
Cholera outbreak caused by contaminated water spreads across 80 villages in endemic Kasese District, February to July 2015
Authors: Benon Kwesiga, Pande Gerald, Ario Alex Riolexus; Affiliation: PHFP Field Epidemiology Track
Summary
On 14th May 2015, the Ugandan Ministry of Health (MOH) sent out a central team to support the local cholera response team in the Western District of Kasese. The cholera outbreak had lasted two months since confirmation of the index cholera case on 14th March 2015. The team set out to epidemiologically characterize the outbreak, identify the mode of transmission and institute control measures. This cholera outbreak originated from Bwera Sub-County, a cholera prone area near the border with the Democratic Republic of Congo (DRC) where another cholera outbreak was ongoing. It gradually spread to over 80 villages across the district, affecting 183 people over a 6 months period (February to July 2015). A case control study revealed that drinking contaminated water was highly linked to developing the disease. Sources of drinking water in the affected areas including piped and stream/river water were heavily contaminated with fecal coliforms. Piped water was inadequately chlorinated and had increasing levels of fecal contamination along the pipeline and in households. The team recommended proper disposal of patients’ faeces, adequate chlorination of the piped water system and health education of the population which helped control the outbreak.
Background
On March 14th 2015, the District Health Officer (DHO) Kasese District notified MOH headquarters about a con- firmed cholera outbreak in the district. The initial cases registered were from two villages in Mpondwe/Lhubiriha Town council located near the Ugandan border with Democratic Republic of Congo (DRC). The first reported case, was a 12 year old boy from Nyabugando village, in Bwera Sub County whose symptoms had started on March 14, 2015. He tested positive by the cholera Rapid Diagnostic Test (RDT) on March 15th, 2015. We also learnt that the first cases had crossed the border to DRC where another cholera outbreak had been reported around the same time.
The first reported case, was a 12 year old boy from Nyabugando village, in Bwera Sub County whose symptoms had started on March 14, 2015. He tested positive by the cholera Rapid Diagnostic Test (RDT) on March 15th, 2015. We also learnt that the first cases had crossed the border to DRC where another cholera outbreak had been reported around the same time. However due to challenges in cross-border collaboration, it was difficult to fully investigate events on the DRC side. Despite efforts by the Kasese District team, the outbreak continued to spread across several villages in the district. On May 14th 2015 therefore, MoH assembled a team to support the local efforts in investigating and con- trolling the outbreak. The investigation team set out to epidemiologically characterize the outbreak, identify the mode of transmission and guide targeted control measures.
Methods
We conducted the study in Bwera and Kitswamba Sub Counties, in Kasese, a district in western Uganda. Bwera town is located 5 km from the Ugandan border with DRC where a big food market is located. There is a lot of cross border trading making it easy for contagious diseases to be transferred between the two countries. The district is composed of 20 rural sub-counties and 4 town councils. We defined a suspected cholera case as onset of acute watery diarrhoea in a Kasese District Resident from February 2015 onwards [1]. A Confirmed cholera case was defined as a suspected case with laboratory confirmed vibrio cholerae. To find cases systematically, we reviewed patient records. We conducted Laboratory testing on stool samples from Bwera hospital. Cases were tested with cholera Rapid Diagnostic Tests (RDTs) before confirmatory culture testing of a stool sample. To test the hypotheses generated from the descriptive analysis, we conducted a case – control study in the most affected areas of Bwera and Kitswamba Sub Counties.
Results
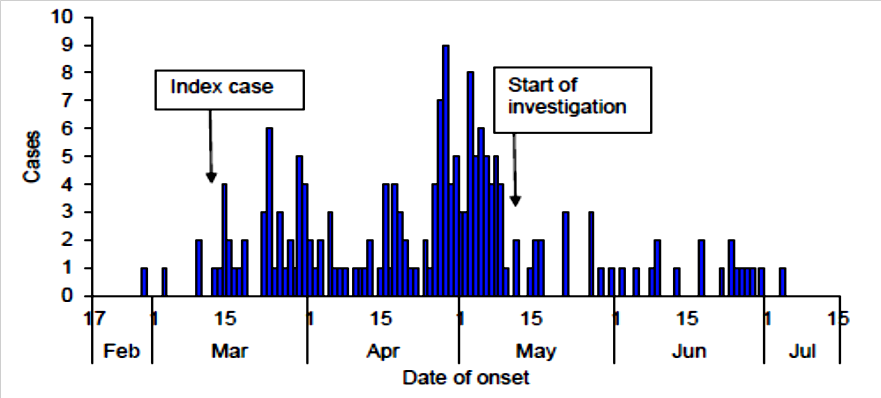
By June 30, 2015, 183 suspected cases had been documented in the district, with cases distributed in more than 80 villages throughout the district. Two sub counties: Bwera and Kitswamba were the most affected. Three cholera treatment centers were set up in these areas where all suspected cases were managed with intravenous fluid rehydration and antibiotics. The age range of the case-patients was 1-90 years; the sex ratio was approximately 1:1. The commonest symptoms were diarrhea (100%) and vomiting (46%). As illustrated by the epi-curve in figure 1, the outbreak lasted five months from February to July 2015.
On stratifying the epi-curve, it depicted small point source epidemics occurring in the different villages as the out- break spread. The main hotspot of the outbreak was Bwera where the sporadic cases were reported throughout the outbreak period. In Kitswamba the outbreak started approximately one and a half months after the index case in Bwera and lasted only one month. The outbreak started from Bwera Sub County in villages nearest to the DRC border, spread to Kasese municipality where it affected a few people before attacking Kitswamba Sub County. Figure 2 below shows the distribution of the affected villages across Kasese district. The highest attack rates were found in parishes within Bwera and Kitswamba.
Tests were conducted from Bwera Hospital laboratory and 61 samples tested culture positive for Vibrio cholerae. We conducted an environmental assessment of the area to assess for possible drivers of the outbreak. The most affected sub county, Bwera is located just near the border with DRC where a lot of cross border trading takes place. The main water supply for this area is a gravity flow scheme of water from River Rubiriha that marks the border between Uganda and DRC. The scheme provides two types of water. Treated water is paid for while untreated water is free. Tests done on the water found that both treated and untreated water were heavily contaminated with E. coli.
We also observed people washing cooking utensils in the water, children playing in the water and evidence of open defecation along the river banks. Our findings therefore suggested that water was the most likely mode of transmission. From the case control study, we found a significant association between drinking unsafe water (not boiled, treated or filtered) and get- ting sick. 94% (46/49) of case-patients and 76% (152/209) of controls drank water that was not treated, boiled, or filtered (ORM-H = 5.9, 95% CI: 1.6-21.5). Eating fish or buying it from various markets were not associated with illness.
Discussion and public health actions undertaken
This was the third cholera outbreak in Kasese since 2000 [2]. Like previous outbreaks, this one also began in Bwera Sub County. It was caused by consumption of contaminated drinking water. Although we could not elicit concrete evidence, it seems that the water was most likely contaminated by faeces from the first cases through open defecation followed by drinking the water without rendering it safe first by boiling, treating or filtering it. These could have led to the spread of the disease to household level [3, 4].
Having confirmed that water was the source of the outbreak and that the available water sources were contaminated, we sought for practical and immediate ways to provide safe drinking water to the affected communities Water treatment helps prevent up to 90% of water borne diseases including cholera [5]. At the time of this outbreak, the only safe water source was borehole water collected in a clean container. The river water in the affected areas was highly contaminated with faecal matter and thus unsafe to drink. Proper treatment of the piped water and proper disposal of faeces could have prevented this outbreak or at least greatly reduced its impact.
Primary prevention through improvement of sanitation and waste disposal as well as provision of safe water are the most effective and sustainable interventions for control of cholera in such a community. Prior experience in cholera outbreaks enabled the health workers to detect this outbreak in a timely manner. However there was a delay of more than a month be- tween confirmation of the first case and launching of a detailed outbreak investigation. If investigation and control measures had been initiated upon confirmation of the first cases, this could have possibly reduced the extent of the outbreak significantly.
During this outbreak, there was a concurrent outbreak on the other side in DRC. The District Health Team reported that the first cases came from DRC although this proved difficult to con- firm. This brought out a challenge of inadequate cross-border collaboration. This was later on addressed by linking the cholera response teams on the Uganda and DRC borders so as to work together and learn from each other. Eventually, through proper disposal of patients’ faeces, adequate chlorination of the piped water system, distribution of water treatment tablets and health education, we were able control this outbreak.
Acknowledgements
We would like to acknowledge all the efforts by the WHO team, the District Health Team, the health workers especially those in the CTCs, the Village Health Team members and Local Council chairmen in responding to this outbreak.
References
- Cummings, J., et al., A cholera outbreak among semi-nomadic pastoralists in northeastern Uganda: epidemiology and interventions. Epidemiol Infect, 2012. 140(8): p. 1376-85.
- Bwire, , et al., Cholera Surveillance in Uganda: An Analysis of Notifications for the Years 2007–2011. Journal of Infectious Diseases, 2013. 208(suppl 1): p. S78-S85.
- DAS, A., et al., Two sequential outbreaks in two villages illustrate the various modes of transmission of cholera. Epidemiology & Infection, 137(06): p. 906-912.
- Nguyen, D., et al., Cholera Epidemic Associated with Consumption of Unsafe Drinking Water and Street-Vended Water—Eastern Freetown, Sierra Leone, 2012. The American Journal of Tropical Medicine and Hygiene, 2014. 90(3): p. 518-523.
- WHO, World Health Organization cholera fact sheet.

Comments are closed.