Cholera outbreak associated with consumption of contaminated lake water at Kasensero landing site, Kyotera District, April–May 2024
Authors: Bridget Ainembabazi1*, Emmanuel Mfitundinda1, Joyce Owens Kobusingye1, Tracy Rutogire1, Shem Mwebaza1, Paul Edward Okello1, Benon Kwesiga1, Richard Migisha1, Joseph Giriman2, Alex Riolexus Ario1; Institutional affiliation: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda 2Kyotera District Local Government, Kyotera, Uganda; Correspondence*: Tel: +256700375907, Email: bainembabazi@uniph.go.ug
Summary
Background: On May 5, 2024, a cholera outbreak was confirmed at Kasensero landing site in Kyotera District. We investigated to determine the source, magnitude, and risk factors associated with the outbreak to inform control and prevention measures.
Methods: We defined a suspected case as the onset of watery diarrhoea in a resident (aged ≥2 years) of Kasensero landing site from 1 April to 24 May 2024. A confirmed case was a suspected case with a positive stool culture for V. Cholerae. We reviewed health facility records and conducted active case search in the community with the help of local leaders. We conducted descriptive epidemiology and environmental assessment to generate a hypothesis. We conducted an unmatched case-control study and identified risk factors using logistic regression.
Results: We identified 64 cases (9 confirmed and 55 suspected) with an attack rate (AR) of 12/1,000 and a case fatality rate of 3% (2/64). The median age was 35 (IQR: 27-42 years). Males (AR=12.5/1000) and females (AR=11.4/1000) were similarly affected. Kimwanyi parish was the most affected parish with 44 cases (AR=45/1,000). We observed latrines with compromised sub-structures, open defecation, and flooding at the landing site. There was general contamination of the lake water caused by the rains and flooding. The floating vegetation on the lake resulted in the stagnation of the lake water. This could have sustained contamination of lake water which is the main source of livelihood at the landing site. The use of lake water for domestic purposes was significantly associated with cholera (aOR=4.0; 95% CI: 1.8–8.6). Boiling drinking water (aOR=0.4; 95% CI: 0.2–0.8) was protective.
Conclusions: The outbreak was associated with drinking unboiled/untreated lake water contaminated by faecal matter and stagnated by floating vegetation. We recommended boiling or treating lake water and construction of recommended pit latrines at the landing site.
Introduction
Over 1.3 billion people are at risk of cholera in endemic countries (1). The disease still affects at least 47 countries across the globe, resulting in an estimated 2.9 million cases and 95,000 deaths per year worldwide (1, 2). Sub-Saharan Africa accounts for 60% of the global burden of cholera (1). In Uganda, 11,030 cases of cholera were reported during the 2011 – 2016 period through the Ministry of Health, Health Management Information System disease surveillance data base (3).
Cholera is a preventable and treatable acute diarrhoeal disease caused by infection of the intestine with the bacterium Vibrio cholerae, either serogroup 01 or 0139 (4, 5). It is usually transmitted through consumption of water or food contaminated by faeces containing Vibrio cholerae (6). It remains a major public health threat in communities with poor sanitation and limited access to safe water for domestic use. It is common in congested settlements such as landing sites and refugee camps. Cholera affects all age groups. About 20% of those infected develop acute, watery diarrhoea and 10-20% of these develop severe dehydration. The incubation period is short (2 hours to 5 days), thus creating an opportunity for quick raise in cases. The case fatality rate (CFR) among untreated cases may reach 30-50%, while it can go as low as less than 1% with appropriate management. Recommended treatment for Cholera is rehydration and appropriate antibiotics since they reduce the shedding of bacteria and reduce the duration of infection.
A cholera outbreak is defined by the occurrence of at least one confirmed case of cholera and evidence of local transmission (2). The first cholera outbreak in Uganda occurred in 1971, and several cholera cases have been reported since then (7-11). In areas with sustained (year – round) cholera transmission, outbreaks are defined as an unexpected increase (in magnitude or timing) of suspected cases over two consecutive weeks of which some are laboratory confirmed (2).
On 26th April 2024, Kyotera District received an alert from Kasensero Health Centre II regarding the death of a fisherman from severe dehydration one day after returning from a fishing trip. He had suddenly developed vomiting and acute watery diarrhoea while fishing, and was returned by his colleague severely prostrated. An increased number of cases of acute watery diarrhoea were also reported in the community. On 5th May, 2024, stool culture and sensitivity results from the Central Public Health Laboratories confirmed Vibrio cholerae. Kasensero landing site had last reported a cholera case over twenty years ago. We determined the source of the outbreak, its magnitude, and risk factors to inform control and prevention measures.
Methods
Outbreak area
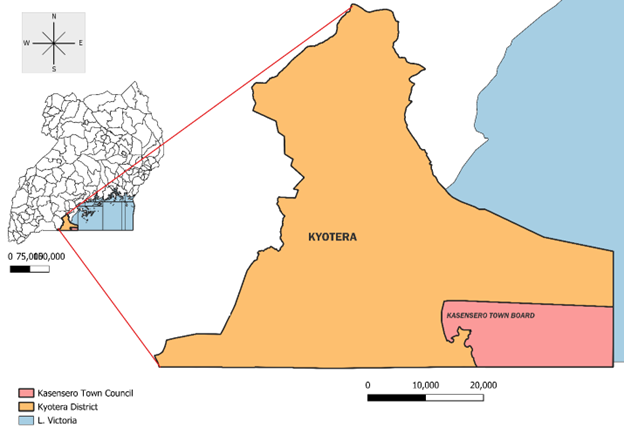
The outbreak occurred at Kasensero landing site, which is located on the western shore of Lake Victoria, in Kyotera District, South Central Uganda (Figure 1). It is located a short distance from the Uganda border with Tanzania, with 60% of the population either being Tanzanian or having roots in Tanzania. It is a Point of Entry through which traders, fishermen, and travellers from East African countries access Uganda. The main economic activity in the area is fishing. The landing site has a population of approximately 5,000 inhabitants.
It has five parishes (wards) and eleven villages (cells). It is located next to Kyeebe sub-county, all in Kakuuto county.
Case definition and finding
We defined a suspected case as onset of watery diarrhoea in a resident (aged ≥2 years) of the Kasensero landing site, Kyotera district from 1 April to 24 May 2024. A confirmed case was defined as a suspected case with a positive culture for V. Cholerae from a stool sample. Cases were identified through health facility records review and active case search in the community with the help of local leaders.
Descriptive epidemiology
We conducted a descriptive analysis of the cases identified by age, sex, clinical presentation, place of residence, and possible risk factors. We calculated attack rates by place (parish) and sex using the 2014 population estimates obtained from the Kyotera district Biostatistician. An epidemiological curve was used to describe the distribution of cases by dates of symptom on set.
Laboratory investigations
We collected stool samples from 38 suspected cases for laboratory confirmation.
Environmental assessment
We observed sanitation and hygiene practices, including the disposal of human faeces in the community. We inspected water collection sources and observed water collection practices. We also observed the nature and state of the sewerage system.
Hypothesis generation
We interviewed the first 30 cases using a case investigation form to collect information on potential risk factors including sources of water, drinking water preparation practices, presence of a latrine at home, travel outside the place of residence, and food storage practices.
Case-control study
We conducted an unmatched case-control study to test the hypothesis, in which we interviewed 60 cases and 120 controls. We defined a control as a resident of Kasensero landing site, aged ≥ 2 years with no history of acute watery diarrhoea from 1 April 20204 to 24 May 2024. Controls were randomly selected, focusing on Kimwanyi parish, which was the most affected parish. We administered a standard questionnaire to both cases and controls. We asked about their sources of drinking water, water for domestic use, food last eaten, methods of water preparation before drinking, storage of water and food, use of latrines/toilets and history of travel. We used logistic regression to identify factors associated with cholera transmission.
Ethical considerations
This investigation was in response to a cholera outbreak. The Ministry of Health of Uganda gave the directive to investigate this outbreak. The Office of the Associate Director for Science at the Center for Disease Control and Prevention (CDC) Uganda determined that this research did not involve human subject research and that its primary intent was public health practice or disease control. Verbal informed consent was obtained from participants or, if the interviewee was a minor, guardians before the start of each interview.
Results
Descriptive epidemiology
We identified 64 cases (9 confirmed cases and 55 suspected) with an attack rate (AR) of 12/1,000. There were two deaths: case fatality rate (CFR=3%). The median age was 35 (IQR: 27-42 years). Males (AR=12.5/1000) and females (AR=11.4/1000) were similarly affected. Kimwanyi Parish was the most affected parish with an attack rate of 42.2/1,000. Attack rates for the other parishes were as follows; Central A (4.3/1,000), Central B (9/1,000), Kagera A (2.6/1,000), Kagera B (2.9/1,000).
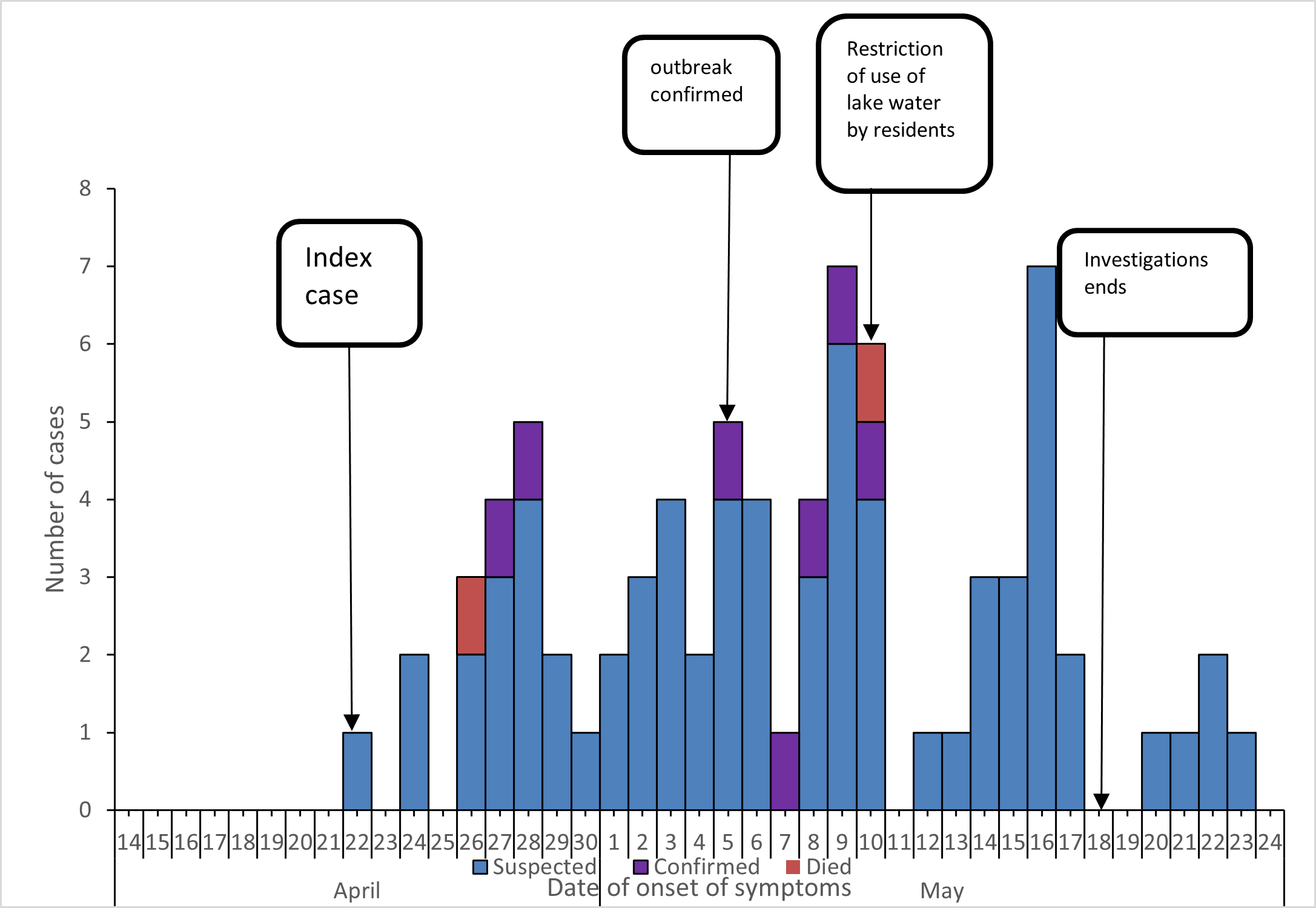
The epidemic curve shows that after the onset of the disease on April 22, a point source outbreak occurred up to April 28, followed by continuous community transmission for three weeks. There were four peaks during the outbreak; the last two higher than the first two. The final peak occurred on May 16, followed by a sharp decline to one or no cases per day until the outbreak ended (Figure 2).
Environmental findings
There was a piped water system that runs from Sekaningo to Kasensero town, and exists under the Central Umbrella of Water and Sanitation Authority under the Ministry of Water and Environment. It covered parts of the most affected village, cell 5. One water point was damaged following the flooding leading to damage to the pipeline extension to the point. A new water point was not set up to replace the abandoned one. The number of water points in use and accessible could not be established. Some households were fetching water from the lake for domestic use.
There was one public toilet (3 stances for women and 3 stances for men) available constructed by the town council and managed by a service provider at a fee of UGX 200 per use. There were at least 6 household latrines (raised and drainable). The water table is very high and limits depth of pit latrines leading to the option of using raised latrines which are expensive. All the household latrines reviewed were old and very likely to have leaking chambers to the ground water due to structural integrity of the latrine sub structure.
The area was flooded as the water levels had risen, and entered some houses close to the lakeshore. With limited access to latrine use due to distance or lack of household latrine or inability to pay the convenience fee, there were reported cases of open defaecation. We also found human faeces in the community and in the flooded water. There was floating water vegetation causing stagnation of contaminated water from the community at the lake shore.
Hypothesis generation
Out of 30 cases, 16 (53%), depended on lake water for domestic use, 29 (93%) did not have a pit latrine at home, and only 5 (17%) had travelled outside Kasensero within two weeks before the onset of the disease. Based on the results of the descriptive analysis, we hypothesized that the outbreak was associated with the consumption of contaminated and untreated Lake Victoria water by residents at Kasensero landing site.
Case-control study results
Residents who collected their water from the lake were four times more likely to develop cholera compared to those who collected their water from other sources like taps or rainwater (aOR = 4.0, 95% CI: 1.8 – 8.6). Additionally, those who boiled their drinking water were 60% less likely to develop cholera (aOR = 0.4 CI: O.2 – 0.8) (Table 1).
Table 1: Risk factors for cholera among residents of Kasensero landing site, Kyotera District, April–May 2024
| Exposure | Exposure | Cases
n (%) |
Controls
n (%) |
cOR
(95% CI) |
aOR
(95% CI) |
||
| Source of water for domestic use | Others (tap water and rain water) | 20 | (44) | 170 | 56 | Ref | Ref |
| Lake water | 40 | (28) | 50 | 47 | 2.8 (1.5-5.4) | 4.0 (1.8-8.6) | |
| Using a toilet in a home | No | 51 | (40) | 77 | 60 | Ref | Ref |
| Yes | 09 | (18) | 40 | 82 | 0.3 (0.15-0.8) | 0.3 (0.1-0.7) | |
| Preparation of drinking water | Others (leave to settle, filtered) | 22 | (44) | 28 | 56 | Ref | Ref |
| Boiling | 25 | (22) | 89 | 78 | 0.4(0.2-0.7) | 0.4(0.2-0.8) | |
CI: confidence interval, cOR: crude odds ratio, aOR: adjusted odds ratio
Discussion
This cholera outbreak was associated with drinking contaminated unboiled/untreated lake water. The source of V. cholerae in this outbreak was not determined. The landing site had recently experienced heavy rainfall, and there was flooding of the area. Additionally, there was floating vegetation for the duration of the outbreak, along the lake shores. This vegetation caused stagnation of the lake water that was contaminated from the community. The residents collected contaminated lake water near the lake shore and drank it without treating it causing the outbreak.
Previous outbreaks in Uganda and other African countries have also been associated with drinking contaminated lake water (10, 13). Landing sites and town slums are among the major outbreak prone areas in the country (10). Other cholera outbreaks in Africa have been associated with drinking contaminated river water, eating at large gatherings, and eating left over food (11, 14, 15).
Study limitations
We were not able to identify how the index case acquired the infection to prevent outbreaks.
Conclusion
This outbreak was associated with consumption of contaminated lake water, stagnated by floating vegetation. The water was likely contaminated by introduction of faeces through practices like open defecation. To prevent future similar outbreaks, we recommended construction of more taps to ensure access to safe water by the landing site residents, construction of pit latrines adequate for the high-water level at the landing site by the local authorities, and subsiding fees for access to the public toilets.
Public health actions
To stop the propagation of the outbreak, we conducted health education on cholera prevention and use of safe water for domestic use. We educated residents and encouraged them to use chlorine releasing tablets that had been provided, to make water safe for consumption. There were few taps in the area, and the use of tap water was limited by the associated cost. Health care workers were trained on Infection Prevention and Control practices (IPC) and case management; they were also trained on local preparation of Oral Rehydration Salts (ORS).
Recommendations
In the short term, we recommended review of access to the public toilet by the local authorities through suspension or subsidizing the user fees. We also recommend that the government, in partnership with the local authorities provide free safe water at the landing site since only a few taps were available and most of the residents were not able to afford the cost daily. In the long term, we recommend construction of more toilets at the landing site since most residents cannot afford to construct the recommended toilets due to the high-water tables. The government in partnership with the local authorities should also engage the water department and the umbrella scheme responsible for the tap water supply in the area to review the requirements for new applicants and reduce the associated cost.
Conflict of interest
The authors declare that they have no conflict of interest.
Authors’ contributions
BA, EM, and JOK designed the study and contributed to data collection and analysis. TR, SM, and JG also contributed to the study design and data collection. BA led the writing of the bulletin. TR, SM, PEO, RM, BK, and ARA participated in the writing of the bulletin and review to ensure scientific integrity. All authors contributed to the final draft of the bulletin.
Acknowledgments
The authors would like to thank the Kyotera District Health Team, Kasensero HC II administration and staff, and the community members of Kasensero landing site for their support in active case search and line listing of cases during this investigation.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Ali M, Nelson AR, Lopez AL, Sack DA. Updated global burden of cholera in endemic countries. PLoS neglected tropical diseases. 2015;9(6):e0003832.
- GTFCC. Ending Cholera: A Global Roadmap to 2030.30.
- Bwire G, Ali M, Sack DA, Nakinsige A, Naigaga M, Debes AK, et al. Identifying cholera” hotspots” in Uganda: An analysis of cholera surveillance data from 2011 to 2016. PLoS neglected tropical diseases. 2017;11(12):e0006118.
- Azman AS, Rudolph KE, Cummings DA, Lessler J. The incubation period of cholera: a systematic review. Journal of Infection. 2013;66(5):432-8.
- Deen J, Mengel MA, Clemens JD. Epidemiology of cholera. Vaccine. 2020;38:A31-A40.
- WHO. Cholera. World Health Organization; 2023 11th December 2023.
- Bwire G, Munier A, Ouedraogo I, Heyerdahl L, Komakech H, Kagirita A, et al. Epidemiology of cholera outbreaks and socio-economic characteristics of the communities in the fishing villages of Uganda: 2011-2015. PLoS neglected tropical diseases. 2017;11(3):e0005407.
- Kwesiga B, Pande G, Ario AR, Tumwesigye NM, Matovu JK, Zhu B-P. A prolonged, community-wide cholera outbreak associated with drinking water contaminated by sewage in Kasese District, western Uganda. BMC public health. 2018;18:1-8.
- Pande G, Kwesiga B, Bwire G, Kalyebi P, Riolexus A, Matovu JK, et al. Cholera outbreak caused by drinking contaminated water from a lakeshore water-collection site, Kasese District, south-western Uganda, June-July 2015. PloS one. 2018;13(6):e0198431.
- Oguttu DW, Okullo A, Bwire G, Nsubuga P, Ario A. Cholera outbreak caused by drinking lake water contaminated with human faeces in Kaiso Village, Hoima District, Western Uganda, October 2015. Infectious diseases of poverty. 2017;6:1-7.
- Okello PE, Bulage L, Riolexus AA, Kadobera D, Kwesiga B, Kajumbula H, et al. A cholera outbreak caused by drinking contaminated river water, Bulambuli District, Eastern Uganda, March 2016. BMC infectious diseases. 2019;19:1-8.
- Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. The Lancet infectious diseases. 2005;5(1):42-52.
- Birmingham ME, Lee LA, Ndayimirije N, Nkurikiye S, Hersh BS, Wells JG, et al. Epidemic cholera in Burundi: patterns of transmission in the Great Rift Valley Lake region. The Lancet. 1997;349(9057):981-5.
- Swerdlow D, Malenga G, Begkoyian G, Nyangulu D, Toole M, Waldman R, et al. Epidemic cholera among refugees in Malawi, Africa: treatment and transmission. Epidemiology & Infection. 1997;118(3):207-14.
- Gunnlaugsson G, Einarsdóttir J, Angulo F, Mentambanar S, Passa A, Tauxe R. Funerals during the 1994 cholera epidemic in Guinea-Bissau, West Africa: the need for disinfection of bodies of persons dying of cholera. Epidemiology & Infection. 1998;120(1):7-15.
- Bwire G, Waniaye JB, Otim JS, Matseketse D, Kagirita A, Orach CG. Cholera risk in cities in Uganda: understanding cases and contacts centered strategy (3CS) for rapid cholera outbreak control. Pan African Medical Journal. 2021;39(1).


Comments are closed.