A point-source Cholera outbreak caused by drinking contaminated water from a fenced lakeshore water-collection site, Kasese district, June 2015
Authors: Pande Gerald1, Kwesiga Benon 1, Kihembo Christine1, Bwire Godfrey5, Ario Alex Riolexus1; Affiliations: 1Public Health Fellowship Program, 2Ministry of Health
On 20th June 2015, Kasese District reported a cholera outbreak in a fishing village that had affected >30 persons. We investigated this outbreak to identify the mode of transmission and to recommend control measures. This cholera out- break was caused by drinking water contaminated by feaces. At our recommendations, the village administrators rigorously disinfected all patients’ waste, fixed the tap-water system, provided water treatment tablets, and issued water- boiling advisory. The outbreak stopped one week afterwards
Introduction: Uganda documented the first cholera outbreak in 1971[1]. Since then, the country has experienced sporadic cases and localized cholera outbreaks, occasionally resulting in prolonged widespread cholera epidemics. The frequency of these reported cholera cases varies among districts in Uganda [2].The most at risk areas include the border areas neighboring the democratic republic of Congo (DRC), Sudan and
Kenya as well as urban slums in Kampala.
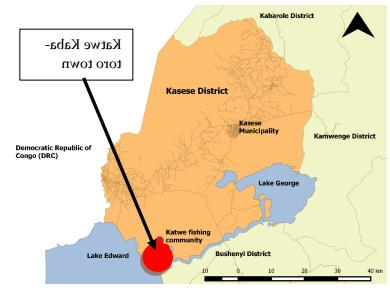
Methods: On 20th June2015 Kasese District reported a cholera outbreak affecting more than 30 people within five(5) days in Katwe-Kabatoro Town council, Kasese district. We conducted an investigation to establish the mode of transmission and to recommend evidence-based control measures.
Katwe Kabatoro Town Council is located in Busongora South County in Queen Elizabeth National Park, Kasese district. The study population consisted of community members in Kyarukara village in Katwe-Kabatoro Town council.
We defined a suspected cholera case as onset of acute watery diarrhea in a Katwe Kabatoro Town council resident from 01st June 2015 onward; a confirmed case was a suspected case with culture-confirmed Vibrio cholerae in a stool sample.
We actively identified cases by visiting affected community and up- dated line -lists obtained from the cholera treatment center. We assessed sources of water for drinking and for household use and assessed human waste disposal practices. We conducted descriptive analysis and interviewed 10 random case-patients on food and water exposures during the most likely exposure period.
Analytic study: In a case control study, we compared drinking water source points among 36 cases and 179 controls. Controls were asymptomatic Kyaruka village residents.
One case per household was selected using simple random sampling in instances where there was more than one case
Results: By 30th June 30, 2015, we had identified 61 suspected cases (attack rate=5.1%) with no death. The epidemic curve indicated an initial point-source outbreak followed by secondary transmission; after the primary cases onset on 16 June, cases rapidly increased and peaked on 19 June 2016 and rapidly declined afterwards; 8 scattered secondary cases occurred after 22 June 2016. Majority of cases
(40.7%) were below 9 years, 20.4% were 20 -29 years as shown in figure1. Katwe-Kabatooro is a fishing village with relatively few older persons living in the area. Therefore the low numbers in the older groups may not indicate low attack rates as shown in figure 3. The sex distribution of the cases showed that male (31) and female(30) residents of the village were equally affected. Of the five villages in the town council, Kyarukara was the most affected ( attack rate/1000 (AR) =20 compared to Kiganda ( AR=0.67) and Top hill (AR=0.36).
The primary case-person was a fisherman who between spent 15th and 16th June 2016 fishing on the lake. On 16th he developed acute diarrhoea and came ashore on 16th June 2016. He reported that he defecated near the fenced Water- Collection Site after returning. It is highly likely that he defecated into the fenced area. We hypothesized that the water from the caged collection site caused this outbreak by interviewing 10 random case-persons. We specifically interviewed study participants about their food and water history during the two days of most likely exposure.

We found that;
There had been no social gatherings between 15-17 June 2016 where people could have shared food or drink.
9 of the 10 case-persons reported that they usually collected water from a fenced water-collection site on the lakeshore and none of the 10 case-patients treated or boiled their drinking water.
Piped water supply in the town council broke down 8 months prior to this outbreak and people had resorted to spring water which is far off and expensive.
Food or water were possible sources in this point source out-break. We specifically interviewed study participants about their food and water history during the two days of most likely exposure.

Case control study findings: From the case-control study, 95% of case-persons, compared to 67% of the control-persons, usually collected their drinking water from the Kyarukara caged water collection site (ORM-H 9.3, 95% confidence Interval CI: 2.1-39).
Laboratory findings: Of the samples tested, 19 Rapid Diagnostic Tests (RDTs) were positive while 8 tested positive on stool culture.
Environmental findings: It was noted that village in the town council and observed that every village had a fenced water collection site which was constructed in or- der to protect the community member fetching water from crocodiles and hippopotamus as they draw water from the river. Kyarukara village had a very latrine coverage ( below 40%) with evidence of open defecation observed.
Discussion: The study showed that that drinking un- safe water (not boiled, treated or filtered) from Kyarukara fenced water collection site were much more likely to get infected. The population had resorted to the free unsafe lake water after main piped water system had broken down 8months prior to this outbreak.
Other alternative sources of drinking water were far off and much more costly. It should be noted that this out- break occurred amidst an ongoing cholera outbreak, sero-type Inaba, lasting 3 months and that had affected more than 80 other villages in Kasese District . This may explain the source of the outbreak. The affected community mainly depends on fishing and salt mining which subjects it to a lot of movement and interaction with other people during trade. Like several other cholera outbreaks, this out- break was caused by contamination of drinking water[3, 4]. It is possible that the primary case-person could have actually defecated into the fenced area and contaminated the water. Community members and local leaders also reported that the initial cases washed their clothes including soiled bed linen near the cage in Kyarukara. These clothes were not disinfected before washing and could have further contaminated the cage water.
Conclusions and recommendations: This was a point- source cholera outbreak was caused by drinking water contaminated with feaces from a fenced water collection site at Kyarukara village. At our recommendations, the town council administration rigorously disinfected all patients’ feaces at the cholera treatment center, fixed the tap-water system which had been dysfunctional, provided water treatment tablets, and issued water-boiling advisory. The outbreak stopped one week afterwards .


Comments are closed.