HIV prophylactic treatment of HIV positive mothers and risk of infants’ HIV positivity
Authors: 1,2Okello P.E, 1Isaac Ssewanyana, 1,2Lilian Bulage, 1Aisu Stephen, 2A.R Ario 1Charles Kiyaga; Affiliations: 1Central Public Health Laboratories, 2Public Health Fellowship Program-Field Epidemiology Track
Summary
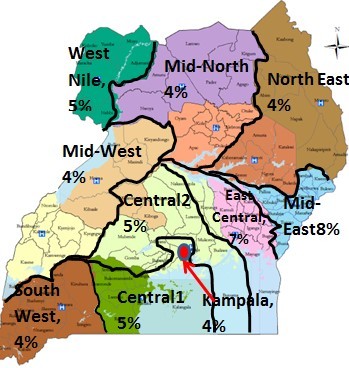
The Early Infant Diagnosis (EID) program of the Uganda Ministry of Health is mandated to diagnose HIV in infants and children at the earliest possible opportunity, usually at 6 weeks from birth. Diagnosis of HIV in infants and mothers is fol- lowed by prompt ART initiation under the policy of Elimination of Mother to Child Transmission (eMTCT) of HIV. We analyzed EID data from the national database at the Central Public health Laboratories (CPHL) from Jan – Dec 2015. Infant positivity rates were higher earlier in the year at 5.5% and declined progressively to 4% by December. . The highest positivity rates were in East Central (7%) and Mid-Eastern (8%) regions while other regions ranged from 4% to 5%. A total of 65,233 infants were tested for HIV by PCR1 between January and De- cember 2015, of which 3,121 (4.78%) were positive. Risk fac- tors for HIV positivity in exposed infants were lack of maternal ARV use, breastfeeding infant whose mother is ARV naive, and lack of ARV prophylaxis for the infant. As the EID program expands, more infants and mothers should be tested followed by prompt ART initiation.
Introduction: A pregnant woman who is HIV positive can transmit the virus to the baby during pregnancy, labour, birth, and breastfeeding; the likelihood ranging from 15% to 45% without antiretroviral treatment and highest in breast- feeding situations [1, 2]. Most mother to child transmission of HIV-1 is believed to occur in the third trimester of preg- nancy, during labor and delivery (3,4). Postnatal transmis- sion of HIV through breastfeeding is thought to cause about one-third to one-half of HIV-1 infections in children world- wide (5,6). Measures must be taken to prevent HIV transmis- sion. However, antiretroviral treatment, elective caesarian delivery, and other effective eMTCT interventions can re- duce this risk to below 5% (7)
In Uganda the Ministry of Health has made efforts to im- prove the health of mothers and their infants by strengthen- ing laboratory diagnosis of HIV. The laboratory method em- ploys PCR of viral RNA from dried blood spot samples (8). Diagnosis is followed by prompt initiation of anti-retroviral prophylaxis or treatment under the Early Infant Diagnosis (EID) program initiated in 2006.We described the epidemio- logic characteristics of infants under the EID program, assessed the risk factors for infant positivity rate and made recommendations for future improvements in EID services.
Method
We obtained data from the central EID database at CPHL. Infant variables included location (residence), age, sex, specimen collection date, specimen testing date, ARV prophylaxis/treatment status for mother and child, breast- feeding status of child, and infant HIV test results. Positivity rates and risk factors for the positivity were calculated. Risk factors were obtained using logistic regression.
Results
65,233 infants were tested for HIV by PCR1 between January and December 2015, of which 3,121 (4.78%) were positive.
Table 1: Profile of infants tested for HIV for the first time by PCR1, Uganda, 2015
| Result | Frequency | Percent |
| Negative | 62,078 | 95.16 |
| Positive | 3,121 | 4.78 |
| Invalid | 30 | 0.05 |
| Samples rejected | 4 | 0.01 |
| Total | 65,233 | 100 |
Positivity rates varied between 4 and 5.5% and rates are low- er towards the end of the year. (Specimens varied from 8,000 to 10,000 per month, each specimen represents a child).
Figure1: Percentage Monthly HIV Positivity rates by PCR1
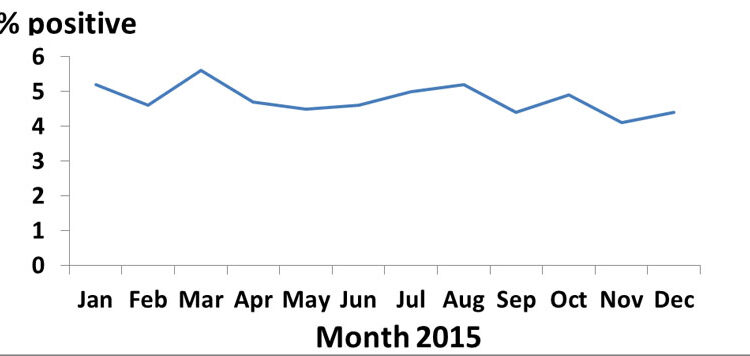
Figure 2: Infant HIV positivity rates by region;
| HIV+child | HIV-child | 95% CI | |||
| Variable | (n) | (n) | AOR* | Lower | Upper |
| Mother not on ART life long | 420 | 2,358 | 6.58 | 5.81 | 7.44 |
| Infant not on ART | 428 | 2,399 | 6.18 | 5.46 | 6.99 |
| No daily Nevirapine | 869 | 6,031 | 7.62 | 6.89 | 8.44 |
| Breastfed infant | 1,236 | 24,140 | 2.71 | 2.39 | 3.09 |
*AOR = adjusted odds ratio.
At antenatal, the odds of HIV transmission from ARV naïve mothers (during pregnancy) to their infants is 7.0(AOR = 6.58 and 95% CI 5.81 -7.44). At delivery, the odds of HIV transmission from ARV naïve mothers to their infants is 6 (AOR = 6.18 and 95% CI 5.46-6.99). An infant ARV naïve is up to 8 times more likely to get HIV infection from the mother (AOR 7.62, 95% CI = 6.89-8.44). Where the mother is ARV naïve, an infant is up to 3 times as likely to get HIV infection from breast milk, (AOR =2.71, 95% CI 2.39-3.09). Lack of ARV use mean the HIV positive person was not initiated on ARV for various reasons.
Discussion and conclusions
The EID indices analyzed vary in time, place and person in ways that provide opportunities for intervention to treat, prevent, or control HIV. HIV positivity rates dropped towards the end of the year. This could be due to intensification of the eMTCT campaign in which more mothers may have started lifelong ART (Option B+) towards the end of the year and reducing the mother to child transmission of HIV. The Eastern registered higher HIV positivity rates (Figure 1) and this calls for increased interventions to control HIV spread in mothers through whom the children acquire the infection perinatally. Identifiable risk factors for HIV positivity in exposed infants were lack of maternal ARV use, the breastfeeding infant whose mother is ARV naive, and lack of ARV prophylaxis for the infant. Lack of life-long ART use by HIV positive mothers promotes HIV transmission to infants during pregnancy, birth & breastfeeding. Infants and mothers should be tested fol- lowed by prompt ART initiation if HIV positive.
References
Bulterys, M., et al., Advances in the prevention of mother-to- child HIV-1 transmission: current issues, future challenges. AID Science, 2002. 2(4).


Comments are closed.