
Fatal Rift Valley Fever Outbreak Caused by Exposure to Sick Animals: Western and Central Uganda, July 2018
Authors: Angella Musewa1, Doreen Birungi1, Bernadette Basuta Mirembe1, Esther Kisaakye1, Steven N. Kabwama1, Benon Kwesiga1 and Alex Riolexus Ario1; Affiliations: 1Uganda Public Health Fellowship Program, Kampala Uganda
Summary
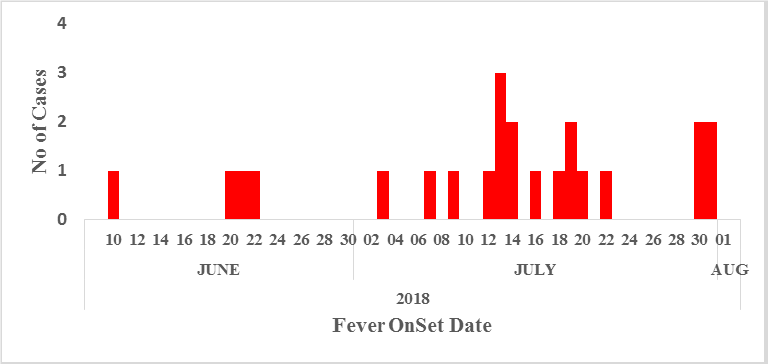
Rift Valley fever (RVF) is a disease affecting both humans and animals. On 25 June, 2018, the Uganda Virus Research Institute notified the Ministry of Health of a confirmed 49-year-old male RVF case from Kasese District. Subsequently, cases were re-ported from other districts. We investigated to determine the magnitude of the outbreak, identify exposure factors, and recommend evidence-based control measures. We identified 19 cases (17 confirmed, 2 probable); 13 (68%) died. The attack rate (AR) was 19 times as high in males (8.7/1,000,000) as in females (0.46/1,000,000). Of the 18 case-patients included in the case-control study and 90 controls, 10 case-patients (56%) and seven controls (7.8%) had a history of butchering/dissecting/carrying sick/dead livestock (ORMH=23, 95%CI=4.6-109). This outbreak was caused by exposure to raw meat from sick/dead livestock. RVF infection in area livestock appeared to be widespread. We recommend banning the processing of meat from sick/dead livestock
Background
Rift Valley fever (RVF) is a zoonotic viral haemorrhagic fever which is caused by an arthropod borne virus called Rift Valley Fever Virus (RVFV) 1. The virus may be transmitted to humans through handling of animal tissue, ingesting unpasteurized or uncooked milk of infected animals 2. Bites from infected aedes mosquitoes have been reported to cause disease to humans 3. RVF virus has an incubation period of 2-7 days following infection.
The virus was first discovered in Kenya in 1930-31 although humans RVF cases were first reported in Uganda in 1968 5. Subsequently, Uganda reported RVF outbreaks in 2016 affecting both animals and humans in Kabale district, Western Uganda 6. Risk factors such as: trade of livestock between Uganda and its neighbouring countries 7, cattle movement from Isingiro, Kabale, Kisoro and Ntungamo, climatic conditions, temperatures, availability of bleeding ground for mosquitoes and abundance of wildlife and game reserves play a major roles in the spread of RVFV in Western Region of Uganda 8, 9 and 3.
On 25 June, 2018, Ministry of Health received a notification of a 49-year-old male confirmed for Rift Valley Fever by Uganda Virus Research Institute (UVRI) and later on at passed on in Bwera hospital, Kasese District. Subsequently, the Ministry of Health received other alerts from Ibanda, Mubende, Lwengo and Sembabule districts presenting with similar symptoms. We investigated to identify the scope of the outbreak, exposures factors and recommend evidence-based control measures.
Methods
We defined a suspected case as acute onset of fever (>38oC) with a negative malaria test, and ≥2 of the following symptoms: headache, myalgia, and any gastroenteritis symptom (nausea, vomiting, abdominal pain, diarrhoea) in any person from Mbarara, Sheema, Ntungamo, Kasese, Lyantonde, Rakai, Mubende, Isingiro and Ibanda districts from 1 June to 10 August 2018. We defined a Probable Case as; a suspect-ed case with thrombocytopenia OR low WBC counts OR raised haematocrit plus at least one of the following; unex-plained bleeding symptoms, such as bleeding from the nose, vomiting blood, coughing out blood (without history of TB), blood in stool, blood in urine. Sudden change in vision e.g. any of the following: blurred vision, poor vision, seeing floaters, pain in the eye, bilateral orbital pain, Jaundice and any unexplained death. A confirmed case was a suspect or probable case that is laboratory confirmed by either detection of RVFV nucleic acid by reverse-transcriptase polymerase reaction (RT-PCR) OR demonstration of serum IgM or IgG antibodies by ELISA.
We reviewed medical records in the affected districts and conducted a community case search to update the list. We conducted a matched case- control study matching on age, sex and neighbourhood for the thirteen case-persons. We collected blood samples from 16 suspected case-persons and samples were shipped to UVRI for analysis.
Results
We identified 21 case-persons, nineteen (19) confirmed and two (2) probable. The case fatality rate was 62% (13/21). The mean age of the case-persons was 35 (SD±11). Nine districts were affected during the outbreak. Isingiro District was the most affected district with an Attack Rate (AR= 1.6/100,000).
Distribution of occupation among case-Persons during the RVF outbreak in Uganda, July-August 2018
Majority of the case persons were farmers 37% (7/19), fol-lowed by butchers 26% (5/19), herdsmen 21% (4/19), and others (drivers and assistant commandant of Nakivaale refugee settlement, Isingiro District)
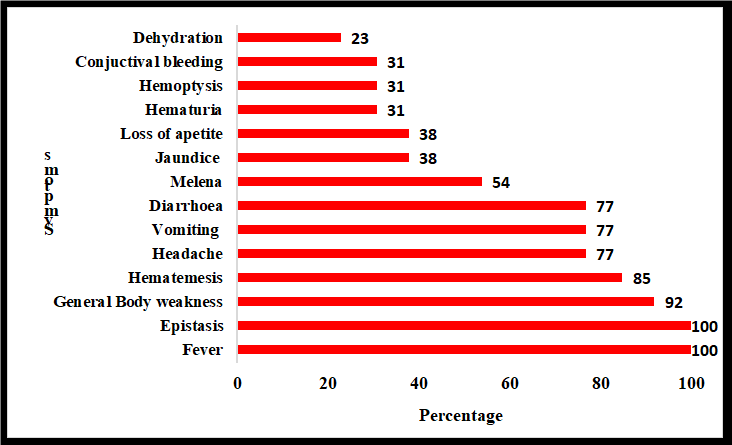
Distribution of symptoms among case-persons during the RVF outbreak, Uganda, July-August 2018
Majority of the case-persons presented with fever, general body weakness, headache, and diarrhea during the RVF outbreak in Uganda, July-August 2018.
Case classification and fatality rate per district during the RVF outbreak in Uganda, July 2018
Ntungamo, Rakai, and Kasese districts had 100% Case Fatality Rate (CFR), Mbarara district reported 75% CFR, Isingiro dis-trict, 55% CFR, Sheema 50%CFR while Ibanda, Lyantonde and Mubende reported 0% CFR.
Case Control Study Finding
Rift Valley Fever (RVF) infection occurred in 39% (7/18) of case-persons who participated in dissection of dead animals compared to 6.0% (5/90) of the control (ORc=11, 95% Fisher’s exact 2.4-50). In addition, 44% (8/18) of the case-persons who participated in cutting meat from sick animals developed RVF compared to 7.0% (6/90) of the controls (ORMH= 35, 95% CI 4.0-314). Also, 44% (8/18) of the case-persons who participated in cutting meat from dead animals compared to the controls 6.7% (4/90) developed RVF (ORC = 17, 95% CI Fisher’s exact 3.6-89). Similarly, 50% (9/18) of the case-persons who participated in cutting meat from sick or dead animals compared to controls 7.0% (6/90) developed RVF (ORMH=40, 95%CI 4.6-349). 50% (9/18) of the case-persons who were exposed to sick or dead animals compared to controls 7.0% (6/90) developed RVF infection (ORMH=40, 95%CI 4.6-349). 78% (14/18) of the case-persons who were exposed to health animals compared to the control 62% (56/90) developed RVF (ORMH=2.1, 95%CI 0.36-31), however, this was not significant
Laboratory findings
Seventeen (17) case-persons were confirmed positive for RVF. Seventy-two (72) animal samples turned positive for RVF.
Discussion
Our field epidemiologic investigation revealed that infection with RVF fever occurred during a rainy season and was associated with exposures to meat from sick and dead animals in eleven district in west and central Uganda. Environmental investigations showed the presence of heavy floods in affected districts, and selling of illegal meat from sick and dead animals. Case-persons who were reported in this outbreak presented with symptoms consistent with RVF infection.
The outbreak affected more males because of the nature of work they do which includes butchering, herding animals, and slaughtering animals which increases their risk of acquiring the infection. Persons below 35 years were more affected be-cause this is an active age-group which involved in activities that predispose them to the infection. This is in agreement with study conducted in Kenya which reported male sex is associated with RVF infections due to the occupation nature of the infections.10
Over the past 50 years, this is the largest RVF outbreak in Uganda with a case count of 68. The outbreak affected farmers, butchers, and herdsmen indicating the occupational nature of the disease. Previous studies too have also reported high-risk occupations for RVF infection, including abattoir workers, veterinary personnel, herdspersons, 18 and farmers16 . From our analysis, butchering and cutting meat from sick animals was associated in RVF infection. A study conducted in Uganda, 2016 found that working in the abattoir and slaughter house increased the risk of RVF infection 8. Also, a study conducted in Kenya in 2015 by LaBeaud et al reported that history of butchering livestock increased RVF seropositivity 10.
This outbreak reported a high case fatality rate compared to previous outbreaks. It could possibly be explained by delays in seeking medical care, delays in referrals, long distance encountered to refer patients. In addition, poor surveillance systems could have contributed to the high case fatality rate. Identification of cases took a little longer compared to previous outbreaks where prompt surveillance was done.
Preventive strategies for RVF infection have been pinned out which include; identification of the infected livestock (cows, sheep, goats and pigs), which mitigate disease spread to healthy animals and subsequently protecting humans who are in close contact with animals13. In addition, use of personal protective equipment, and thorough cooking of meat and milk before consumption has been documented19.
Limitations
Although it has been documented that aedes mosquitoes play a potential role in the transmission of RVFV, our study did not establish the possibility. Apart from establishing the presence of aedes mosquitoes, we didn’t establish for active virus infection in the mosquitoes. Given the wide scope of the affected area, it is possible that we did not identify all the case-persons hence underestimation of the magnitude of the outbreak.
Conclusions and recommendations
This was a propagated RVF outbreak caused by butchering meat, slaughtering animals and consuming roasted meat in Uganda. We recommended proper boiling of meat before consumption and inspection of all animals before slaughter. We recommend that one health approach should be adopted for effective control of RVF outbreaks in Uganda. The Ministry of Agriculture, Animal Industry and Fisheries should conduct routine surveillance for RVF infection in livestock and tighten meat inspection exercises. The Ministry of Health should be on the lookout of any suspected case and supportive care should be offered so reduce on mortality cases.
Public health actions
Based on our findings, the affected communities were sensitized on the dangers of eating meat from animals that are sick or have died of unknown causes, radio talk shows were also held in the affected communities, an isolation unit was set up at one of the health fours in the most affected district, and quarantine measures and meat inspection was strengthened.
References
1. Ly HJ, Lokugamage N, Nishiyama S, Ikegami T. Risk analysis of inter-species reassortment through a Rift Valley fever phlebovirus MP-12 vaccine strain. PLoS One. 2017. doi:10.1371/journal.pone.0185194
2. Peyre M, Chevalier V, Abdo-Salem S, et al. A Systematic Scoping Study of the Socio-Economic Impact of Rift Valley Fever: Research Gaps and Needs. Zoonoses Public Health. 2015. doi:10.1111/zph.12153
3. Tran A, Trevennec C, Lutwama J, et al. Development and Assessment of a Geographic Knowledge-Based Model for Map-ping Suitable Areas for Rift Valley Fever Transmission in Eastern Africa. PLoS Negl Trop Dis. 2016. doi:10.1371/journal.pntd.0004999
4. Reichler MR, Bur S, Reves R, et al. Results of testing for human immunodeficiency virus infection among recent contacts of infectious tuberculosis cases in the United States. Int J Tuberc Lung Dis. 6447;7(56 Suppl 7):S875-8.
5. Henderson BE, Mc Crae AWR, Kirya BG, Ssenkubuge Y, Sempala SDK. Arbovirus epizootics involving man, mosquitoes and vertebrates at lunyo, uganda 1968. Ann Trop Med Parasitol. 1972. doi:10.1080/00034983.1972.11686834

Comments are closed.