan. Stool samples from five of the 13 suspects were sent to CPHL, Kampala, and four out of the five (80%) samples tested positive for cholera on both RDT and PCR. Of the 13 individuals, seven (54%) were children, and nine (69%) were female.
Symptoms and presentation of case-patients: Imported cholera outbreak at Elegu, Uganda-South Sudan Border, January 2024
On January 21, 2024, three hours after their arrival, 13 of the 14 family members developed acute watery diarrhea and vomiting, which are symptoms of cholera. They sought care at a nearby private facility within two hours of symptom onset. All thirteen (100%) case-patients had both diarrhea and vomiting. Eleven (85%) had general body weakness and 6(46%) had abdominal pain.
Timeline of the imported cholera outbreak at Elegu, Uganda-South Sudan Border, January 2024
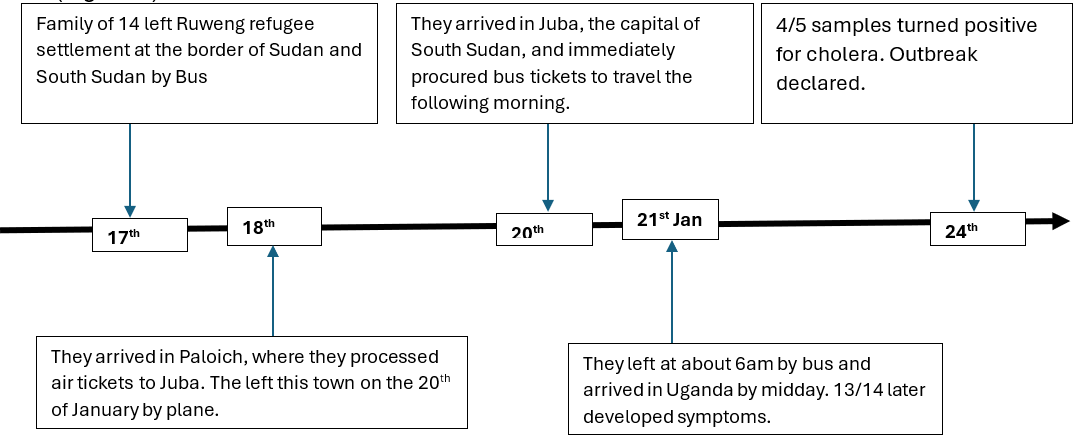
The family had been staying in the Ruweng Town refugee settlement in South Sudan for a month, planning to travel to Uganda. On January 17, 2024, they left the settlement and headed south, reaching the city of Paloich on the night of January 18. There, they booked a flight to Juba for two days later, on January 20.
While in Ruweng, the family bought food and other groceries from street vendors within the refugee settlement and used water from the settlement reservoir, which was treated with chlorine. The settlement had a high influx of refugees from Sudan and an ongoing cholera outbreak at the time. The family reported receiving cholera vaccines in Sudan three months prior, but there was no evidence to corroborate this.
On their journey to Paloich, the family ate bread and a local bread called Tamia, along with water they had packed. In Paloich, they bought rice and fish from the local market and used water from the reservoir, which was provided by an NGO and treated.
Once in Juba, the family bought eggs, meat, water, and powdered juice from a supermarket, which they cooked and consumed. The next morning, they packed some eggs and bread but did not eat anything until they crossed the border into Uganda at Nimule-Elegu border point. Three hours after the last meal, 13 of the 14 members fell ill (Figure 1).
7-1-7 Assessment findings: Imported Cholera Outbreak at Elegu, Uganda-South Sudan Border, January 2024
Detection: The initial cholera outbreak was detected on 21/01/2024 at the Elegu Point of Entry (PoE). A cluster of 14 asylum seekers sought clearance at the PoE health desk, and the index case, a 15-month-old male, exhibited initial cholera-like symptoms. The refugee reception center authorities suspected cholera and promptly completed a Case Investigation Form (CIF) on the same day. According to interviews with district officials who led the response and the frontline health workers, several key factors enabled this timely detection:
“The availability of appropriate case definitions and guidelines allowed us to quickly recognize the symptoms and suspect cholera,” noted the District Surveillance Focal Person (DSFP).
“The presence of a screening facility at the Elegu refugee collection and reception center was crucial for identifying these cases early on,” commented a Nyumanzi refugee settlement official.
“The swift detection of the outbreak was facilitated by the good attitude and ethics of the health workers. Our prior experience in dealing with cross-border issues during the COVID-19 pandemic also played a role in the timely response,” added Assistant District Health Officer (ADHO).
Notification: Immediately following the detection, the Surveillance team from Adjumani district took swift action. An alert was sent using the 6767 system to the electronic Integrated Disease Surveillance and Response (eIDSR) platform. Additionally, a phone call was made to Medical Teams International (MTI), an NGO supporting refugee settlement in the region, requesting Emergency Medical Services (EMS) for the suspected cases. Interviews with the surveillance team revealed that several key factors enabled this timely and effective response:
“Our knowledge of the existing alert management system, including the 6767 platform and eIDSR, allowed us to respond promptly,” stated a member of the surveillance team.
“The availability of the necessary tools and resources, such as case definitions and guidelines, ensured we had the right information to act on the alert,” remarked another team member.
“The clear communication and reporting channels from the Elegu refugee reception center to the district-level surveillance team facilitated the rapid notification during the outbreak,” added the DSFP.
Response: The response to the potential cholera outbreak was initiated immediately on the same day the index case was detected at the Elegu Point of Entry (PoE). The District Rapid Response Team (RRT) was swiftly deployed to investigate the situation, collect laboratory specimens, and initiate treatment while evacuating the suspected cases.
“Some of the response team members have recently had training as frontline field epidemiologists, these were very resourceful as we mounted the response,” said the District Health Officer (DHO).
The outbreak was detected, and authorities were notified within a single day. Furthermore, by day 5 of the outbreak, all response pillars had been functionalized (Table 3).
Table 3: A Table Showing Calculated Timelines within the 7-1-7 Period: Imported Cholera Outbreak at Elegu, Uganda-South Sudan Border, January 2024
| Interval |
Calculation In days |
Timeliness In days |
Target In days |
Met target? Yes/No |
| Detection | Difference between dates of emergence and detection | 1 | 7 | YES |
| Notification | Difference between dates of detection and notification | 1 | 1 | YES |
| Response | Difference between dates of notification and completion of the last early response action | 5 | 7 | YES |
Discussion
This study assessed an imported cholera outbreak in Uganda, highlighting the preparedness and challenges associated with cross-border outbreak management in the country. Thirteen refugees traveling from South Sudan to Uganda were diagnosed with cholera, 6 hours after they arrived at the Elegu point of entry. The authorities were able to detect, notify, and respond to the outbreak within the stipulated timelines as per the 7-1-7 Metric, and no significant bottlenecks were identified in the response to this outbreak.
Our findings indicate that the case-patients were exposed to cholera during their stay in Ruweng town, most likely on the day of departure since it marks the first day among the 5 days of incubation. The outbreak in Ruweng was reportedly imported from Sudan, which had experienced a cholera outbreak since September 2023, with over 10,000 cases and more than 290 deaths [19, 20]. Cholera importation is not uncommon, as shown by several studies [21, 22]. Ugandan districts near the border have been at the highest risk of such cholera outbreaks. A study on cholera surveillance in Uganda found that cholera was persistently occurring in the northwestern border districts of the country [6]. We recommend that all asylum seekers coming from regions with ongoing outbreaks should be thoroughly screened and vaccinated at the border point.
This assessment highlights the vulnerability of asylum seekers specifically and immigrants in general to cholera and other waterborne diseases during their displacement and migration. A study on cholera prevention and control in refugee settings found that these outbreaks consistently involved inadequate water chlorination, a lack of sanitation facilities, and improper disposal of cholera waste[23]. Refugees may encounter different strains of cholera or other pathogens along their journey, which may require different prevention and treatment strategies. Therefore, it is essential to provide adequate water, sanitation, and hygiene (WASH) facilities, health education, and oral cholera vaccines (OCV) to asylum seekers and other displaced populations, especially in areas with endemic or epidemic cholera [23, 24].
In this study, we describe the use of the 7-1-7 metric for reporting on the timeliness of outbreak response, which was designed to align with and support the implementation of the International Health Regulations (IHR), specifically, the capacities at the community or primary public health response level, intermediate public health response level, and national level [13, 17]. We found that for the imported cholera outbreak at Elegu, the Uganda-South Sudan border point in January 2024, the authorities were able to detect, notify, and respond to the outbreak within the stipulated 7-1-7 timelines. Prompt response initiation was observed, with the outbreak being detected and notified within 1 day. However, it’s also important to note that this was a relatively smaller outbreak containing a few cases without secondary cases, which could have facilitated this exceptional performance.
According to the 7-1-7 metric, the authorities responding to the outbreak, met the targets for detection, notification, and reporting [13]. These were done in 1:1:5 days, compared to the set target of 7:1:7 days respectively [16]. This performance can be attributed to the recent experience of both Ebola and COVID-19 outbreaks. The outbreak found the district with an existing and functional Regional Emergency Operations Centre (REOC), trained frontline health workers, and a response structure with clear pillars and terms of reference [25].
The fact that the frontline health workers at the district and the reception center had had some training in surveillance show that disease detection capacities must continue to be developed at both public and private health facilities, as most events are detected by health workers outside the public health system. A study done in Uganda comparing both private and public facilities capacity to detect disease outbreaks further highlighted this need [26]. Clear communication and reporting channels between health workers and surveillance officers are crucial to verifying events and initiating a larger public health response [16]. The analysis revealed that the most frequent response bottlenecks such as resource limitations and the availability of countermeasures, at the district level were not significant issues during this outbreak. However, the national-level and partner support resources to augment these gaps were a major enabling factor in the response.
These insights underscore the importance of strengthening disease detection and response capacity at the local level while ensuring effective coordination and resource mobilization at the national level to support a comprehensive and timely outbreak management strategy. Our analysis indicates that the 7-1-7 target is achievable during outbreak management and highlights the importance of continued system strengthening.
Study limitations
The reliance on qualitative interview data is a key limitation of this assessment, as information gathered through interviews can be subject to potential biases, selective memory, and incomplete recollection of events.
Conclusion
In conclusion, this study on the imported cholera outbreak at Elegu, the Uganda-South Sudan border point in January 2024, demonstrates the preparedness and challenges associated with cross-border outbreak management in Uganda. Despite the initial detection of 13 cases among refugees arriving from South Sudan, the authorities were able to respond within the stipulated 7-1-7 timelines, highlighting the country’s capacity to manage such outbreaks. The prompt detection, notification, and response were facilitated by the recent experience with Ebola and COVID-19 outbreaks, as well as the availability of a functional emergency operations center and trained frontline health workers. However, the findings also underscore the need to continue strengthening disease detection capabilities at the local level, improving communication between health workers and surveillance officers, and ensuring adequate resource mobilization at the national level to sustain an effective and comprehensive outbreak management strategy, especially for larger events.
Recommendations
Based on the findings, we recommended several actions to prevent and control cholera among asylum seekers and other vulnerable populations. Firstly, the surveillance and response systems for cholera and other diarrheal diseases should be strengthened in the affected areas, including the refugee collection centers and border points, potentially through regular screening of all incoming refugees. Secondly, mass vaccination campaigns with oral cholera vaccine (OCV) should be conducted for both the refugee and host communities, particularly in high-risk areas or where outbreaks are ongoing. These multi-faceted interventions targeting surveillance, sanitation, and vaccination can help mitigate the risk of cholera outbreaks among these vulnerable populations.
Conflict of interest
The authors declare that they had no conflict of interest.
Authors’ contributions
IS: participated in the conception, investigation, design, analysis, and interpretation of the study and wrote the draft bulletin; BK, RN, MN, and BK reviewed the report, reviewed the drafts of the bulletin for intellectual content and made multiple edits to the draft bulletin; BK, LB, and ARA reviewed the final bulletin to ensure intellectual content and scientific integrity.
Acknowledgments
The authors express their gratitude to the staff of the Uganda Public Health Fellowship Program for their technical support and guidance during the study. They also extend their appreciation to the Ministry of Health and the rapid response team for providing access to the notes and case-patients. We would also like to thank the Uganda Centre for Disease Control and Prevention for their technical support.
Furthermore, the authors acknowledge and appreciate the support from the Elegu Border Authorities, particularly the Port Health team and the Elegu Refugee Reception Centre, as well as the staff at Nyumanzi Health Centre III during the investigation who initiated conversations between our team and the port health team from South Sudan.
Lastly, the authors are thankful for the technical support provided by the Arua Regional Emergency Operations Centre and the West Nile Regional WHO offices during the investigation while using the 7-1-7 metric.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Bhattacharya, S.K., G.B. Nair, and Y. Takeda, Renewed Interest in Cholera Control. Journal of Gastroenterology & Hepatology Reports, 2022. 3(1): p. 1-5.
- Erkyihun, G.A., N. Asamene, and A.Z. Woldegiorgis, The Threat of Cholera in Africa. Zoonoses, 2023. 3(1): p. 20230027.
- Mengel, M.A., et al., Cholera outbreaks in Africa. Cholera outbreaks, 2014: p. 117-144.
- Zheng, Q., et al., Cholera outbreaks in sub-Saharan Africa during 2010-2019: a descriptive analysis. International Journal of Infectious Diseases, 2022. 122: p. 215-221.
- Echenberg, M., Africa in the Time of Cholera: A History of Pandemics from 1817 to the Present. Vol. 114. 2011: Cambridge University Press.
- Mukhopadhyay, A.K., Y. Takeda, and G. Balakrish Nair, Cholera outbreaks in the El Tor biotype era and the impact of the new El Tor variants. Cholera outbreaks, 2014: p. 17-47.
- Bartelt, L.A. and R.L. Guerrant, Challenges in Enteric Epidemics: barometers of inadequate water and sanitation, in Challenges in Infectious Diseases. 2012, Springer. p. 147-202.
- Cummings, M., et al., A cholera outbreak among semi-nomadic pastoralists in northeastern Uganda: epidemiology and interventions. Epidemiology & Infection, 2012. 140(8): p. 1376-1385.
- Ministry of Health, U. PREVENTION AND CONTROL OF CHOLERA. 2017; Available from: https://www.health.go.ug/wp-content/uploads/2019/11/Final-CHOLERA-GUIDELINES-2017_0.pdf.
- Oguttu, D.W., et al., Cholera outbreak caused by drinking lake water contaminated with human faeces in Kaiso Village, Hoima District, Western Uganda, October 2015. Infectious diseases of poverty, 2017. 6: p. 1-7.
- Bwire, G., et al., Cholera surveillance in Uganda: an analysis of notifications for the years 2007–2011. The Journal of infectious diseases, 2013. 208(suppl_1): p. S78-S85.
- Smolinski, M.S., A.W. Crawley, and J.M. Olsen, Finding outbreaks faster. Health security, 2017. 15(2): p. 215-220.
- Frieden, T.R., et al., 7-1-7: an organising principle, target, and accountability metric to make the world safer from pandemics. The Lancet, 2021. 398(10300): p. 638-640.
- Crawley, A.W., N. Divi, and M.S. Smolinski, Using timeliness metrics to track progress and identify gaps in disease surveillance. Health security, 2021. 19(3): p. 309-317.
- Bochner, A., et al., Implementation of the 7-1-7 target for detection, notification, and response to public health threats in five countries: a retrospective, observational study. Lancet Glob Health. 2023; 11 (6): e871-e879.
- Bochner, A.F., et al., Implementation of the 7-1-7 target for detection, notification, and response to public health threats in five countries: a retrospective, observational study. The Lancet Global Health, 2023. 11(6): p. e871-e879.
- Organisation, W.H. The Triple Billion targets: A visual summary of methods to deliver impact. [cited 2024 April 27th ]; Fact sheet]. Available from: https://www.who.int/data/stories/the-triple-billion-targets-a-visual-summary-of-methods-to-deliver-impact.
- (OCHA), O.f.t.C.o.H.A. Uganda: Emergency Update on the South Sudan Refugee Situation Inter-Agency Daily #28 | 17th August 2016. 2016 [cited 2024 11th May 2024]; Available from: https://reliefweb.int/report/uganda/uganda-emergency-update-south-sudan-refugee-situation-inter-agency-daily-28-17th.
- (OCHA), O.f.t.C.o.H.A., Sudan: Situation report. 2024.
- web, R. Sudan – Cholera outbreak, update (WHO, UN OCHA) 2024; Available from: https://reliefweb.int/report/sudan/sudan-humanitarian-update-4-february-2024.
- Connor, B.A., et al., Cholera in travellers: a systematic review. Journal of travel medicine, 2019. 26(8): p. taz085.
- Li, F., et al., Investigation of an imported cholera case in China with whole genome sequencing. Infection, Genetics and Evolution, 2020. 84: p. 104362.
- Shannon, K., et al., Cholera prevention and control in refugee settings: successes and continued challenges. PLoS neglected tropical diseases, 2019. 13(6): p. e0007347.
- Swerdlow, D., et al., Epidemic cholera among refugees in Malawi, Africa: treatment and transmission. Epidemiology & Infection, 1997. 118(3): p. 207-214.
- Kayiwa, J., et al., Establishing a Public Health Emergency Operations Center in an Outbreak-Prone Country: Lessons Learned in Uganda, January 2014 to December 2021. Health security, 2022. 20(5): p. 394-407.
- Buregyeya, E., et al., Comparison of the capacity between public and private health facilities to manage under-five children with febrile illnesses in Uganda. Malaria Journal, 2017. 16: p. 1-7.


Comments are closed.