
Cholera outbreak associated with drinking contaminated water from an open well-Kampala City, Uganda, January 2019.
Authors: Daniel Eurien1*, Angella Musewa1, Esther Kisakye1, Francis Ongole2, Benon Kwesiga1, Daniel Kadobera1, Alex Riolexus Ario1
Affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda
2Central Public Health Laboratories, Ministry of Health, Kampala, Uganda
Summary
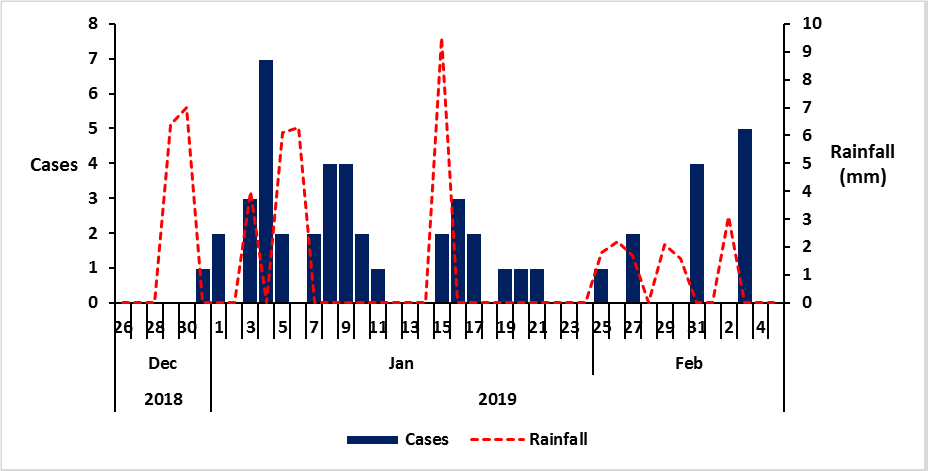
On 6th January 2019, the Ministry of Health was notified by the District Surveillance Officer Lubaga Division, of a suspected cholera outbreak in Sembule village that had reportedly killed two people. We investigated to identify the source and mode of transmission of the out-break, and recommend evidence-based interventions. We systematically identified cases by active search in the community and in three designated cholera treatment centers, conducted descriptive epidemiology and generated hypotheses. We conducted a case-control study in Sembule village, the epicenter of this outbreak in which we compared exposures during 28 December 2018 to 11 February 2019 among confirmed case-persons and asymptomatic controls, individually matched by age-group. We identified 50 case-patients, of which 22 were confirmed cases of V. cholerae O1, biotype El Tor serotype Inaba. The epidemic curve showed several point-source outbreaks following rains. Drinking water from open well W – naturally formed underground water puddles throughout the slums (OR M-H=21, 95% CI: 4.6–93) was a significant exposure. Drinking water from public stand tap (OR M-H = 0.33, 95% CI: 0.13–0.86) and drinking boiled water (OR M-H =0.15, 95% CI: 0.04-0.60) were significantly protective. The village had a token-operated water tap, which had broken down one month prior to the outbreak, and residents resorted to drink water from open well. Environmental assessment showed that residents emptied their faeces into the drainage channel connecting the open well. Water from a container in one of 8 households tested positive for V. cholerae; water from open well C had coliform counts ˃900MPN/100ml. We concluded that this outbreak was caused by drinking contaminated open well water. We recommended emergency chlorination of drinking water, fixing the broken public tap, closure of open well C, sensitization about the danger of drinking water from open well C, and improving latrines so they are not discharged into the drainage channel.
Introduction:
Cholera is a communicable disease with a short incubation period of a few hours to 5 days and has a high epidemic potential. It is a bacterial infection caused by Vibrio Cholerea and is mainly transmitted through consumption of food, or water contaminated with the bacteria (1). It commonly presents with profuse pain-less watery diarrhea, and vomiting (1). When untreated, about 5% of the case-persons die of severe dehydration.
Uganda is among the 51 cholera endemic countries. Cholera endemic countries are classified as those reporting confirmed cholera cases detected during the last 3 years with evidence of local transmission (1). Kampala city is among the three endemic cholera regions in Uganda, the other two being the western border districts with the Democratic Republic of Congo (DRC), and Karamoja region to the north east (2). Kampala city, like most cities in developing countries, is experiencing rapid urbanization leading to an increase in population, and rapid development of periurban (informal) settlements. More than 60% of the city’s population with low incomes resides in these settlements which have the lowest basic service levels (sanitation, water supply, solid waste collection, and storm water disposal) hence increased risk for hygiene related diseases including cholera (3) ,(4).
On 6th January 2019, the District Surveillance Officer Lubaga division in Kampala called the Emergency Operation Center at the Ministry of Health regarding a suspected cholera outbreak in his division. We investigated to estimate the scope of the outbreak, identify the mode of trans-mission, and recommend evidence-based control measures.
Methods:
We defined a suspected case as onset of pro-fuse, painless acute watery diarrhea in a Kampala City resident (≥2 years) from 28 December 2018 to 11 February 2019. A confirmed case was a suspected case with Vibrio cholera identified from the patient’s stool specimen by culture or Polymerase Chain Reaction (PCR). We found cases by record review and active community case finding. We conducted a case-control study in Sembule village, the epicenter for this outbreak to compare exposures among con-firmed case-persons and asymptomatic controls, matched by age-group. We also conducted an environmental assessment. We tested water samples from randomly selected households and water sources for total coliforms using the Most Probable Number (MPN) and PCR to identify the organism.
Results:
We identified 50 case-patients, of which 22 were confirmed cases of V. cholerae O1, biotype El Tor serotype Inaba, and 3 died (Case fatality rate=6%). Cases presented with watery diarrhea (100%), vomiting (68%), abdominal pain (12%), and fever (5.8%). The epidemic curve showed several point-source outbreaks following rains. All age-groups were affected; age-group 5–14 was the most affected (AR: 8.2/100,000). All the five divisions were affected. Lubaga Division was most affected (attack rate [AR]: 6.5/100,000), all cases were from Sembule village. Affected households from Sembule village drank water from open wells after their stand pipe tap broke down in December 2018. In the case-control investigation, 83% (15/18) of case-persons compared to 18% (16/90) of control-persons drank water from well X(OR M-H=21, 95% CI: 4.6–93) (Figure 1). However, 28% (5/18) of case-persons com-pared with 69% (62/90) of control persons drank water from a public stand tap (OR M-H = 0.33, 95% CI: 0.13–0.86); 33 % (6/18) of case-persons compared with 66% (59/90) of control persons drank boiled water (OR M-H =0.15, 95% CI: 0.04-0.60). The village had a token-operated water tap, which had broken down one month prior to the outbreak, and residents resorted to drink water from open well X. Environmental assessment showed that residents emptied their faeces into the drainage channel connecting the Open well X. Water from a container in one of 8 house-holds tested positive for V. cholerae; water from open well X had coliform counts >900MPN/100ml.
Figure 1: Distribution of symptom onset dates of cholera cases: Kampala City, Uganda, December to January 2019
Meteorological data showed that heavy rainfall preceded peaks of the cholera outbreak. Despite implementation of interventions including community awareness campaigns and distribution of chlorine to households, the number of cases continued after subsequent rainfall. There were no new cases following stoppage of community members from using the implicated well water.
and distribution of chlorine to households, the number of cases continued after subsequent rainfall. There were no new cases following stoppage of community members from using the implicated well water.
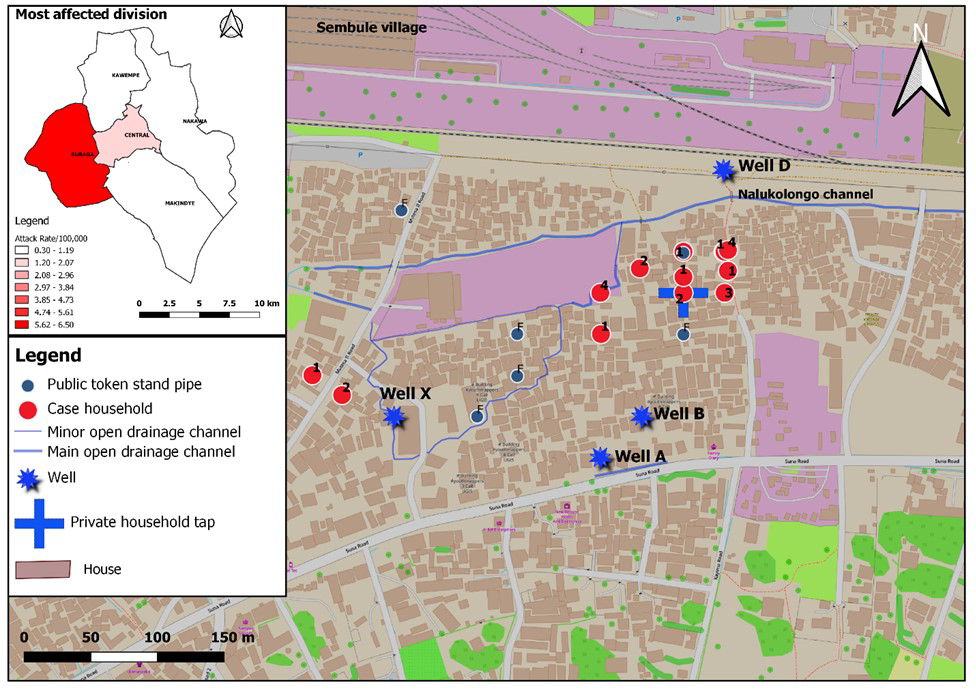
All the five divisions were affected (inset map), with Rubaga Di-vision being the most affected (AR: 6.5/100,000) followed by Central Division (AR: 2.1/100,000). All the affected case-persons in Rubaga Division were in Sembule village where the first cases were reported (Figure 2).
Discussion:
Our investigation revealed that the cholera outbreak in Sembule village was caused by drinking well water contaminated by flooding from open drainage channels after rainfall. Prior to this outbreak, there was reported unconfirmed cholera outbreak in the neighboring Katwe village. Therefore, cholera might have been introduced into Sembule village by one or multiple visitors carrying the bacteria, causing the initial infections. The initial case-patients also likely released feces from their pit latrines onto the drainage channel, a practice common in slum areas where latrines are emptied into open drainages during heavy rains. Heavy rainfall subsequently washed the case-patients’ feces released from latrines onto drainage channels that flooded the wells, consequently contaminating the water. Residents collected the contaminated well water after the flood receded and drank it without boiling or treating it, causing the outbreak.
Globally, poor water and sanitation conditions have been implicated in several waterborne disease outbreaks including typhoid and cholera (7, 8). Cities in Sub-Saharan Africa particularly at a high risk because many have registered high population growth rates in recent years, without corresponding in-crease in access to improved water and sanitation facilities (9, 10). Consequently, outbreaks of waterborne diseases including cholera occur frequently and mostly precipitated by rains (11,12). In Uganda, cholera outbreaks in the capital Kampala mostly occur in slum dwellings usually characterized by over-crowding with insufficient clean water and poor sanitation facilities (13). Investigations of cholera outbreaks in different parts of Uganda revealed that the outbreaks were caused by drinking contaminated untreated water (14). Contamination usually results from poor planning and inadequate enforcement of the Public Health Act in slum areas. Many cholera outbreaks in Uganda have not been investigated epidemiologically, and most times die out after the implementation of general interventions (15). The inability to investigate all past cholera outbreaks presented a missed opportunities to generate specific-evidence based interventions that could have helped prevent subsequent outbreaks. Our investigation was able to provide actionable evidence on the ways well water was contaminated following release of fecal matter from latrines after rains. We were also able to demonstrate the safety of the public piped water system. This information informed Kampala Capital City Authority and National Water and Sewerage Corporation to implement immediate interventions to stop the outbreak and long-term interventions to prevent future outbreaks of cholera and other water-borne diseases.
The main limitation of our study was the inability to link the possible source of the initial contamination to the outbreak.
Conclusions and recommendations:
This outbreak was caused by drinking contaminated open well water. We recommended emergency chlorination of drinking water, fixing the broken public tap, closure of open well X, sensitization about the danger of drinking water from open well, and improving latrines so they are not discharged into the drainage channel.
References
1.World Health Organisation cholera fact sheet [Internet]. [cited 2019 Jan 14]. Available from: https://www.who.int/news-room/fact-sheets/detail/cholera
2.Bwire G, Malimbo M, Maskery B, Kim YE, Mogasale V, Levin A. The Burden of Cholera in Uganda. PLoS Negl Trop Dis [Internet]. 2013 Dec 5 [cited 2019 Jan 14];7(12). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3855006/
3.2014 National Census Main Report.pdf [Internet]. [cited 2019 Jan 21]. Available from: http://www.ubos.org/onlinefiles/uploads/ubos/NPHC/2014%20National%20Census%20Main%20Report.pdf
4.Kulabako RN, Nalubega M, Wozei E, Thunvik R. Environmental health practices, constraints and possible interventions in periurban settlements in developing countries – a review of Kampala, Uganda. International Jour-nal of Environmental Health Research. 2010 Aug 1;20(4):231–57.
5. Katukiza AY, Ronteltap M, Oleja A, Niwagaba CB, Kansiime F, Lens PNL. Selection of sustainable sanitation technologies for urban slums–a case of Bwaise III in Kampala, Uganda. Sci Total Environ. 2010 Dec 1;409(1):52–62.

Comments are closed.