A measles outbreak propagated by children congregating at water collection points: Mayuge District, Uganda, October, 2016
Authors:Majwala Robert Kaos1*, Nakiire Lydia1, Kadobera Daniel1
Summary
On 12 October, 2016 a measles outbreak was reported in Mayuge district. We investigated the outbreak to determine its extent, risk factors, evaluate vaccination coverage and vaccine effectiveness, and recommend evidence-based control measures. Probable case was onset of fever (≥3 days) and generalized rash, plus ≥1 of the following: conjunctivitis, cough, runny nose in a resident of Mayuge. A confirmed case was a probable case with measles-specific IgM (+). We found cases by reviewing medical records and active community case-finding. A matched case-control was conducted to evaluated risk factors for transmission . We estimated vaccine effectiveness (VE) using the formula: VE≈100 (1-ORprotective) and calculated vaccination coverage using the per- cent of controls vaccinated. 62 probable cases were identified (attack rate [AR] = 4.0/10,000. Children <5 years (AR=14/10,000) were the most affected. 32% (13/41) of case-persons and 13% (21/161) of control-persons went to water-collection sites (by them- selves or with parents) during the case-patients’ likely exposure period (ORM-H=5.0; 95% CI=1.5–17). Among those aged 9 – 59 months, the effectiveness of the single-dose measles vaccine was 69% (95% CI=25-88); vaccination coverage was 68% (95% CI=61- 76). Exposures at water-collection sites might have contributed to propagation of this outbreak. Low vaccine effectiveness and vaccination coverage facilitated measles transmission. We recommended intensifying measles vaccination, advised residents with fever and rash to avoid going public gatherings including water-collection sites, and introducing a two-dose measles vaccine in routine vaccination schedule.
Introduction
Measles is one of the top five causes of vaccine preventable morbidity and mortality in the world [1] despite the availability of a safe and effective vaccine. Measles is an epidemic prone disease that has been targeted for eradication [2]. Measles surveillance is part of the National Integrated Dis- ease Surveillance and Response System, requiring immediate notification whenever measles is suspected [2] [3] . On 12 October, 2016, 3/10 samples from suspected measles case patients from Mayuge District tested positive for measles IgM antibodies. We investigated this outbreak to determine the extent, risk factors, vaccine effectiveness and coverage, and recommend evidence based control measures.
Methods
A Probable measles case-patient was someone presenting with fever of ≥3 days with a generalized muculopapular rash plus ≥1 of conjunctivitis, cough or running nose be- tween 19th June and 17th November, 2016.
A confirmed case was a probable case-patient with measles IgM (+). We reviewed health facility records and searched case-patients in the community, laboratory confirmation was done using WHO procedures [4].
Case control investigation involving participants from Kityerera and Malongo Sub-counties using face to face interviews with investigator administered questionnaires was conducted.
One case-patient per household was interviewed, households with more than one case-patient; the first to develop a measles rash was interviewed.
After interviewing a case- patient, 4 asymptomatic controls, matched by village and age were randomly selected and interviewed. District population estimates were extrapolated from the 2014 Uganda National Population census [5].
Vaccination coverage was computed from the vaccination coverage among controls and compared with district administrative coverage for a 3 year period (2014 – 2016).
Monthly measles data elements for period (2014 – 2016) were downloaded from DHIS 2,cumulative measles monthly coverage was computed and compared against monthly targets using Mayuge District population estimates obtained from Uganda National Population Census report 2016 [5].
We estimated Vaccine effectiveness (VE) for children ≤ 59 months using formula ; VE= 1-RR where Relative Risk (RR) approximates to Odds Ratio (OR) in rare diseases, hence VE = 1 – OR.
Findings
We found 62 case patients; Attack rate [AR] = 1.3 per 10,000. The most affected age groups were 0 – 11 months (AR = 13/10,000) and 12 – 59 months (AR = 15/10,000). Males had AR = 4.3/10,000 while females had AR = 3.9/10,000. Two sub counties were affected by this measles outbreak, Kityerera AR = 4.1/10,000 and Malongo AR = 4.0/10,000. The most affect- ed parish was Bumwena with AR = 79/10,000 followed by Kityerera with AR = 13/100,000.
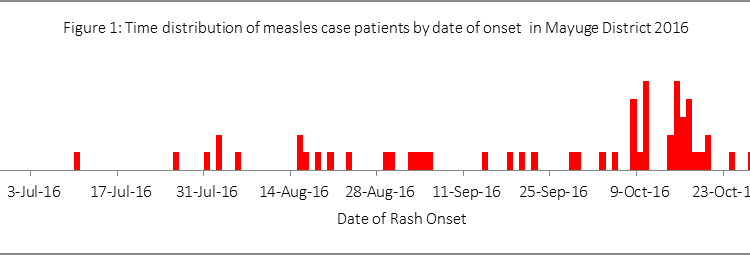
The epidemic curve (Figure 1) indicated features of person to person transmission. The index case patient in this outbreak had a rash onset date of 10th July, 2016 and the last case patient had rash onset date of 27th October; hence this measles out- break lasted 110 days. During interviews it was also found out that on 9th August, 2016 a lady travelled from a family that had recorded two measles case-patients of measles in Bumwena parish, Malongo sub-county to Kityerera Parish, Kityerera sub-county with two children aged 24 and 36 months, both non-vaccinated. After 7 days (16th August, 2016) the 36 months old baby developed a measles rash, and 11 days later (20th August, 2016) the younger sibling also developed a measles rash. A 9 year old child with whom they shared a homestead developed a measles rash on 23rd August, 2016 and was taken to the grandmother’s place for care. The homestead where the grand- mother stayed had 4 homes. This led to local transmission to 18 other children, with 83% of these aged between 0-59 months
About 39% (12/31) case patients’ aged 9 – 59 months were measles vaccine compared to 68% (82/121) controls of the same age group (odds ratio (ORMH), 0.31; 95% confidence interval (CI), 0.12 – 0.75). We found out that in this community, mothers of infants less than 6 months do not usually fetch water. Mothers of infants aged between 6 months to two years tend to carry their babies along as they go to fetch water from water collection points.
Children above 2 years escort their mothers, guardians or other siblings as they go to fetch water, often carrying age appropriate water collection vessels. We found that among children aged 6 – 59 months; approximately 32% (10/31) of case patients went to water collection points either alone, with their parents/guardians or with other children compared to 13% (16/121) of controls; ORMH 5.0; 95% CI = 1.5-17.
The Vaccine Effectiveness for children aged 9 – 59 months was 69%; 95% CI: (25 – 88). The vaccination coverage using controls from the case control investigation was 68% (95% CI: 61 – 76). In 2014 administrative measles vaccination coverage in the district was 86%, 75% in 2015 and by end of September 2016 vaccination coverage was 52%; against a cumulative target of 75%. By extrapolation, if no catch up vaccination had been implemented, by December 2016 vaccination coverage would have been 69%.
Discussion
Our investigation documents a propagated community measles outbreak that lasted 110 days with 62 case-patients, we were unable to identify the primary case-patient however the index case-patient was in Bumwena Parish, Malongo sub-county. It appears the index case patient transmitted the measles virus to the two other subsequent case patients since all of them developed disease within the incubation period for measles.
Similarly it appears two 2 children had exposure to measles from the household where they were staying in Bumwena Parish since this household had already recorded two measles case patients. Since the 36 month’s old child developed a measles rash 7 days after leaving the measles affected family in Bumwena Parish, it appears he had exposure in Bumwena.
However, the 24 month’s old child could have contracted the measles from his older sibling through person to person contact since they were staying in the same household or from Bumwena parish since the onset of the measles rash was 18 days from the time they left the measles affected family in Bumwena parish.
Measles transmission is through person to person, where a susceptible individual gets into contact with an infected individual, this may have been the case with the two siblings who had been staying in a measles affected family prior to moving to Kityerera Sub-county, additionally the 9 year old child who also got measles after staying in the same homestead with a measles case in Kityerera also supports this theory [6].
Vaccination coverage among controls in our investigation was estimated at 68%. This was nearly the same as the extrapolated administrative measles coverage of 69%. Low coverage creates a pool of susceptible individuals in the population, these susceptible individuals have been shown to cause outbreaks in populations with low measles vaccine coverage [7]. The coverage of 69% is far less than the 97% coverage that prevents measles outbreaks [8].
Vaccine effectiveness in our investigation was 75%. This was lower than the observed 85 – 94% in other settings studies for one dose measles vaccination [9]. Several factors affect vaccine effectiveness including age at vaccination, vaccine handling techniques, and quality of the cold chain.
Our investigation did not access these factors. A single measles vaccine administered at 12 months increases the vaccination effectiveness to about 92% compared to 85% when the measles vaccine is given at 9 months [9]. A two dose measles vaccine with one given at 9 and the other at about 12 months has been shown to increase vac- cine effectiveness to over 94% [9].
Our investigation further revealed that children congregating at water collection points were 5 times more likely to get measles than those who never went to collect water. When children get to water collection points, there is mixing between those with measles rash and health ones. Our findings are in agreement with studies done in The Republic the Marshall Islands and China that showed that congregate setting are associated with measles transmission [10] [11].
Conclusion
It appears exposures to infectious patients at water collection points propagated this measles outbreak. Low vaccination coverage coupled with low vaccine effectiveness facilitated community transmission of measles in Mayuge District.
Recommendations
We recommended supplementary measles vaccination for group of 0 – 59 months, introduction of a second measles vaccine, advised the community leaders and parents to discourage sick children from going to water collection points.
Public health actions
The district implemented daily vaccination at all health facilities, extra community outreach- es and mobile vaccination teams were established and implemented under the ‘periodic Intensified Immunizations (PIRI)’ project. Sensitization of residents to avoid public gatherings when they develop fever or fever and rash was also carried out.
References
- CDC: Vaccine preventable deaths and the Global Immunization Vision and Strategy, 2006-2015. MMWR 2006, 15(18):511-515.
- Uganda MoH: National Technical Guidelines for Integrated Disease Surveillance and Response. In. Kampala: Ministry of Health Uganda; 2012:
- WHO: Technical guidelines for integrated disease surveillance and response in the African Region. In., 2nd Edition edn: World Health Organization; 2010: 418.
- WHO: Manual for the Laboratory Diagnosis of Measles and Rubella Virus Infection. In., Second edition Geneva: World Health Organisation; 2007.
- UBOS: The National Population and Housing Census 2014 – Main Report, Kampala, Uganda. In. Kampala: Uganda Bureau of Statistics; 2016:
- Siegel JD, Rhinehart E, Jackson M, Chiarello L: 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Health Care Settings. American Journal of Infection Control, 35(10):S65-S164.


Comments are closed.