Application of 7-1-7 matrix in a One Health context during the first anthrax outbreak in Kanungu district, Southwestern Uganda, September 2024
Institutional affiliations: Hannington Katumba1*, Charity Mutesi1, Bridget Ainembabazi1, Hellen Nelly Naiga1, Richard Migisha1, Aloysius Tumwesigye2, Birungi Mutahunga Rwamatware2, Benon Kwesiga1, Hilda Tendo Nansikombi1, Alex Riolexus Ario1 Author: 1Uganda Public Health Fellowship Program-Field Epidemiology Track, Uganda National Institute of Public Health, Kampala, Uganda, 2Kanungu District Local Government, Uganda *Correspondence: Tel: +256 777 538911, hkatumba@uniph.go.ug
Summary
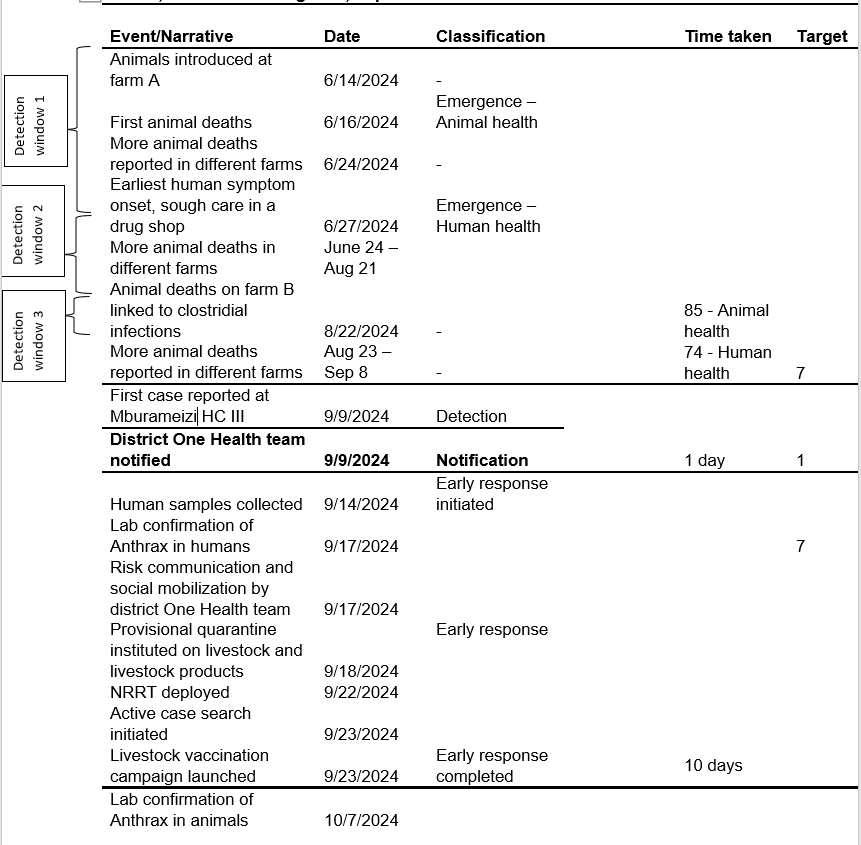
Background: In 2021, Uganda adopted the 7-1-7 framework which stipulates outbreak detection in 7 days, notification in 1 day, and completion of early response actions in 7 days. We used the 7-1-7 approach to assess response to the first known anthrax outbreak in Kanungu District following its confirmation on September 17, 2024.
Methods: We used the 7-1-7 metrics to document the dates of emergence, detection, notification, and completion of early response actions. We held discussions with the district leadership, health workers, and community members to establish key dates and facts, and to identify bottlenecks and enablers. Qualitative data were organized into themes to capture bottlenecks and enablers.
Results: The disease emerged in animals on June 15, 2024 and was detected after 85 days. In humans, the time from emergence (June 26, 2024) to detection was 77 days. The district One Health Team was notified 1 day after detection. Early response actions were jointly initiated after 5 days and completed in 13 days for human health, and in 14 days for animal health. Enablers for immediate notification included presence of a real-time One Health communication platform for health workers. Bottlenecks included weak zoonotic disease surveillance characterized by understaffing, low suspicion index for anthrax, and weak coordination with private health facilities.
Conclusion: Response to the first known anthrax outbreak in Kanungu District met only 1 (notification) of the 3 the 7-1-7 timeliness metrics because of the presence of a real-time one health communication platform. There was delayed detection and response largely due to low suspicion index among health workers and weak zoonotic disease surveillance. The district health team should strengthen One-Health and event-based surveillance at community level to enhance early detection and response activities to avert human fatalities and economic losses.
Introduction
With the increased globalization, it is imperative that any public health emergencies be identified and dealt with in time in order to minimize morbidity and mortality through timely implementation of disease prevention and control measures [1]. The 7-1-7 framework is recommended as a standard tool for assessing timeliness of response to public health emergencies. It stipulates detection of public health emergencies within 7 days from date of emergency, one day for a notification to me made to the authority responsible for action, and 7 days for completion of early response activities[11, 12].
Anthrax is a priority zoonotic disease in Uganda, targeted for multisectoral collaboration in surveillance and response [10, 14]. Despite this, outbreaks of anthrax continue to occur in different regions of the country, with a number of districts experiencing repeated or sustained anthrax outbreaks while some districts experienced anthrax outbreaks for the first time [15-20]. Kanungu District experienced its first ever anthrax outbreak in September 2024. The outbreak was associated with 111 animals that died suddenly, 90 cases of human anthrax including 4 confirmed cases and 6 deaths. We assessed the timeliness of detection, notification, and response to the first anthrax outbreak in Kanungu District, using the 7-1-7 metrics to identify bottlenecks, enablers, and lessons learned in managing outbreak of a priority zoonotic disease in a rural district in Uganda.
Methods
Outbreak setting:
Kanungu District is located in Kigezi region, Southwestern Uganda. It is home to some sections of the Bwindi Impenetrable National Park (BINP) in the south and the Ishasha sector of the Queen Elizabeth National Park (QENP) in the North and North East (Figure 1).
The district has several livestock farms, including communal grazing areas, and is a gate-way for movement of livestock and livestock products to the Democratic Republic of Congo (DRC). The district has a District One Health Team (DOHT), which has been in place for about 2 years.
Study variables and data collection: To establish facts on key dates and events, we interviewed health workers, field veterinarians, and community members using the 7-1-7 metrics. We noted the dates of emergence in both animals and humans. We also noted the dates when the outbreak was detected, when notification to the district health authorities was done. Additionally, we documented the dates early response was initiated and when the 7 and early response actions were completed. We then held discussions with the district technical, political and administrative leadership to identify the bottlenecks and enables in the outbreak response and further validate the information obtained from the field.
Data processing:
For the qualitative data, we used 2 different members of the investigation team, proficient in the local language (Runyankole-Rukiga) to listen to audio recordings and analyze the information in each sentence and obtain consensus on the challenges and enablers as highlighted by the respondents. We presented the findings and quoted verbatim some representative statements obtained from respondents.
Ethical approval and consent to participate: We conducted this study in response to a public health emergency and as such it was determined to be non-research. The MoH authorized this study and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. §§See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq. We obtained permission to investigate from the Kanungu District Local Government health authorities. We obtained verbal consent from all the respondents aged ≥ 18 years and there were no respondents under 18 years of age. Participants were assured that their participation was voluntary and that there would be no negative consequences for declining to participate or withdrawing from the investigation. Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, only accessible to the investigation team.
Result
7-1-7 assessment
Detection in animal health: From the earliest sudden animal deaths until when anthrax was first recorded in the system at Mburameizi health center III, there was a time gap of 85 days. The initial animal deaths on farm X were never reported to the veterinary health team. Some farms vaccinated their livestock against clostridial infections, as anthrax was not suspected in animals until it was detected in humans. From interviews with key informants we found that this was the first time to interface with anthrax and this contributed to its late detection by the surveillance system.
I studied about anthrax in school, but I have never seen any animal that has died of anthrax. (Farm manager-)
Animals have been dying from time past, and they are usually healthy-looking animals. In such cases, we usually suspect black quarter. In fact, around August, some farmers vaccinated their herds against black quarter after it had been confirmed by lab on one of the farms” (District Veterinary Officer, KDLG)
Detection in Human Health: The earliest date of symptom onset was June 27, 2024. This outbreak was later detected on September 9, 2024, at Mburameizi Barracks Health Center III. Considering that there were already reports of livestock deaths in in neighboring farms, admission of patients with suggestive symptom for anthrax raised suspiscion, after 74 days. One of the case persons reported history of rearing livestock, and slaughter and trade of meat of animals that had died suddenly. One of the case persons was quoted thus:
I used to head about anthrax from old people, but at my age, I have never seen anyone with the disease (case person Mburameizi subcounty)
Notification: The notification was immediate (one day). Once anthrax was detected at Mburameizi HC III, a notification was sent to the district One Health Team, who are regularly in touch with the health facility through the district surveillance focal person The district has a whatsapp group that is meant for surveillance. Health related information is regularly posted by different health workers from different health facilities in the district.
“We have a whatsapp group where different health workers all-over the district share information. This helps us to know what is happening in different facilities in real time” (In-Charge, Mburameizi Health Center III).
Response
Early response actions were completed in 14 days. As more cases were reported at the same health facility, the DHT was promoted to follow up on these alerts. Once the alerts were verified, a district laboratory team was dispatched to pick samples from these case persons on September 14, 2024. This marked initiation of the early response activities, 5 days after notification.
Laboratory results were received by the district on September 17, 2024, 3 days after sample collection, and anthrax outbreak as confirmed in humans. Immediately the district team launched a joint (One Health) risk communication campaign by means of radio talk shows.
“Anthrax is a serious disease that can cause serious disruption in the livelihood of communities. Once it was confirmed we had to act fast” (District Health Officer, Kanungu DLG).
The national rapid response team was deployed to support case investigation and other response activities on September 22, 2024. A mass livestock vaccination against anthrax was launched on September 23, 2024, targeting the most affected subcounties, completing the early response actions (Table 1).
Table 1: Time characteristics and 7-1-7 assessment of an anthrax outbreak in Kanungu district, Southwestern Uganda, September-October 2024
Discussion
Our study assessed the timeliness of detection, notification, and response to the first known anthrax outbreak in Kanungu District in South Western Uganda, right from the community level, to the district level. The disease was detected after 85 days in animals and 77 days in humans. A notification was immediate (one day) and early response actions were completed in 14 days. We identified 3 missed windows of opportunity during which the outbreak could have been detected earlier. The district had a real-time One Health communication platform that facilitated immediate notification. The assessment revealed a major gap in routine surveillance in the veterinary sector and the one health framework in the outbreak district. We highlight the importance of strengthening district One Health teams for integrated surveillance and early detection of public health emergencies, and the need for capacity building to enhance health worker suspicion index particularly regarding zoonotic diseases.
Study limitations
All the data collected were qualitative, heavily relying on the respondents to recall events as far as 3 months back. This could have led to inaccuracies in the data collected, likely leading to wrong estimation of dates of onset, the number of cases, or the interpretation of information provided by the respondents. We therefore used different investigation team members to independently analyze the obtained from respondents. Further validation was obtained by corroboration with information obtained from district leadership, and quantitative data obtained from outbreak investigation and response.
Additionally, the 7-1-7 approach has not yet been launched in the Uganda Animal health surveillance system. Our aim was to highlight it its utility in a One-Health context, in support of strengthening collaboration between the One Health sectors during routine disease surveillance.
Conclusion
This study reiterates the critical importance of timely detection and response to a zoonotic disease outbreak. Response to the first known anthrax outbreak in Kanungu District a border district experiencing a major public health threat of anthrax for the first time met only 1 (notification) of the 3 the 7-1-7 timeliness metrics owing to a real-time communication platform. There was delayed detection and response largely due to, low suspicion index among health workers and weak zoonotic disease surveillance. Application of the 7-1-7 framework this study enabled us highlight the missed windows of opportunity for early detection of zoonotic disease outbreaks in animals before humans are affected. Accordingly, the district health team (DHT) should strengthen One-Health and event-based surveillance in routine health service delivery in health facilities and at community level by improving support supervision. This could enhance early detection and response, averting human fatalities and economic losses.
Public health actions
Following our preliminary result dissemination, one implementing partner supported training of Over 500 VHTs Event Based Surveillance (EBS) at community level. Additionally, about 1000 teachers were sensitized about anthrax, and about 8,000 animals vaccinated against anthrax within the first 7 days of response initiation.
Acknowledgements
We acknowledge generous support and tireless dedication of the Kanungu District Local Government technical team specifically Frank Ilimaso (the district surveillance focal person) and Keneth Bejuna (veterinary surveillance focal person) for their dedicated support and guidance during the process of reaching different farms, health facilities, and communities to obtain information that led to the 7-1-7 assessment. We also acknowledge the district political leadership led by the Resident District Commissioner (RDC) who was also the head of the District Task Force (DTF). The RDC continuously supported risk communication and implementation of control measures that eventually led to the end of the outbreak. Special appreciation goes to Dr Scott Kellerman and the entire team at Bwindi Community Hospital, Buhoma for the time you dedicated to participate in this assessment, including availing your vehicle and fuel.
Conflict of Interest
The authors declared no conflict of Interest
Author Contribution
HK led the conception, design, analysis, and interpretation of the study results, and drafted the bulletin. HK, CM and BA participated in assessment, interpretation of results and review of the draft bulletin article. BMR and TA participated in the validation of the data obtained and interpretation of results. RM and HNN supervised the assessment and reviewed the bulletin for intellectual content, HTN, BK, SK, ARA reviewed the bulletin draft for intellectual content and scientific integrity.
Acknowledgements
We appreciate the technical support of the Uganda Public Health Fellowship Program.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source is however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Galante, D. and A. Fasanella. Anthrax in Animals. 2022 2022/07 [cited 2022; Available from: https://www.msdvetmanual.com/infectious-diseases/anthrax/anthrax-in-animals.
- Ario, A.R., et al., Uganda’s experience in establishing an electronic compendium for public health emergencies. PLOS Global Public Health, 2023. 3(2): p. e0001402.
- Kayiwa, J., et al., Establishing a public health emergency operations center in an outbreak-prone country: lessons learned in Uganda, January 2014 to December 2021. Health security, 2022. 20(5): p. 394-407.
- National Population Council, G.o.U., POPULATION GROWTH IN UGANDA: CHALLENGES AND OPPORTUNITIES. 2021, National Population Council, Government of Uganda Kampala, Uganda
- Kabasa, J.D., J. Kirsten, and I. Minde, Implications of changing agri-food system structure for agricultural education and training in Sub-Saharan Africa. Journal of Agribusiness in Developing and Emerging Economies, 2015. 5(2): p. 190-199.
- Faostat, F., New food balances. FAOSTAT. Available via FAO. Accessed, 2021. 25.
- Statistics, U.B.o., NATIONAL LIVESTOCK CENSUS 2021: MAIN REPORT. 2024, Government of Uganda: Kampala, Uganda.
- Bashaasha, B., et al., Uganda. 2013.
- Mbonye, A.K., et al., Ebola viral hemorrhagic disease outbreak in West Africa-lessons from Uganda. African health sciences, 2014. 14(3): p. 495-501.
- Buregyeya, E., et al., Operationalizing the one health approach in Uganda: challenges and opportunities. Journal of epidemiology and global health, 2020. 10(4): p. 250-257.
- Frieden, T.R., et al., 7-1-7: an organising principle, target, and accountability metric to make the world safer from pandemics. The Lancet, 2021. 398(10300): p. 638-640.
- Bochner, A.F., et al., Implementation of the 7-1-7 target for detection, notification, and response to public health threats in five countries: a retrospective, observational study. The Lancet Global Health, 2023. 11(6): p. e871-e879.
- Bush, L.M. and M.T. Vazquez-Pertejo. Anthrax. 2023 2023/03 [cited 2023; Available from: https://www.msdmanuals.com/professional/infectious-diseases/gram-positive-bacilli/anthrax.
- Medley, A.M., et al., Preventing the cross‐border spread of zoonotic diseases: Multisectoral community engagement to characterize animal mobility—Uganda, 2020. Zoonoses and public health, 2021. 68(7): p. 747-759.
- Nuwamanya, Y., et al., Anthrax outbreaks in western Uganda: The role of illegal meat dealers in spreading the infection, August 2022–April.
- Monje, F., et al., Animal Anthrax outbreak triggered by butchering infected carcasses on and or near the pastureland, Kween District, Uganda: January–December 2018.
- Monje, F., et al., Animal Anthrax outbreak caused by slaughtering infected carcasses on and or near the pastureland, Kiruhura District, Uganda, May-October 2018.
- Wafula, M.M., A. Patrick, and T. Charles, Managing the 2004/05 anthrax outbreak in queen elizabeth and lake mburo national parks, uganda. African Journal of Ecology, 2008. 46(1): p. 24-31.
- Nantima, N., et al., The importance of a One Health approach for prioritising zoonotic diseases to focus on capacity-building efforts in Uganda. Rev Sci Tech, 2019. 38(1): p. 315-25.
- Sekamatte, M., et al., Multisectoral prioritization of zoonotic diseases in Uganda, 2017: A One Health perspective. PloS one, 2018. 13(5): p. e0196799.
- Kungu, J.M., et al., Perceptions and practices towards anthrax in selected agricultural communities in Arua District, Uganda. Journal of Tropical Medicine, 2020. 2020(1): p. 9083615.
- Hamutyinei Dhliwayo, T., et al., Anthrax outbreak investigation in Tengwe, Mashonaland West Province, Zimbabwe, 2022. PLoS One, 2022. 17(12): p. e0278537.
- Hasahya, E., et al., Analysis of patterns of livestock movements in the Cattle Corridor of Uganda for risk-based surveillance of infectious diseases. Frontiers in Veterinary Science, 2023. 10: p. 1095293.
- Ilukor, J., et al. Analysis of veterinary service delivery in Uganda: an application of the process net-map tool. in Proceedings of the Tropentag 2012 conference: Resilience of agricultural systems against crises. 2012.
- Ilukor, J., et al., THE PROVISION OF VETERINARY SERVICES: WHO ARE THE INFLUENTIAL ACTORS AND WHAT ARE THE GOVERNANCE CHALLENGES? A CASE STUDY OF UGANDA. Experimental Agriculture, 2015. 51(3): p. 408-434.
- Kock, R., et al., A One-Health lens for anthrax. The Lancet Planetary Health, 2019. 3(7): p. e285-e286.
- Sanou, H., et al., How community-based health workers fulfil their roles in epidemic disease surveillance: a case study from Burkina Faso. BMC Health Services Research, 2024. 24(1): p. 1372.
- Walekhwa, A.W., et al., Strengthening anthrax outbreak response and preparedness: simulation and stakeholder education in Namisindwa district, Uganda. BMC Veterinary Research, 2024. 20(1): p. 484.


Comments are closed.